Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.16 no.3 Centurion Ago./Set. 2017
http://dx.doi.org/10.17159/2309-8309/2017/v16n3a9
UPPER LIMB
Standardised post-operative radiographs for volar radial plate fixation: the '22/11 X-ray'
W MattheeI; AJF RobertsonII; AD BarrowIII
IMBBCh, MRCS(Eng), FC (Ortho)SA, MMed(Ortho), Consultant Orthopaedic Surgeon in private practice, Gauteng
IIMBBCh, MMed(Ortho Surg), Consultant Orthopaedic Surgeon and Head of Clinical Unit (Paediatric Orthopaedics), Charlotte Maxeke Johannesburg Ac; Hospital, Department of Orthopaedic Surgery, University of the Witwatersrand
IIIMBBCh, FCS(Ortho), Consultant Orthopaedic Surgeon in private practice, Gauteng
ABSTRACT
BACKGROUND: The current standard post-operative radiographs for patients who have had volar locking plate fixation for a distal radius fracture may give the impression of intra-articular screw placement due to the normal anatomic inclination of the radiocarpal joint. Our aim was to determine: 1) if anatomically tilted post-operative radiographs increased the observer's confidence with regard to assessment of screw position, and 2) the intra- and inter-observer reliability of these radiographs.
METHODS: Thirty patients' standard and tilted (11 ° postero-anterior and 22° lateral) post-operative radiographs were assessed by an orthopaedic intern, registrar, consultant, and a radiologist on two occasions. Single and combined views were analysed.
RESULTS: There was no difference in confidence of assessment, but there was a significant change of assessment of actual screw position with fewer intra-articular penetrations reported with the tilted PA view. There was low intra-observer reliability except for the consultant orthopaedic surgeon. Inter-observer reliability was substantial when the intern's observations were excluded.
CONCLUSIONS: The routine acquisition of the tilted PA radiograph can assist senior health professionals with important patient management decisions.
LEVEL OF EVIDENCE: Level II.
Key words: anatomically tilted, radiographs, X-rays, distal radius, volar locking plate
Introduction
Distal radius fractures are common orthopaedic injuries, and fixation with an anatomically contoured volar locking plate is a treatment option.1 There are many different implants available, allowing for rigid fixation and early mobilisation of the wrist.2-4
Construct stiffness is increased when the screws are placed in the subchondral bone of the radio-carpal joint.5 Failure to correctly place the screws in subchondral bone may result in collapse of the distal fragments and malunion.2 However, penetration of the joint by one or more screws may produce pain and decreased function of the wrist, and predispose the patient to the development of osteoarthritis.
The anatomy of the distal radio-carpal joint has implications regarding radiographic assessment. The frontal plane inclination of the distal radius is 19° to 29° (mean 24°).6 The sagittal plane inclination of the distal radius is 2° to 20° (mean 11.45°), with women having a greater amount of palmar tilt than men.7 The operating surgeon typically screens the wrist at a number of different angles to check plate and screw position. Post-operatively and prior to discharge, however, formal radiographs at our institution are routinely taken perpendicular to the wrist joint. An observer may interpret the screws to be impinging the joint if they do not account for the volar tilt on the postero-anterior (PA) or the radial inclination on the lateral view (Figure 1). A report from a radiologist incorrectly concluding that several screws are penetrating the joint could cause frustration for the surgeon, confusion and alarm for the patient, and may have potential legal ramifications. In some hospitals, these films may be reviewed only by the attending intern or orthopaedic registrar before the patient is discharged and could lead to delays in discharge or the initiation of unnecessary investigations.

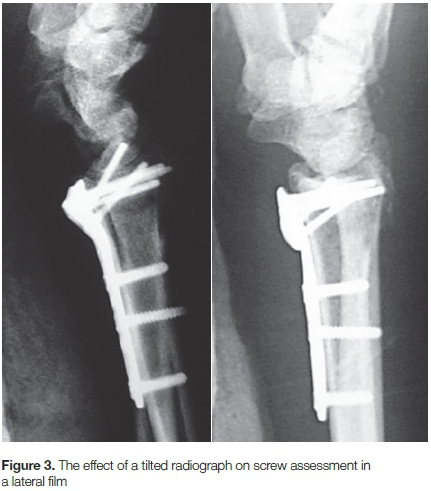
Tilted views tangential to the joint allow for evaluation of the radio-carpal joint without the overlying bone shadow of the radial styloid on the lateral view and the dorsal rim of the distal radius on the PA view (Figures 2 and 3). In many centres, there are no protocols for obtaining standardised anatomically tilted radiographs for patients who have undergone fixation of the distal radius. We hypothesise that such tilted views would improve post-operative interpretation of screw position for those involved in the patient's care but who are not dedicated hand surgeons, and should therefore be considered for routine acquisition.

Our research questions were:
1. Do anatomically tilted radiographs of the wrist improve the ability of observers with differing levels of orthopaedic knowledge and experience to confidently assess screw position with respect to the radio-carpal joint in patients undergoing volar locking plate fixation of the distal radius?
2. How good is the inter- and the intra-observer reliability of these radiographs?
Materials and methods
Approval was obtained from the Human Research Ethics Committee of the local university. This was a comparative study of a cohort of 30 sequential patients undergoing fixation of a distal radius fracture with a volar locking plate at three public teaching hospitals.
Inclusion criteria for the sample population were patients aged 18 years or older who consented to being involved in the study and were undergoing a primary open reduction and internal fixation (ORIF) of the distal radius with an anatomically contoured volar locking plate (irrespective of fracture type or plate used) within ten days of injury. Polytrauma patients were excluded as were those with confirmed or suspected pregnancy. There were no criteria pertaining to the operating surgeon's area of interest or level of experience.
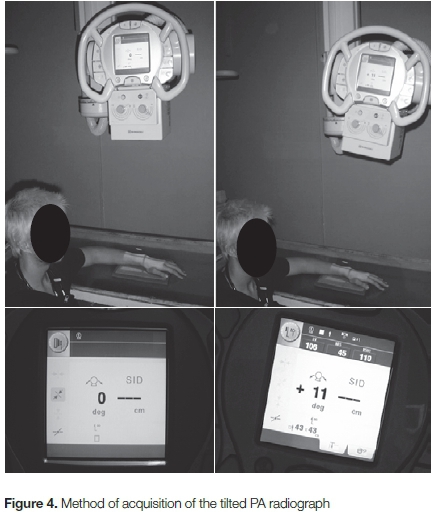
Our protocol is to apply a below-elbow volar plaster-of-Paris splint for the initial ten to 14 days post-operatively and thus all patients had radiographs taken with the splint in situ. The same model of X-ray machine was used at all three facilities and was equipped with a digital monitor which displayed the angle of tilt of the tube in one-degree increments.
A standard (PA) and lateral radiograph of the wrist was acquired, forming the control series of images. Additionally, a tilted PA radiograph was acquired with the wrist in neutral, palm down with the arm abducted to 90° and the elbow in 90° of flexion, and the X-ray tube was tilted by 11° from the normal vertical position, pointing towards the elbow (Figure 4). The tilted lateral radiograph was acquired with the wrist in a supinated position with the arm abducted to 90° and the elbow in 90° of flexion, and the X-ray tube was tilted to 22° from the normal vertical position, pointing towards the elbow (Figure 5).

All radiographs thus acquired were randomised using an online random number generator, and copied to a PowerPoint presentation (Microsoft Office 2010).8 The first 120 slides presented single views only (PA or lateral), and the remaining 60 slides were paired views (PA + lateral).
The slides were shown independently to four different observers who were not given any information as to the nature or purpose of the study. They were an intern in an orthopaedic rotation, a fourth-year orthopaedic registrar, a consultant orthopaedic surgeon who did not have a special interest in upper limb surgery, and a consultant radiologist who did not have a special interest in musculoskeletal radiology.
Each observer was asked: 'Can you tell with certainty where the screws are in relation to the wrist joint? (Y/N)'. If the answer to the question was 'Y', they were asked if they thought the screws were in the joint or not. A second observation was performed for each observer no earlier than four weeks later.
The data was converted to integer values for analysis. The first analysis pertained to the difference in confidence of assessment of screw position in relation to the wrist joint when comparing the tilted vs the normal radiographs for each of the observers on both occasions. The difference was calculated for each using the Fisher exact 1 -tail test using Statistica (Statsoft). A significant difference was regarded as a p-value of less than 0.05.
A second assessment of whether the observer thought that the screw was actually in the joint was calculated using the Pearson chi-squared test.
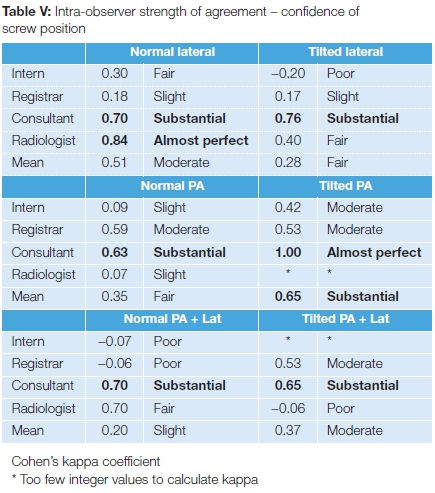
Intra-observer strength of agreement was calculated using Cohen's kappa coefficient with a 95% confidence interval, with strength of agreement being 'poor' for kappa < 0.00, 'slight' (0.00-0.20), 'fair' (0.21-0.40), 'moderate' (0.41-0.60), 'substantial' (0.61-0.80) and 'almost perfect' (0.81-1.00).9
Inter-observer reliability was calculated by using the Cohen's kappa coefficient to determine the strength of agreement between each of the four observers; and the mean coefficient was used as the final result for the group as a whole.
Results
Of the 30 patients, 15 were males and 15 female. There were 14 left and 16 right wrists. The mean age was 39.3 years (range 20-77 years). The mean time between injury and surgery was two days (range 0-9 days) and between surgery and the post-operative radiographs two days (1-18 days). The operating surgeons were consultants in three patients, registrars in 26, and a medical officer in one case. The implant used was the Aculoc plate from Acumed (Hillsboro, OR) in 25 patients, the DVR plate from DePuy (New Brunswick, NJ) in four, and one Synthes (Solothurn, Switzerland) locking plate. The mean time between the first and second observations was 11.4 weeks (4.5-29 weeks).
Regarding the confidence of assessment of screw position in relation to the wrist joint there was no significant difference seen in nearly all comparisons of tilted vs normal views on either occasion (Table I). With regard to assessment of actual screw position (Table II), there were several significant differences noted on both occasions for most observers for the tilted PA radiographs as well as the combined tilted PA + lateral compared to the standard views. No significant differences were demonstrated for the tilted lateral vs standard lateral radiographs.
Sub-analysis of PA films (Table III) demonstrated observers consistently reported fewer 'Yes' answers for joint impingement with tilted films compared to standard films (not significant). However, there were consistently more 'No' answers for joint impingement for all observers, and on both occasions for the tilted views, and this was found to be significant. Also, there was a consistent decrease among all observers in the 'Unsure' answers for the tilted PA compared to the normal view, and this was significant on the first observation, but not the second.
There were very low proportions of observers who initially reported 'No' joint penetration and then reported 'Yes' or 'Unsure' with the tilted PA films (Table IV). By comparison, there were higher proportions of observers who initially reported 'Yes' and subsequently changed their answer to 'No' or 'Unsure'.
Intra-observer reliability was noted to be 'substantial' or better only for the consultant for all films, and on both observations (Table V). For all other observers, the agreement was at best 'moderate'. For assessment of actual screw position, the agreement was again 'substantial' only for the consultant for all radiographs, with a mean kappa value of 0.722 (0.677-0.787) (Table VI). The mean value for the group of observers was not greater than 0.6 for any view.

Inter-observer analysis is detailed in Tables VII and VIII. Although there were some 'substantial' values between certain pairs of observers, the mean kappa value for all observers did not reach a value of 0.6 or higher on either observation even though in almost every instance, the mean values for the tilted radiographs were higher than those of the normal radiographs.
On sub-analysis of the tilted PA radiographs, if the intern's results were excluded, the mean kappa value for the first observation regarding confidence of assessment was 0.674 and for assessment of actual position was 0.704 and 0.652 for first and second observations respectively.
Discussion
The use of anatomically tilted radiographs in the management of distal radius fractures has been described previously and tilt images are well-known and accepted in terms of their improved imaging of the joint surface. Mekhail et al. used a 30° cephalad projection of a postero-anterior wrist radiograph allowing better fracture assessment, especially of the dorsomedial fragment of the lunate fossa in a die-punch fracture.10 Lundy et al. suggested that the 22° lateral view may help better understanding of the intra-articular depression of lunate facet fractures and aid in the subsequent fracture reduction and fixation.11 Johnson and Szabo recommended tilted lateral views for better assessment especially when there was significant dorsal angulation.12 Yi et al. studied the use of anatomically tilted lateral radiographs on the determination of the restoration of normal volar tilt, finding moderate to excellent reliability but no statistically significant differences compared with standard lateral radiographs.13
It should be emphasised that this study did not attempt in any way to determine the diagnostic usefulness of tilted radiographs for joint penetration and thus no 'gold-standard' was applied for comparison. It was assumed that most, if not all, implants had been checked at multiple angles by the operating surgeon intra-operatively and were known to be extra-articular. It may be standard practice in some centres to use fluoroscopy as the definitive imaging modality without formal radiographs, especially in institutions where such fractures are treated exclusively by specialist hand surgeons, but this is not universal practice.14
We could find only one study in the literature evaluating the assessment of anatomically tilted radiographs of the distal radius in living patients to compare to this study. Kumar et al. studied a series of ten patients undergoing volar plate fixation. The screws appeared intra-articular in all ten patients on the standard antero-posterior view, and in eight patients on the standard lateral.15 The tangential views, however, resulted in no screws seen to be penetrating the joint. They did not standardise the degrees of tilt, but gave ranges of 10° to 15° in the fully pronated position, and 20° to 25° in the lateral position. They obtained this tilt by lifting the arm off the table, but give no indication as to how this position was maintained.
The use of cadavers allows for direct joint assessment and thus permits calculations of diagnostic accuracy, but cadaveric studies of this area of interest typically do not include in their design fixation of actual fractures. In practical clinical situations, postoperative radiographs are often acquired with a plaster or fibre-glass splint; and fracture lines, joint disruption and soft-tissue swelling may all contribute to make accurate interpretation challenging.
Boyer et al. evaluated tilted radiographs for diagnosing joint penetration using dorsal plates in cadaveric specimens, comparing radiographic results with arthrotomy for evaluation of joint penetration.16 Tilted radiographs (PA: 11°; lateral: 23°), were taken using a tilted radiolucent table. The tilted lateral view improved the sensitivity and specificity over the standard lateral view, but there was a false positive rate of 17%.
The tilted PA view did not increase the sensitivity or specificity of intra-articular screw placement over the standard PA view. Radiographs were examined on two separate occasions -observers were first presented with one view at a time, and two weeks later were presented with paired views. There was no meaningful improvement in the sensitivity and specificity of intra-articular screw detection with the combined tilted views compared to the combined standard views. It was not reported who the observers were.
Tweet et al. intentionally penetrated the radiocarpal joint in 15 out of 30 cadaveric specimens.14 Tilted imaging of 11° and 22° were shown to five blinded observers, as well as two 360° rotational fluoroscopy movies. The rotational fluoroscopy provided the highest sensitivity (93%) and specificity (96%) for detection of joint penetration and was more reliable than most images (standard or tilted). They also noted that of 696 respondents who are active members of the American Society for Surgery of the Hand, 606 (87%) use only fluoroscopic imaging to detect intra-articular screw penetration without acquiring cassette radiographs post-operatively.
Soong et al. reported on multiple anatomically tilted radiographs using one type of volar locking plate in cadaveric specimens.17 The accuracy of the radiographs in confirming screw position was determined by arthrotomy. They used a goniometer to tilt the forearm at the required angles (15°, 23°, 30° tilted laterals, and 11° tilted PA). They determined that a screw was extra-articular if no part extended beyond the thick shadow of subchondral bone. They reported that the low-angle lateral anatomic tilt views (15° and 23°) were more specific to exclude intra-articular screw placement of screws placed on the ulnar side of the radius, whereas the specificity of the radially placed screws increased with the high-angle lateral anatmomic tilt views (30°). This is especially true for screws placed in the styloid process. Thus it may be appropriate to place the screws on the ulnar side first, followed by the more radially placed screws.
There are few reports in the literature concerning variability assessment between observers. Our finding of poor inter-observer reliability was almost certainly as a direct result of the poor intra-observer reliability recorded. Though not significant there was a noticeable tendency towards improved confidence for the intern between observations, possibly as a result of their time spent in the orthopaedic rotation. It is also noted that the Cohen's kappa coefficients for the radiologist and intern in particular varied quite substantially between observations - the reason for this is unclear.
Yi et al. performed a retrospective analysis of 20 patients who had distal radius volar plate fixation, and compared results with 20 controls.13 They used a 23° tilted lateral radiograph of the wrist, and measured intra- and inter-observer variability in the measurement of volar angulation between a specialist orthopaedic hand surgeon, a specialist hand fellow, and a senior orthopaedic registrar. Intra-observer reliability was excellent for the tilted lateral radiographs compared to the standard films for both patients and controls, especially for the more senior observers. Inter-observer reliability was excellent for the tilted films, but only moderate for the standard X-ray. Their data agrees with our results in that the intra-observer agreement is substantial at the level of the orthopaedic consultant.
Boyer et al. also examined inter-observer reliability for screw penetration.16 Reliability was significantly improved for the anatomically tilted lateral views compared to the standard lateral view. Improvement in reliability was also noted with the tilted PA views compared to the normal PA views. No change was seen in the comparison of combined tilted PA and lateral views with combined normal PA and lateral.
Alternative described methods of obtaining anatomically tilted radiographs of the wrist joint include lifting the arm off the radiolucent table to the desired angle, the use of a radiolucent bolster angled at a specific degree, and tilting the table on which the forearm rests and using a goniometer to confirm the angle of tilt.11,15,16,18 The method in this study - tilting the X-ray tube to the desired angle - is advantageous in that the patient does not need to be re-positioned between the standard and tilted PA films, and no extra equipment is needed.
The question remains whether these tilted radiographs should be requested routinely in these cases. In this study only the tilted PA view appeared to improve interpretation for 'non-expert' observers. The use of only one additional radiograph in the routine series requires very little extra cost, time, effort or training to acquire. The extra radiation exposure would be small by comparison to a CT or repeated, non-standard radiographs for cases of concern. Therefore, we support its routine acquisition in addition to the standard PA and lateral radiographs.
Potential limitations of the study are the chosen angles of 11° and 22° for the tilted films. The angles were chosen as they represent an estimation of the mean range in a given population, and are easy to remember and apply - trainees are often taught the 'rule of 11s' for the radiographic assessment of acceptable fracture reduction of the distal radius.
The actual curvature of the joint in the coronal as well as the sagittal planes needs to be taken into consideration. Due to this curvature, it may not be possible to obtain a single radiograph at any one angle that can exclude all possibilities of intra-articular screw placement.17
We used modern digital X-ray machines capable of accurately setting the amount of tilt in one-degree increments, but this may not be the case in hospitals having older X-ray machines with far less accurate, mechanical calibration devices used to set the tilt, usually in two- or five-degree increments.
Another potential limitation is that it is assumed that the operating surgeon has reduced the fracture anatomically. If not, the normal inclination of the radius may not have been restored, and the degree of tilt for the tilted radiographs would not therefore not be suitable. The fracture type as well as the specific implant used may also affect the radiographic interpretation.
The four observers in this study were chosen because they each represent a different level of orthopaedic knowledge and experience, and different results may have been obtained with different observers or different groups of observers.
Conclusions
We find that the use of standardised anatomically tilted radiographs of the wrist did not change the observer's subjective confidence of assessment with respect to intra-articular impingement. However, the tilted PA view did result in fewer reports of joint penetration, as well as less uncertainty regarding intra-articular screw placement, and the routine acquisition of this radiograph for interpretation by senior medical professionals may aid in further patient management decisions. However, the intra-observer reliability of these radiographs was poor for trainees and non-orthopaedic personnel, and this resulted in poor inter-observer reliability.
Compliance with ethics guidelines
Approval was obtained from the Human Research Ethics Committee of the local university.
The authors confirm that this is entirely their own work, and it has not been published elsewhere.
References
1. Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006;88(12):2687-94. [ Links ]
2. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27(2):205-15. [ Links ]
3. Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006;31 (3):359-65. [ Links ]
4. Willis AA, Kutsumi K, Zobitz ME, Cooney WP. Internal fixation of dorsally displaced fractures of the distal part of the radius. A bio-mechanical analysis of volar plate fracture stability. J Bone Joint Surg Am. 2006;88(11):2411-17. [ Links ]
5. Drobetz H, Bryant AL, Pokorny T, Spitaler R, Leixnering M, Jupiter JB. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction-a biomechanic study in a cadaveric model. J Hand Surg Am. 2006;31 (4):615-22. [ Links ]
6. Schuind FA, Linscheid RL, An KN, Chao EY. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am. 1992;74(9):1418-29. [ Links ]
7. Mann FA, Kang SW, Gilula LA. Normal palmar tilt: is dorsal tilting really normal? J Hand Surg Br. 1992;17(3):315-1 7. [ Links ]
8. RANDOM.ORG. [Online]. [cited 2013 03 25]. Available from: http://www.random.org/sequences/. [ Links ]
9. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74. [ Links ]
10. Mekhail AO, Ebraheim NA, McCreath WA, Jackson WT, Yeasting RA. Anatomic and X-ray film studies of the distal articular surface of the radius. J Hand Surg Am. 1996;21 (4):567-73. [ Links ]
11. Lundy DW, Quisling SG, Lourie GM, Feiner CM, Lins RE. Tilted lateral radiographs in the evaluation of intra-articular distal radius fractures. J Hand Surg Am. 1999; 24(2):249-56. [ Links ]
12. Johnson PG, Szabo RM. Angle measurements of the distal radius: a cadaver study. Skeletal Radiol. 1993;22(4):243-46. [ Links ]
13. Yi JW, Kim RG, Choi JH, Kim JK. Use of standard and anatomic-tilt lateral X-rays to determine distal radius volar angulation. J Hand Surg Am. 2012;37(4): 736-40. [ Links ]
14. Tweet ML, Calfee RP, Stern PJ. Rotational fluoroscopy assists in detection of intra-articular screw penetration during volar plating of the distal radius. J Hand Surg Am. 2010 Apr;35(4):619-27. [ Links ]
15. Kumar D, Breakwell L, Desmukh SC, Singh BK. Tangential views of the articular surface of the distal radius-aid to open reduction and internal fixation of fractures. Injury. 2001 ;32(10):783-86. [ Links ]
16. Boyer MI, Korcek KJ, Gelberman RH, Gilula LA, Ditsios K, Evanoff BA. Anatomic tilt x-rays of the distal radius: an ex vivo analysis of surgical fixation. J Hand Surg Am. 2004;29(1):116-22. [ Links ]
17. Soong M, Got C, Katarincic J, Akelman E. Fluoroscopic evaluation of intra-articular screw placement during locked volar plating of the distal radius: a cadaveric study. J Hand Surg Am. 2008;33(10):1720-23. [ Links ]
18. Melton JT, Southgate JJ. Modified lateral radiograph for assessment of the radiocarpal joint following palmar plating of the distal radius. J Hand Surg Eur Vol. 2009;34(2):274-75. [ Links ]
 Correspondence:
Correspondence:
Dr W Matthee
Waterfall City Hospital, Room GF15
Cnr Magwa Crescent and Mac Mac Avenue1652
Midrand, Tel: +2711 304 6784, Fax: +2711 304 7705
Email: warren.matthee@drmatthee.com
Editor: Prof Anton Schepers, University of the Witwatersrand Received: August 2016 Accepted: May 2017 Published: August 2017
Funding: No external funding was received for this study.
Conflict of interest: The authors certify they have no affiliations with or involvement in any organisation or entity with any financial interest, or non-financial interest, in the sunject matter or materials discussed in this manuscript.














