Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.16 n.1 Centurion Feb./Mar. 2017
http://dx.doi.org/10.17159/2309-8309/2017/v16n1a9
UPPER LIMB
Clinical outcomes following reduction and pinning of lesser arc injuries without repair of the scapholunate interosseous ligament
TL HiltonI; D ChiversII; M HeldIII; M SolomonsIV; M MareeV
IMBChB(UCT), DA(SA), DipPEC(SA); Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
IIMBChB(Wits); Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
IIIFC Orth(SA), MMed(Ortho); Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
IVMBChB(UCT), FCS(Orth); Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
VMBChB(UCT), FCS(Orth); Department of Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
ABSTRACT
BACKGROUND: Purely ligamentous lesser arc, Mayfield grade 3 and 4, perilunate dislocations (PLDs) are uncommon. Current recommendations are for open reduction and repair of the interosseous ligaments to prevent the development of scapholunate dissociation and degeneration to a scapholunate advance collapse (SLAC) wrist. This study proposes a less invasive treatment method which includes closed reduction and pinning alone without repair of the scapholunate interosseous ligament. We propose that most patients will obtain good function and pain scores and the few that develop instability may still have a reconstruction performed through a naïve surgical field
METHODS: Dislocations were reduced anatomically and held with buried K-wires which were removed at 6 weeks with no specific rehabilitation protocol observed. Subjective assessment included Mayo wrist scoring system, wrist range of movement, instability and grip strength testing. Radiological measurements included scapholunate distance, scapholunate angle, radiolunate angle and osteoarthritis
RESULTS: Ten male patients, median age of 35 years, were followed up for a median of 22 months. Seven patients underwent a closed reduction and anatomical pinning while three underwent open reduction due to unachievable reduction by closed means. All of these patients presented at a median of 14 days after the injury occurred. None of the patients had their scapholunate ligaments repaired or reconstructed. Mayo scores included three excellent scores, two good scores and five fair scores. Instability was found clinically in one asymptomatic patient who had a positive Watson shift test. Radiological scores include a median scapholunate distance of 2 mm, a scapholunate angle of 70° and a radiolunate angle of 15°. Osteoarthritis was found in two patients, all of whom were asymptomatic
DISCUSSION: Current recommendations in the literature are that PLDs should be reduced via an open surgical technique with repair of the scapholunate interosseous ligament (SLIL) and percutaneous pinning. However, the results of this treatment strategy are not optimal and do not confer uniformly good results. We propose a closed anatomical reduction and percutaneous pinning of the PLD. Our study shows that most patients will demonstrate good function and pain scores when managed this way. A smaller number of these injured wrists will go on to develop instability. However, the advantage of our method over the current recommendations is that when this happens the reconstruction of the SLIL will be made easier through a naïve surgical field
CONCLUSION: We recommend the closed reduction and anatomical pinning of a purely ligamentous lesser arc injury. This treatment strategy yields good results at medium term follow-up and preserves the option for the reconstruction of the scapholunate interosseous ligament should instability develop
Key words: perilunate dislocation, carpal instability, scapholunate, DISI
Introduction
Purely ligamentous lesser arc Mayfield type 3 and 4 injuries, i.e. perilunate and lunate dislocations, are uncommon. The scapholunate interosseous ligament (SLIL) is always involved in this injury. Historically, closed reduction and plaster casting of lesser arc injuries yielded poor outcomes.1-3 Current approaches favour operative treatment with open reduction, internal stabilisation and repair of the important interosseous ligament.3-10 SLIL repair is thought to be critical to prevent carpal instability and post-traumatic osteoarthritis. However, some studies have shown that despite careful reduction of the wrist and repair of the SLIL, a high percentage still go on to develop abnormal radiological parameters and instability.11 We feel that an open reduction, internal fixation and repair of the SLIL is unnecessary in the acute stage of this injury. We hypothesise that a less invasive approach to the early treatment of these injuries will have good medium-term results in the majority of patients while minimising further trauma, while still preserving the ability to perform more extensive surgery should instability develop.
Methods and materials
Following research ethics approval, a retrospective folder review of patients referred with acute hand and wrist trauma from 2011 to 2014 was performed. All patients were treated at a tertiary level, university hospital. Ten consecutive patients with purely ligamentous lesser arc Mayfield type 3 and 4 injuries, i.e. dorsal perilunate and volar lunate dislocations, were identified. Surgery was performed on the day of presentation under regional intravenous or brachial block anaesthesia. All reductions were initially attempted closed. If closed wrist reduction failed, open reduction was performed. Surgery was performed by the on-call hand surgery registrar with a consultant present. If senior cover was not available to perform the accurate reduction and wiring at the initial surgery, the wrist reduction was performed only. The definitive surgery, i.e. accurate scapholunate (SL) reduction and wiring, was performed on the next available list. If closed reduction was not possible immediately, the patient was splinted and the reduction and definitive surgery performed the following day by the senior hand surgeon on duty. We found this to be the case only in injuries that presented late to the unit.
Method of reduction
Perilunate and lunate dislocations were reduced closed using Tavernier's manoeuvre.12 The technique used by the unit to perform an accurate and anatomic closed reduction was by one of two ways. If two surgeons were present, a percutaneous joystick manoeuvre, as described in Green's Operative Hand Surgery,13was used. If a single surgeon was present, the lunate was manipulated to be co-linear with the capitate and radius and temporarily held with a smooth 1 mm or 1.2 mm K-wire from the radius to the lunate.
The wrist was then gently extended and ulnar deviated to reduce the flexed scaphoid and close the scapholunate (SL) gap. The definitive fixation was performed in a manner described below. We found the lunotriquetral (LT) joint to reduce anatomically once the lunate had been reduced. Thus, it was not specifically repaired or wired, as it was not deemed that additional stabilisation was required. We feel that most clinicians managing these injuries acknowledge that SLIL and the development of scapholunate advanced collapse (SLAC) is the major concern rather than problems with the ulna side of the wrist.
If closed wrist reduction was not possible, open reduction was performed through a dorsal approach described by Berger et al.14between the third and fourth extensor compartments. Extensor pollicis longus (EPL) was released and a radially based capsular flap created, preserving the radiotri-quetral ligament. All cartilaginous debris was removed and any cartilaginous damage to the scaphoid and capitate noted. An anatomic reduction was achieved of both the SL and LT articulations and the reduction was held in the same manner as described below. No attempt was made to repair the SLIL or the LT ligament.
It was imperative that an anatomical reduction of the SL and LT articulation was achieved and confirmed with intraoperative screening. An SL gap less than 2 mm, an SL angle between 30° and 60° and a radiolunate angle of less than 10° was accepted as reduced.
The radial sensory nerve was protected by blunt dissection down to styloid. Two smooth percutaneous 1.6 mm K-wires were placed just distal to the radial styloid, one from the scaphoid into the lunate to maintain the scapholunate reduction and one from the scaphoid into the capitate to prevent scaphoid flexion. The wires were cut short and buried beneath the skin. No wires were inserted from the triquetrum to the lunate.
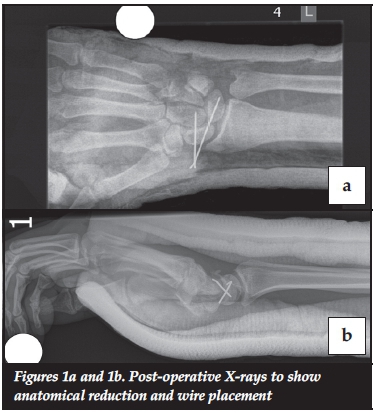
All patients were placed in a below-elbow thumb SPICA plaster in approximately 10 degrees of wrist flexion, for 6 weeks after which the plaster and wires were removed in theatre under local anaesthesia. Patients were referred to the physiotherapy service to regain wrist motion, but with no structured rehabilitation or post-operative splinting protocol (Figures 1 and 2).

Follow-up and long-term assessment
At the follow-up visits patients underwent subjective and objective clinical and radiological assessment. A subjective clinical assessment included perception of pain and return to function in terms of work and sport. The objective clinical assessment included tests for carpal instability, wrist range of movement and grip strength. The finger extension test and Watson shift test were used to assess for carpal instability. Wrist flexion and extension of the injured and uninjured side was measured using a hand-held goniometer. Grip strength was measured in kilograms using the Jamar® Hydraulic Hand Dynamometer. To measure grip strength the patient was seated with the elbow flexed to 90 degrees, arm adducted and forearm in neutral. Three readings were recorded, alternating with the normal side to prevent fatigue. The Mayo Wrist Score was calculated in order to quantify the functional outcomes of this treatment method and as a method for comparison between patient groups, i.e. open versus closed wrist reduction and between the groups who underwent two assessments.
Radiographic investigation included a clenched fist, neutral posterior-anterior (PA) and a lateral view of the wrist. The scapholunate angle (SLA), scapholunate distance (SLD) and radiolunate angle (RLA) were measured using the digital measuring tools available with the Phillips iSite Enterprise radiology software. The presence of osteoarthritic changes of the radiocarpal and mid-carpal joints were also recorded. The senior author, using the same radiographic landmarks, performed all measurements. SL distance was measured as the distance between the scaphoid cortex and the lunate cortex at the centre of the scapholunate joint.15 The SLA was measured between the longitudinal axis of the lunate (drawn perpendicular to a line joining the dorsal and volar poles of the lunate) and a line intersecting the volar cortices of the proximal and distance convexities.16
Statistical methods
Subject characteristics were summarised using descriptive statistics; for continuous variables, means and standard deviations are reported, and for categorical variables, counts and percentages are reported. Despite the small number of study subjects, the normality of the distribution of continuous data was assessed using the Shapiro Wilk Test. Normally distributed data was summarised using means and standard deviations, and the means compared in the two groups using the Student's t-test. Skewed data was summarised using the median and range, and the medians were compared using the Wilcoxon Rank-Sum/Mann Whitney U-test. The level of statistical significance was set at p<0.05.
Results
The patient cohort included ten patients with a median age of 35 years (min 18, max 53), all were male and all were right-hand dominant. In five (50%) patients, the right hand was injured. Six patients (60%) sustained their injury from a fall from a height while the remainder were motor vehicle injuries.
Of the ten patients, seven presented immediately after their injury and underwent successful closed reduction and anatomical wiring. Three patients proceeded to open reduction after closed attempts failed and all three were found to have intra-substance tears intra-operatively. Of the three that required open reduction there was a significant delay to presentation and therefore surgery at a median of 14 days (min 14, max 21). All ten patients returned at 6 weeks for removal of plaster and removal of wires. At final follow-up one of the ten patients' X-rays were not available for analysis and this patient was excluded from the radiological assessment.
Table I reflects the entire cohort at final follow-up, median of 22 months (min 4, max 30). Nine of the ten patients reported no pain with one patient reporting only mild, occasional pain. This was reflected in the Mayo score that showed an excellent score in three patients (30%), good in two (20%) and fair in five (50%). Sixty per cent of patients returned to work, while 20% were unemployed at time of follow-up but found work subsequently. Only 20% did not return to work and this was due to other injuries sustained.

One of the ten patients had a positive Watson Scaphoid Shift test but was asymptomatic. No patients had a positive finger extension test. The wrist range of movement and grip strength of the total group, for the injured side, was 76% and 90% respectively compared to the normal side.
The good clinical instability scores were in contrast to the radiological variables with none being in the range that the study deemed acceptable at final follow-up. Again, the small numbers prevented significant statistical correlation; however, the poor radiological scores did not correlate with poor clinical scores. Two of the nine patients showed arthritic changes on X-ray at final follow-up but experienced no pain clinically.
There were no post-operative complications such as sepsis, broken metalware or arthrofibrosis.
Discussion
There is currently no disagreement in the literature concerning the importance of the scapholunate relationship in wrist biomechanics and whether accurate reduction of the carpus is imperative to favourable longterm outcome in PLDs.11,17-20 However there is controversy as to whether to achieve reduction via open or closed means and how to maintain the scapholunate relationship. There is no clear evidence to suggest that open reduction and acute repair of the SLIL is advantageous to closed reduction and pinning alone. Currently there is only one small study by Inoue and Kuwahata21 of 14 patients, that compares closed reduction and pinning to open reduction, SLIL repair and pinning. In this study no statistical difference in outcome between these two groups was found.21
Open treatment, including ligament repair, is aimed at preventing scapholunate advanced collapse, i.e. the SLAC wrist. The SLAC wrist is seen with acceleration of the post-traumatic osteoarthritis and wrist instability found with conservative treatment at long-term follow-up. However, when looking at whether or not an open reduction and internal fixation, without repair of the SLIL, is beneficial to a good radiological score and functional outcome, a study by Forli et al.11has the longest follow-up with an average of 13 years (range, 10-25). They conclude that there is a tendency for patients to show degenerative changes on X-ray with time and that good reduction, not necessarily the SLIL repair, results in a better radiological score. They also state that poor reduction results in worse degenerative changes; however, that this does not seem to translate into a poor functional outcome.11 In our study we achieved anatomic reduction in seven of ten patients with closed manipulation, which is comparable to that of Adkison et al.3Of these, only one patient showed signs of osteoarthritis on X-ray follow-up and scored fair on the Mayo score with no pain, full range of movement and grip strength 93% compared to the uninjured side.
Open treatment of PLDs using dorsal or dorsal and volar combined incisions, for reduction and ligament repair have also shown poor results.7,22,23 Hildebrand et al.24 performed an open reduction through a combined dorsal and volar approach on a mixed cohort of patients who sustained both PLDs and perilunate fracture dislocations (PLFDs).24 Despite good Mayo scores and wrist range of movement they reported high complication rates and poor patient satisfaction. Trumble et al.25 described combined dorsal and volar approach with repair of the SLIL, protected by a looped interosseous cerclage wire, to give better compression across the SL interval compared to K-wires.25 This study reported good range of movement and grip strength when compared to the contralateral side and no deterioration of the SL gap or angle over time, in keeping with the work of Forli et al.11Unfortunately outcomes such as pain, instability or the incidence of osteoarthritis were not assessed and their results were equivocal with regard to return to work and function. In addition, more than half the patients required re-operation in order to remove broken metal-ware. No comment was made concerning the integrity of the SLIL repair at the second procedure. Apart from equivocal results achieved with closed and open methods of treatment, implant failure, and other surgical complications such as flexor tendon adhesions, superficial and deep wound sepsis and arthrofibrosis should be taken into account when considering the open treatment of PLDs.1,22,24-26
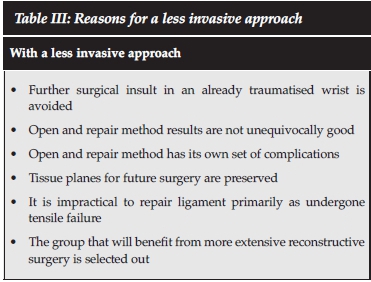
Table II compares this study with several other studies assessing the open treatment of these lesser arc injuries. The results of our study are comparable in most included fields. Table III summarises our rationale for a more conservative approach. The underlying premise is that some patients will do well without repair of the SLIL provided that anatomical reduction is achieved and maintained while the surrounding soft tissues heal. That is, not all patients go on to develop instability, precluding the need for potentially extensive yet unnecessary surgery in an already traumatised wrist. Those patients that do progress to develop symptomatic scapholunate dissociation select themselves out and are able to have an open reconstruction by one of the well-described techniques with the added benefit of a relatively unscarred surgical field. Secondly the SLIL has undergone tensile failure resulting in a circumferential mid-substance tear of both the volar and dorsal ligaments. Repair is unlikely to yield a ligament of sufficient strength to maintain carpal dynamics once the patient is mobilised. In addition, repair of both the SLIL and LT ligaments would require a combined dorsal/volar approach respectively, increasing the likelihood of surgical complications.
A limitation of this study is its small number of patients, which makes statistical correlation with clinical results difficult. It should be reiterated however that this study looks at an uncommon and very specific injury pattern and its numbers are comparable to those found in current similar studies. Furthermore, there are limited patient-related outcome measures (PROMs) included in this study. Although not as comprehensive as some of the more recent PROMs such as the patient-related wrist evaluation score, we did use the Mayo Wrist Score to assess functional outcomes. We chose this scoring system, as did many of the landmark articles on this topic, in order to achieve meaningful comparison with them. Potential bias exists in the study's interpretation of the post-operative X-rays. Only the senior surgeon in the study performed the analysis with no independent control. However, this was a radiological assessment, based on objective criteria, and it should be noted that the radiological parameters were not within normal range and reported as such, which speaks to their objectivity.
Conclusion
In conclusion, the results of this study show that the closed reduction and pinning of a purely ligamentous lesser arc injury or Mayfield type 3 and 4, yielded no poor results at medium-term follow-up. Furthermore it would appear that there is no medium-term benefit to repairing a ruptured SLIL. This approach minimises surgical trauma to the damaged wrist and preserves tissue planes for future surgery should it be required.
Compliance with ethics guidelines
Ethics approval was obtained. Ethics number HREC REF: 226/2014, University of Cape Town Human Research Ethics Committee.
Conflict of interest: All named authors hereby declare that they have no conflicts of interest to disclose.
Financial statement: No financial support was received for this study or publication including grants or pharmaceutical company support.
There was no commercial or financial involvement that might present an appearance of a conflict of interest related to the submission.
There was no sponsorship of the research that would prevent the authors publishing both positive and negative results or forbids the authors from publishing this research without the prior approval of the sponsor.
Funding statement: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Informed consent: Informed consent was taken from the patients prior to enrolment in the study and documented with the signing of a consent form.
References
1. Stanbury SJ, Elfar JC. Perilunate dislocation and perilunate fracture-dislocation. J Am Acad Orthop Surg, 2011;19(9):554-62. [ Links ]
2. Kardashian G, Christoforou DC, Lee SK. Perilunate dislocations. Bull NYU Hosp Jt Dis, 2011;69(1):87-96. [ Links ]
3. Adkison JW, Chapman MW. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res, 1982;164:199-207. [ Links ]
4. Grabow RJ, Catalano L, 3rd. Carpal dislocations. Hand Clin, 2006;22(4):485-500; abstract vi-vii. [ Links ]
5. Blazar PE, Murray P. Treatment of perilunate dislocations by combined dorsal and palmar approaches. Tech Hand Up Extrem Surg, 2001;5(1):2-7. [ Links ]
6. Apergis E, et al. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl, 1997. 275: p. 55-59. [ Links ]
7. Herzberg G, et al. Perilunate dislocations and fracture-dislocations: a multicenter study. J of Hand Surg Am, 1993;18(5):768-79. [ Links ]
8. Su CJ, et al. Lunate and perilunate dislocation. Zhonghua Yi Xue Za Zhi (Taipei), 1996;58(5):348-54. [ Links ]
9. Martinage A, et al. [Perilunate dislocations and fracture-dislocations of the wrist, a review of 14 cases]. Chir Main, 2008;27(1):31-39. [ Links ]
10. Cooney WP, et al. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res, 1987;(214):136-47. [ Links ]
11. Forli A, et al. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J of Hand Surg Am, 2010;35(1):62-68. [ Links ]
12. Tavernier L. Les deplacements traumatiques du semilunaire. Thesis, 1906: p. 138-39. [ Links ]
13. Arner M. Green's Operative Hand Surgery (Book). Acta Orthop Scand, 1999;70(4): 411. [ Links ]
14. Berger RA, Bishop AT, Bettinger PC. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg, 1995;35(1):54-59. [ Links ]
15. Suzuki D, et al. Comparison of scapholunate distance measurements on plain radiography and computed tomography for the diagnosis of scapholunate instability associated with distal radius fracture. J Orthop Sci, 2014;19(3):465-70. [ Links ]
16. Maizlin ZV, Vos PM. How to measure scapholunate and Cobb's angles on MRI and CT. J Digit Imaging, 2012;25(4):558-61. [ Links ]
17. Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J of Hand Surg Am, 2008;33(6):998-1013. [ Links ]
18. Short WH, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: Part II. J Hand Surg Am, 2005;30(1):24-34. [ Links ]
19. Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am, 2006;31(1):125-34. [ Links ]
20. Drewniany JJ, Palmer AK, Flatt AE. The scaphotrapezial ligament complex: an anatomic and biomechanical study. J Hand Surg Am, 1985;10(4):492-98. [ Links ]
21. Inoue G, Kuwahata Y. Management of acute perilunate dislocations without fracture of the scaphoid. J of Hand Surg Eur, 1997;22(5):647-52. [ Links ]
22. Souer JS, et al. Perilunate fracture-dislocations of the wrist: comparison of temporary screw versus K-wire fixation. J of Hand Surg Am, 2007;32(3):318-25. [ Links ]
23. Herzberg G. Perilunate and axial carpal dislocations and fracture-dislocations. J of Hand Surg Am, 2008;33(9):1659-68. [ Links ]
24. Hildebrand KA, et al. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J of Hand Surg Am, 2000;25(6):1069-79. [ Links ]
25. Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J of Hand Surg Am, 2004;29(3):412-17. [ Links ]
26. Knoll VD, Allan C, Trumble TE. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am, 2005;30(6):1145-52. [ Links ]
27. Sotereanos DG, et al. Perilunate dislocation and fracture dislocation: A critical analysis of the volar-dorsal approach. Journal of Hand Surgery 1997;22(1):49-56. [ Links ]
 Correspondence:
Correspondence:
Dr TL Hilton
Department of Orthopaedics Surgery
Groote Schuur Hospital
H49 OMB Observatory
Tel: 021 404 5118
Email: tlhilton@hotmail.com
Cell: 0027 (82) 796 7608














