Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.16 no.4 Centurion nov./dic. 2017
http://dx.doi.org/10.17159/2309-8309/2017/v16n4a7
PAEDIATRICS
Intramedullary femoral lengthening with an 'unstable' hip without prior stabilisation: preliminary results of a case series
Laubscher MI; Mitchell CII; Timms AIII; Goodier DIV; Calder PV
IMBChB(UFS), Dip PEC, FC Orth(SA), MMed Ortho(UCT); Orthopaedic Surgeon; Orthopaedic Research Unit, Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
IIBP&O, BMBS; Senior House Officer, Orthopaedics; Limb Reconstruction Unit, Royal National Orthopaedic Hospital, Middlesex, United Kingdom
IIIBSc, RGN; Clinical Nurse Specialist; Limb Reconstruction Unit, Royal National Orthopaedic Hospital, Middlesex, United Kingdom
IVMBBS, FRCS(Eng), FRCS(Orth); Orthopaedic Surgeon; Limb Reconstruction Unit, Royal National Orthopaedic Hospital, Middlesex, United Kingdom
VMBBS, FRCSEng), FRCS(Orth); Orthopaedic Surgeon; Limb Reconstruction Unit, Royal National Orthopaedic Hospital, Middlesex, United Kingdom
ABSTRACT
BACKGROUND: Leg length discrepancy due to proximal migration of the femur commonly presents with a short leg gait and symptoms of hip and low back pain. The most common causes are chronic hip dislocation due to developmental dysplasia or the late sequelae of neonatal hip sepsis. It is usually recommended that the hip is stabilised prior to performing limb lengthening, and various techniques have been described. Unfortunately, these methods are not without complications, such as anatomical distortion making future arthroplasty more complex. We recognised a subgroup of these patients in whom the hip appeared unstable on plain film radiography, but in whom there was no proximal migration on weight bearing.
METHODS: We report on three of these patients who underwent limb lengthening with an intramedullary device, without prior stabilisation of the hip.
RESULTS: The desired length (range 55 to 60 mm) was achieved in all patients without further migration of the proximal femur. In all cases shoe raises were discontinued, and patient satisfaction was high. There was an improvement in gait in all patients.
CONCLUSION: Femoral lengthening is possible without prior stabilisation of the hip in certain so called 'unstable' hip situations. The proximal femoral anatomy is not further altered and future salvage procedures such as a total hip replacement are not compromised.
Level of evidence: Level 4
Key words: pelvic support, Ilizarov hip reconstruction, femoral lengthening, Precice
Introduction
Leg length discrepancy (LLD) due to proximal migration of the femur presents a treatment dilemma. The most common causes are the late sequelae of neonatal hip sepsis and chronic dislocation of the hip due to untreated developmental dysplasia (DDH). The patients present with a limp, with or without pain, and an LLD.1 Traditional teaching dictates that the hip should be stabilised prior to limb lengthening. Various techniques have been described, including the pelvic support osteotomy (PSO) and Ilizarov hip reconstruction. The PSO is a useful surgical procedure for the salvage of damaged hips of patients in whom arthrodesis or hip arthroplasty are not appropriate.2 Bodyweight is transferred to the femoral shaft through a proximal femoral valgus osteotomy abutting the ischial tuberosity.1Further proximal migration of the femur is prevented during weight bearing and a Trendelenburg limp is eliminated. It does however not address the LLD. Ilizarov3 added a second, more distal varus osteotomy to correct overall mechanical alignment and allow lengthening for leg length equalisation. Traditionally these surgeries were all performed with the use of either monolateral or circular external fixators.4 Subsequently these techniques have been further modified with the use of internal fixation for acute osteotomies and lengthening performed through an intramedullary lengthening nailing system.5,6
All these reconstructive options alter the shape of the proximal femur and complicate future salvage surgery, such as a total hip replacement (THR).7,8 Previous authors have described femoral lengthening without previous stabilisation of the hip with use of an external fixation system.9 There are many theoretical benefits to the patient undergoing limb lengthening using an intramedullary device compared to an external fixator.10 The Precice (Ellipse Technologies Inc, Irvine, California) Intramedullary Limb Lengthening System (ILLS) has added advantages including a variation in implant size and length with an ability to lengthen or shorten at an accurate rate.11 We retrospectively reviewed all femoral lengthenings performed in 'unstable' hip situations without prior hip stabilisation at our unit using the Precice ILLS.
Patients and methods
This study was subject to an institutional Research and Development (R&D) Department review (R&D registration number SE.14.038). Three patients, all female, with ages ranging from 12 to 24 years (median 16 years) constituted the cohort of this retrospective study. Inclusion criteria were an LLD secondary to proximal migration of the femur where femoral lengthening was performed without prior stabilisation of the hip. The diagnoses were absent femoral heads secondary to neonatal hip sepsis in two cases (Hunka 4b and 5)12 and chronic dislocation of the hip due to untreated developmental dysplasia of the hip (DDH) (Crowe IV) 13 in one case. All patients presented with a painless short leg gait and their goal was for leg length equalisation.
The characteristics and treatment of the study group are summarised in Table I.
Pre-operative evaluation
All cases were considered for a possible PSO prior to femoral lengthening. This included assessment of hip range of motion (especially maximal adduction). Leg length and single leg stance (flamingo view) radiographs were obtained. All patients demonstrated limited adduction clinically and minimal pelvic tilt seen radiographically in single leg stance (Figure 1). This led the senior authors to believe that the hips were indeed stable enough to withstand the forces of lengthening.

Procedure
Surgery was performed in all cases by the senior author (PC), a consultant limb reconstruction surgeon. A retrograde Precice intramedullary lengthening nail was inserted and a supracondylar femoral osteotomy performed for lengthening. The nails were inserted using the standard technique as advised by the manufacturers.14 All the osteotomies were pre-drilled and performed with a low energy technique15 at the distal metaphyseal-diaphyseal junction. No attempt was made to alter the mechanical axis, and the osteotomy was anatomically reduced when inserting the nail.
Post-operative management and follow-up
A latent period of six days was observed. Distraction was performed initially at a rate of 1 mm/day in three to four increments. Distraction was stopped or the rate lowered in cases with excessive pain or where adjacent joint contracture developed. The mean rate of lengthening was calculated as the total length achieved in millimetres divided by the number of days until lengthening was complete.
Patients were seen at two-weekly intervals with radiographs to monitor lengthening. Lengthening occurred along the anatomical axis of the femur as dictated by the intramedullary device. Once the desired length was achieved, follow-up intervals were increased to four weeks until union.
Patients initially attended out-patients' physiotherapy weekly to maintain hip and knee range of motion (ROM) and were provided with a daily home programme. The physiotherapy frequency was increased when ROM was lost. Patients were mobilised strictly non-weight bearing during the lengthening process. Once the desired length was achieved, patients were allowed to gradually increase their weight bearing over a four- to six-week period from non-weight bearing to full weight bearing based on the regenerate consolidation seen on the radiographs.
Data collection, evaluation at final follow-up and radiological assessment were performed by the first author (ML) who was not involved in the lengthenings. Radiographic union was defined on serial radiographs when corticalisation in the regenerate bone was observed in at least three cortices as previously described.16
Healing index (HI) was modified as suggested by previous authors10,17,18 as the period with the nail in situ (days) until adequate union was achieved that would allow removal of an external fixator. The presence of a nail in situ did not interfere with this evaluation.10,17
All complications and further re-operations were recorded from the hospital notes. At their latest follow-up, all cases were interviewed by one of the authors (ML) and asked to complete a simple questionnaire. Subjects were asked whether they felt subjectively that their gait improved, if they were able to abort their shoe raise and to indicate whether they would opt to have the treatment again if given the choice.
All patients underwent formal gait lab analysis post-operatively, as soon as it was possible for them to walk unaided with a normal gait pattern. An experienced technician performed gait lab analysis.
No statistical analysis was performed due to the small sample size.
Results
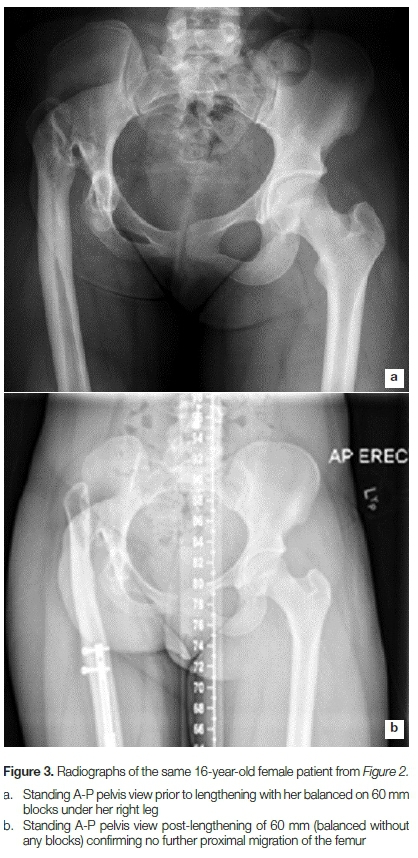
The desired length was obtained in all patients, in two patients 55 mm and the third 60 mm. The lengthening rate ranged from 0.66 to 0.95 mm/day. The modified HI calculated as described earlier ranged from 27.1 to 40.2 days/cm. There was no further proximal migration of the femur in any cases (Figures 2 and 3). The median length of latest follow-up was 18 months (range 15-20 months).
All three patients achieved their goal of leg length equalisation and were able to abandon their shoe raises. Gait improved subjectively in all three cases and all indicated that they would choose to have the treatment again in the same way if given the choice.
Formal gait lab analysis was performed in all three cases at a median of 3 months (range 3-4 months) following the completion of lengthening. The assessment revealed an improvement in gait pattern in all three cases. Gait analysis showed the short leg gait was eliminated in all patients.
We encountered a number of problems or complications. All three patients required reduction in the rate of lengthening due to thigh pain. Case no. 2 developed loss of flexion of her knee that resolved with inpatient physiotherapy alone and case no. 3 developed a fixed flexion deformity (FFD) of her knee that required a posterior release and inpatient physiotherapy to resolve. The same patient (case no. 3) developed a hip adduction contracture during lengthening that only resolved with inpatient physiotherapy. There were no implant complications such as backing out of locking bolts or nail breakage.10
Discussion
The PSO and Ilizarov hip reconstructions aim to eliminate a Trendelenburg and short leg gait by stabilising the proximal femur to preventing further proximal migration. For a PSO to be successful it is recommended that the hip is mobile or the femoral head absent.1During the planning for these reconstructions the leg is held in maximum adduction to determine the level of the proximal valgus and extension osteotomy where the femur is seen to abut the pelvis.2 It also eliminates further adduction that then prevents the pelvic drop during the stance phase of gait. In certain cases, however, no adduction is possible. If this is the case, surgical release with or without excision of the remaining femoral head and neck is advocated by some authors to allow adduction for the proximal osteotomy.1
A second, more distal varus osteotomy is then needed to correct the mechanical axis and allow lengthening of the limb. Placement of the hip or femoral shaft into adduction is therefore essential in order to follow the principles of these reconstructive procedures. In certain clinical scenarios adduction is limited, which prevents optimal position of a proximal femoral valgus osteotomy. The question is whether hip stability is provided by the abutment to the pelvis or whether the hip capsule and surrounding soft tissues provide enough support for distal lengthening. With no adduction allowing pelvic dip in single leg stance it may be proposed that hip stability is sufficient to allow lengthening of the femur to treat LLD in these cases.
The PSO and Ilizarov hip reconstruction should ideally be performed in adolescents. Indications include untreated or complicated DDH, early childhood hip sepsis, post-Girdlestone resection arthroplasty, traumatic hip instability and femoral neck pseudo-arthrosis, all in cases where hip arthrodesis or THR is not indicated or attractive.2 When a PSO is performed before the age of 12 years, the valgus remodels and a secondary procedure is required. A PSO is also less suitable for older patients, where it is advised to rather perform a THR.2 When a THR is performed in these situations, different surgical strategies can be followed. A high centre of rotation can be accepted and the acetabular component placed where the hip articulation is. This is however associated with altered biomechanics and early loosening.19 Alternatively the centre of rotation can be restored where the femur is shortened in the subtrochanteric region to allow the cup to be placed at the true acetabulum.20 Both these options do not restore leg length and the patient is left with a residual LLD. Lastly releases can be performed in an attempt to restore the centre of rotation and bring the proximal femur down to allow articulation at the true acetabulum. This however puts the sciatic nerve at risk, as the lengthening required is often more than the nerve can tolerate. Instability has also been described following this technique. All patients were skeletally mature on radiographs. Although one subject (case no. 2) was 12 years of age when we performed the surgery, her distal femoral physis was closed and she was classified as Risser stage 5 on pelvic radiograph. She was a child of an immigrant family and on closer interrogation it appeared that her age was not accurate due to late registration of her birth in her home country. A retrograde Precice nail would be contraindicated in a skeletally immature individual.
The PSO and Ilizarov hip reconstruction offers best value as a definitive procedure.21 Although it is said that it is possible to perform a THR following a PSO, the anatomy of the proximal femur is grossly distorted. THR following these reconstructions is associated with a high complication rate and even the need for early revision.8 If these patients develop hip symptoms in the future, we feel it is more likely plausible to perform a THR following Precice lengthening. Because the leg length has been restored, subtrochanteric shortening osteotomy can be performed to allow the hip centre of rotation to be restored without risking injury to the sciatic nerve.
Previous authors have also performed femoral lengthenings in these situations without prior stabilisation of hip.9 However, no mention is made of how cases where selected or which patients are suitable for this treatment option. That brings us to the question of whether these hips really are unstable. None of our patients developed hip symptoms during lengthening and there were no cases of proximal migration. The soft tissue problems we encountered were at the knee. This leads us to conclude that these hips have adequate 'stability' to prevent further proximal migrations and that a PSO prior to lengthening is therefore unnecessary. We feel that the pre-operative single leg stance radiograph (flamingo view) is important to aid in this assessment. If there is no adduction possible at the hip, the pelvis is prevented from dropping on the affected side.
Often there is an associated FFD of the hip joint as well as an external rotation deformity. During gait, anterior pelvic tilt is increased and the patient compensates through increasing lumbar lordosis which in turn can be responsible for lower back pain.
The PSO or Ilizarov hip reconstruction allows a simultaneous extension and rotational correction at the proximal osteotomy with that alleviates this. This was not possible in our series and FFD and external rotation deformities would remain. One patient (case no. 3) had a persistent external rotation deformity post-lengthening. We do feel that this could be addressed during future surgery, such as THR.
We encountered most complications in the patient (case no. 3) with a chronic high dislocation of the hip due to DDH. Although these cases of proximal migration of the femur present in a similar fashion, the underlying pathology would also influence outcome. Although we are unable to draw any significant conclusions due to our small numbers, we think that a high dislocation (secondary to DDH) might react differently than a complete absent hip from sepsis.
This is however a preliminary study with relatively short follow-up. We accept that hip instability can still develop post-lengthening at a later stage. Also at the time of writing none of the Precice nails had been removed as advised by the manufacturer. Late complications after removal of the device might still occur. Lastly, the study also involves small numbers, although due to the relative rarity of the treatment most studies on the topic are also limited to small numbers. Nevertheless, we believe our study is the first, to our knowledge, in which femoral lengthening is performed with a Precice nail in these 'unstable' hip situations without prior stabilisation.
To conclude we feel that femoral lengthening is possible in certain so-called 'unstable' hip situations without prior stabilisation of the hip. The proximal femoral anatomy is not further altered. We recommend watching them closely for soft tissue complications.
Acknowledgements
The authors would like to thank Matt Thornton for his assistance with the gait lab analysis of their cases.
Compliance with ethical standards
This study was subject to an institutional Research and Development (R&D) Department review (R&D registration number SE.14.038).
References
1. El-Rosasy MA, Ayoub MA. Midterm results of Ilizarov hip reconstruction for late sequelae of childhood septic arthritis. Strategies Trauma Limb Reconstr. 2014;9(3):149-55. [ Links ]
2. Pafilas D, Nayagam S. The pelvic support osteotomy: indications and preoperative planning. Strategies Trauma Limb Reconstr. 2008;3(2):83-92. [ Links ]
3. Mahran MA, Elgebeily MA, Ghaly NAM, Thakeb MF, Hefny HM. Pelvic support osteotomy by Ilizarov's concept: Is it a valuable option in managing neglected hip problems in adolescents and young adults? Strategies Trauma Limb Reconstr. 2011 ;6(1):13-20. [ Links ]
4. Mandar A, Tong X-B, Song S-H, et al. Pelvic support osteotomy for unstable hips using hybrid external fixator: case series and review of literature. J Orthop Sci. 2012;17(1):9-17. [ Links ]
5. Gursu S, Demir B, Yildirim T, Er T. An effective treatment for hip instabilities: pelvic support osteotomy and femoral lengthening. Acta Orthop Traumatol Turc. 2011;45(6):437-45. [ Links ]
6. Krieg AH, Lenze U, Hasler CC. Ilizarov hip reconstruction without external fixation: a new technique. J Child Orthop. 2010;4(3):259-66. [ Links ]
7. Emara KM. Pelvic support osteotomy in the treatment of patients with excision arthroplasty. Clin Orthop Relat Res. 2008;466(3):708-13. [ Links ]
8. Thabet AM, Catagni MA, Guerreschi F. Total hip replacement fifteen years after pelvic support osteotomy (PSO): a case report and review of the literature. Musculoskelet Surg. 2012;96(2):141 -47. [ Links ]
9. Cheng JC, Lam TP. Femoral lengthening after type IVB septic arthritis of the hip in children. J Pediatr Orthop. 1996;16(4):533-39. [ Links ]
10. Laubscher M, Mitchell C, Timms A, Goodier D, Calder P. Outcomes following femoral lengthening: An initial comparison of the Precice intramedullary lengthening nail and the LRS external fixator monorail system. Bone Joint J. 2016;98-B(10):1382-88. [ Links ]
11. Kirane YM, Fragomen AT, Rozbruch SR. Precision of the PRECICE internal bone lengthening nail. Clin Orthop Relat Res. 2014;472(12):3869-78. [ Links ]
12. Hunka L, Said SE, MacKenzie DA, Rogala EJ, Cruess RL. Classification and surgical management of the severe sequelae of septic hips in children. Clin Orthop Relat Res. 1982;(171):30-36. [ Links ]
13. Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15-23. [ Links ]
14. Rozbruch SR, Birch JG, Dahl MT, Herzenberg JE. Motorized Intramedullary Nail for Management of Limb-length Discrepancy and Deformity. J Am Acad Orthop Surg. 2014;22(7):403-409. [ Links ]
15. De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis). J Pediatr Orthop. 7(2):129-34. [ Links ]
16. Anand A, Feldman DS, Patel RJ, et al. Interobserver and intraobserver reliability of radiographic evidence of bone healing at osteotomy sites. J Pediatr Orthop B. 2006;15(4):271 -72. [ Links ]
17. Shabtai L, Specht SC, Standard SC, Herzenberg JE. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472(12):3860-68. [ Links ]
18. Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79(10):1464-80. [ Links ]
19. Kosuge D, Yamada N, Azegami S, Achan P, Ramachandran M. Management of developmental dysplasia of the hip in young adults: current concepts. Bone Joint J. 2013;95-B(6):732-37. [ Links ]
20. Charity JAF, Tsiridis E, Sheeraz A, et al. Treatment of Crowe IV high hip dysplasia with total hip replacement using the Exeter stem and shortening derotational subtrochanteric osteotomy. J Bone Joint Surg Br. 2011;93(1):34-38. [ Links ]
21. Manzotti A, Rovetta L, Pullen C, Catagni MA. Treatment of the late sequelae of septic arthritis of the hip. Clin Orthop Relat Res. 2003;(410):203-12. [ Links ]
 Correspondence:
Correspondence:
Dr Maritz Laubscher
Department of Orthopaedic Surgery, H49 OMB
Groote Schuur Hospital, University of Cape Town
Cape Town, 7925, South Africa
Email: maritzl@msn.com
Received: April 2017
Accepted: May 2017
Published: November 2017
Funding: The authors declare that no financial support was received for this study.
Editor: Prof Anton Schepers, University of the Witwatersrand
Conflict of interest: None of the authors reported a conflict of interest regarding this study. This study is not based on a previous communication.














