Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.16 no.1 Centurion feb./mar. 2017
http://dx.doi.org/10.17159/2309-8309/2017/v16n1a7
SPINE
Early onset scoliosis: The use of growth rods
RD GovenderI; RN DunnII
IMBBCh(Wits), FC Orth(SA); AOSpine Fellow at the Spine Surgery Unit, Groote Schuur Hospital
IIMBChB(UCT), MMed(UCT)Orth, FCS(SA)Orth; Pieter Moll and Nuffield Chair of Orthopaedic Surgery and HOD University of Cape Town
ABSTRACT
BACKGROUND: Early onset scoliosis (EOS) is defined as scoliosis occurring before the age of 5 years. The management presents a unique challenge where both natural history and fusion lead to impaired cardiopulmonary function of the child.
AIM: To assess the outcome of the use of non-fusion instrumentation and repetitive elongation ('growth rods') in EOS.
METHODS: A retrospective review of 14 consecutive patients who underwent growth rod implantation and lengthening procedure for EOS was performed. Growth rod constructs were constructed predominately from modular commercially available sets using laminar hooks, pedicle screws and connection blocks, with single or double rod constructs. Vertical expanding prosthetic titanium ribs (VEPTR) were used in two patients. Patients returned to theatre at six-monthly intervals for a lengthening procedure. Patients were assessed with regard to type of scoliosis, age at surgery, number of lengthenings done, progression of Cobb angle, amount of construct lengthening, amount of spine growth achieved and complications.
RESULTS: The most common type of scoliosis seen was idiopathic (five), followed by neuromuscular (four), conjoined twins (two), syndromic (two), and congenital (one). Five patients were followed until final fusion, one procedure was stopped due to wound complications and one patient was lost to follow-up. The 14 patients had a median of seven lengthenings each. The median pre-operative Cobb angle was 56° (IQR 46.5°-59.5°) and median last follow-up Cobb angle of 32.5° (IQR 27.0°-44.5°). The median spine growth achieved was 97 mm (IQR 69-122 mm). Eight of the 14 patients (57%) experienced 14 complications during their lengthening procedures.
CONCLUSIONS: The growth rod instrumentation provides spinal deformity correction and control, while allowing ongoing growth of the spine. It is a labour-intensive process with significant incidence of complications. There is however very little other choice in these patients due to concerns of early fusion restricting pulmonary development.
Key words: spine, growth rods, scoliosis
Introduction
The management of scoliosis in the growing child presents a unique challenge to the treating surgeon due to the patient's small size, frequently associated comorbidities and pulmonary consequences with early fusion.
Early onset scoliosis (EOS) is defined as scoliosis occurring before the age of 5 years. It affects not only the growing spine but also has a direct influence on the cardiopulmonary development and function of the child.
Cardiopulmonary function is compromised as a result of the decreased size of the thoracic cavity, which has a negative effect on lung alveolar development.
The goal in the management of EOS is to control the deformity and allow continued growth of the spine and thoracic cavity. Non-fusion instrumentation facilitates this and allows ongoing respiratory development.
Aim
The purpose of this study was to assess the efficacy and complications of non-fusion instrumentation 'growth rods' in early onset scoliosis in a local context.
Patients and methods
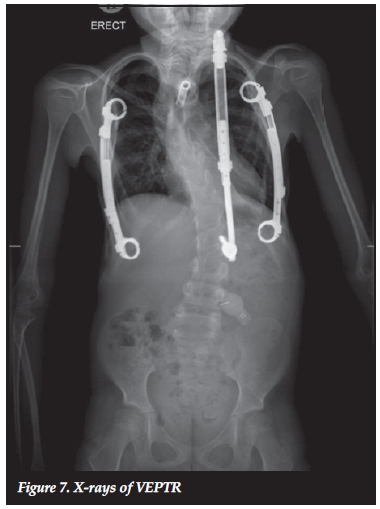
A retrospective review of 14 consecutive patients who underwent non-fusion repetitive lengthening surgery was performed. These patients were all treated by the senior author during the ten-year period 2004 to 2014. Various instrumentation constructs were used. The earlier patients underwent unilateral constructs while the later cases had bilateral rods implanted. Connector blocks allowed side-by-side rod assembly to facilitate subsequent lengthening (Figures 1-2). Pedicle screws were the default fixation but when not feasible or due to complications, hooks were used. Two vertical expanding prosthetic titanium rib (VEPTR) constructs were also employed in the cohort.

Definitive surgery, i.e. when final fusion surgery was performed, consisted of pedicle screws, dual rods and bone grafting.
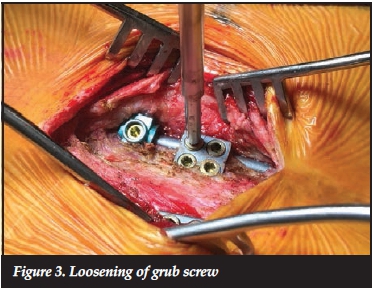
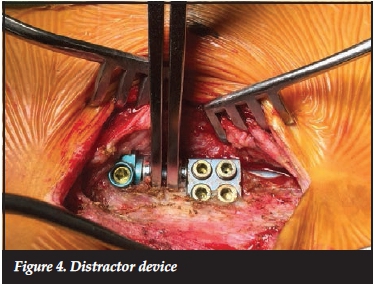
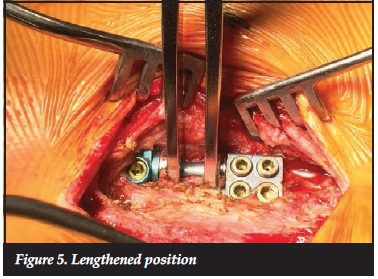
After the index procedure, patients returned to theatre at six-monthly intervals where the connector blocks were exposed, the rod loosened and manually lengthened with a distractor device and then retightened in the new distracted position (Figures 3-5).
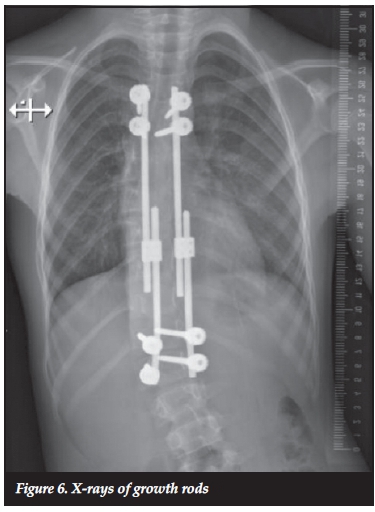
Standard scoliosis X-rays were taken at each admission (Figures 6-7). Patients were not braced post-operatively.
Data recorded included type of scoliosis, age at surgery, number of lengthenings done, progression of Cobb angle, amount of construct lengthening, amount of spine growth achieved (Tl-Sl height) and complications.
Results
Idiopathic (five cases) was the most common type of scoliosis followed by neuromuscular (four), conjoined twins (two), syndromic (two), and congenital (one). The average age at first surgical episode was 6 years 1 month. Five patients reached the end of their lengthening during the study period and were fused definitively. One lengthening was abandoned due to wound complications, and one case was lost to follow-up.
There were 95 lengthenings in the series, with a median of seven lengthening procedures per patient. Figure 8 illustrates the serial construct lengthenings achieved in each patient.

The median initial Cobb angle was 56° (IQR 46.5°-59.5°). The last follow-up median Cobb angle was 33° (IQR 27.0°-44.5°). This is reflected in Figure 9 along with a breakdown according to aetiology. Most correction is usually seen with the index procedure when the rods are inserted. Thereafter moderate correction is achieved with the subsequent lengthenings. All types of scoliosis showed an improvement in the Cobb angle. The congenital group showed the least relative deformity correction; however, these are known to have more rigid curves, which are less likely to correct.
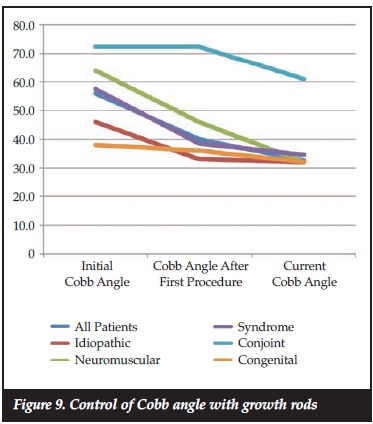
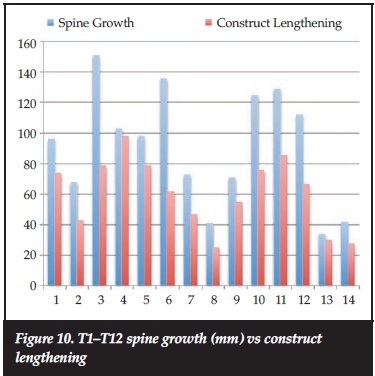
Spine growth was measured using the difference between the current and the initial Tl to SI length on the AP X-rays. The median spine growth achieved was 97 mm (IQR 69-122 mm) while the median increase in instrumentation construct length was 65 mm (IQR 44-78 mm). The average lengthening of the construct at each procedure was 8 mm. The median rate of spine growth was 27 mm/year (IQR 19-34 mm/year). Thus 67% of spinal growth was shown to have occurred in the instrumented segments of the spine.
Figure 10 shows the growth achieved in each patient compared to the amount of construct lengthening.
Eight of the 14 patients (57%) experienced complications during their lengthening procedures (Table I). In total, there were 14 separate complications noted during the study: four screws required revision to an adjacent level, three laminar hook revisions; four wound healing problems; two rod breakages (both in a neuromuscular scoliosis with a long construct); and a pneumothorax caused by a penetrating laminar hook at an index procedure.

Discussion
Early onset scoliosis is a heterogeneous group of conditions with varying prognoses and natural history depending on whether the aetiology is congenital, idiopathic, syndromic or neuromuscular.1 The goals of treatment include correction of the spinal deformity, maintenance of this correction during the growth phase, avoidance of arthrodesis of the spine, as well as allowing continued lung development and spinal growth.2
Fusion carried out in the thoracic spine at an early age has a negative impact on lung parenchyma development and pulmonary function. Early spinal fusion, especially if performed in the thoracic region, is a cause of respiratory insufficiency and adds the loss of pulmonary function to the spinal deformity. A thoracic spine height of 18 cm or more is necessary to avoid severe respiratory insufficiency.3 The forced vital capacity may decrease by 50% of predicted volume if more than 60% of the thoracic spine (i.e. eight thoracic vertebrae) is fused before the age of 8 years.4
The 'golden' period for both thoracic spine and thoracic cage growth occurs between birth and 8 years of age and coincides with lung development. The Tl-Sl spine segment measures around 20 cm at birth and increases to around 45 cm at skeletal maturity, with 40% of this growth occurring in the first 5 years of life.5
The source of potential respiratory failure is twofold, viz. ventilation is limited by chest wall deformity, and lungs are hypoplastic as normal growth is impaired by a restricted thoracic volume. It is important to preserve both thoracic growth and lung volume during this period. Patients with early onset deformities have fewer alveoli than expected and studies suggest that premature cessation of alveolar proliferation rather than mechanical compression is the cause.'
These children are predisposed to thoracic insufficiency syndrome, i.e. the inability of the thorax to ensure normal breathing due to severe alterations in the gas exchange. In the most serious cases, the clinical picture can be lethal.7
Another complication of early arthrodesis of the spine is the 'crankshaft phenomenon'. This is the progression of the spinal deformity after a posterior fusion, due to continued growth of the anterior portion of the spine.
Conservative interventions, including bracing and physical therapy, have not demonstrated efficacy in prospective or randomised clinical studies.8 Surgical treatment of early onset scoliosis is complex and has a high complication rate. In children with early onset spinal deformities with strong progression potential, expandable constructs are used to support the growth of the thoracic cage and accompanying lung growth. However, modern techniques and instrumentation control only one plane of the deformity as distraction forces are applied to the spine or thoracic cage.5 At present, there is no instrumentation able to fully control the multi-dimensional nature of early onset spinal deformities.
Skaggs et al. proposed a classification for growth friendly procedures based on the mechanism by which they modulated spinal and chest wall growth. The classification included distraction-based, compression-based and guided-growth techniques.1,9,11
Distraction-based implants
These implants correct and maintain the spinal deformity via distraction. Distraction-based implants can be attached to the spine, ribs or pelvis.1
Growing rod technique:
Growth rods provide structural support, correct and maintain the deformity and also allow axial spine growth. Serial lengthening of the rods is performed every 6-12 months thereafter.11,12 Indications for use of growth rods include patients who have significant axial spine growth remaining, a progressive deformity of more than 50° or a flexible spine deformity1,11 Improved surgical results have been achieved with the use of dual growth rods compared to a single growth rod; this is attributed to the improved stability of the construct.2,11,13 Complications noted in the literature with this technique include infection, rod breakage and screw pull-out.
Transcutaneously distracted magnetically driven rods became available recently but are too expensive for widespread use in our setting.
Vertical expandable prosthetic titanium rib (VEPTR):
This technique was developed to treat thoracic insufficiency syndrome. The device is connected to the ribs to primarily expand the constricted thorax and secondarily allow spine growth and indirectly correct the scoliosis.7,14 The goal is to restore the growing thorax to maximise development of the lungs; thus it should be the treatment option when addressing a thoracic deformity.2 Lengthening of the prosthesis is required every six months. Complications are similar to growing rods, namely wound problems, rib fractures and creeping fusion.1
Compression-based implants
This technique uses the Heuter Volkman principle of compression forces inhibiting growth.9 Vertebral staples are placed spanning the intervertebral disc spaces resulting in asymmetrical loading of the vertebral growth plates on the side that had the staple placement. Limited correction is possible with stapling. The literature on stapling is limited and the clinical indications for stapling are not universally accepted.11
Guided-growth implants:
The Luque trolley technique in which rods are attached to the spine using sublaminar wiring is largely of historical interest. Due to the extensive subperiosteal dissection most patients had a spontaneous fusion of the instrumented region. The Shilla technique allows spine growth to occur with screws that slide along the rods that are inserted proximally and distally.1
The management of early onset scoliosis is a prolonged and labour-intensive process. Complications are frequent and should be expected. They are related to the number of surgical procedures performed and the length of treatment.15 Wound breakdown, delayed healing and sepsis are frequent. Due to the non-fusion technique, screw/hook dislodgement, rod or screw breakage are seen. Junctional kyphosis and curve progression may also occur.13 These complications are the price to be paid for the non-fusion technique which allows ongoing thoracic growth and potential pulmonary development.
This technique allows for early correction and control of the deformity which makes the definitive surgery at a later stage, less complex.
Conclusion
Early onset scoliosis remains a challenging condition to treat. The growth rod instrumentation provides an option to correct and control the spinal deformity, while gaining growth in torsal height.
This allows thoracic wall growth and potentially allows for continued lung development. It is a labour-intensive process with significant incidence of complications.
There is, however, very little other choice in these patients due to concerns of early fusion restricting pulmonary development and eventual function.
Acknowledgement
Dr Peter Hardcastle contributed to the initial data collection while a registrar in the department.
Compliance with ethics guidelines
Prof Dunn and Dr Govender declare that this article is their original work. They have no conflict of interest and have received no commercial benefits of any kind for the writing of this article. Ethics clearance was obtained for the use of the patient information.
References
1. Gomez JA, Lee JK, Kim PD, Roye DP, Vitale MG. 'Growth friendly' spine surgery: management options for the young child with scoliosis. J AM Acad Orthop Surg 2011;19:722-27. [ Links ]
2. Thompson GH, Lenke LG, Akbarnia BA, et al. Early onset scoliosis: future directions. J Bone Joint Surg Am 2007;89-A:163-66. [ Links ]
3. Karol L, Johston C, Mladenov K et al. Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Joint Surg Am 2008;90:1272-81. [ Links ]
4. Goldberg CJ, Gillic I, Connaughton O, et al. Respiratory function and cosmesis at maturity in infantile-onset scoliosis. Spine 2003;28:2397-2406. [ Links ]
5. Dimeglio A, Canavese F. The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J 2012;21:64-70. [ Links ]
6. de Groodt EG, van Pelt W, Borsboom GI. Growth of the lung and thorax dimensions during the pubertal growth spurt. Eur Respir J 1988;1:102-108. [ Links ]
7. Campbell RM, Smith MD, Mayes TC et al. The characteristics of thoracic insufficiency associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am 2003;85:399-408. [ Links ]
8. Rowe DE, Bernstein SM, Riddick MF, et al. A meta analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am 1997;79:664-74. [ Links ]
9. Akbarnia BA, Campbell RM, Dimeglio A, et al. Fusionless procedures for the management of early-onset spine deformities in 2011: what do we know? J Child Orthop 2011;5:159-72. [ Links ]
10. Skaggs DL, Akbarnia BA, Flynn JM et al. A classification of growth- friendly spine implants. J Pediatr Orthop 2014;34(3):260-74. [ Links ]
11. Cunningham ME, Frelinghuysen PHB, Roh JS, et al. Fusionless scoliosis surgery. Curr Opin Pediatr 2005;17:48-53. [ Links ]
12. Yazici M, Emans J. Fusionless instrumentation systems for congenital scoliosis. SPINE 2009;17:1800-1807. [ Links ]
13. Akbarnia B, Marks D. Dual growing rod technique for the treatment of progressive early-onset scoliosis. Spine 2005;30(17S), S46-S57. [ Links ]
14. Campbell RM Jr, Hell-Vocke AK. Growth of the thoracic spine in congenital scoliosis after expansion thoracoplasty. J Bone Joint Surg Am 2003; 85:409-420. [ Links ]
15. Bess S, Akbarnia B. Complications of growing-rod treatment for early-onset scoliosis. J Bone Joint Surg Am. 2010; 92:2533-43. [ Links ]
 Correspondence:
Correspondence:
Prof RN Dunn
Department of Orthopaedic Surgery H49 OMB
Groote Schuur Hospital
7925 Observatory
Cape Town
Tel: 021 404 5387
Fax: 021 447 2709
Email: info@spinesurgery.co.za














