Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.15 n.4 Centurion Oct./Nov. 2016
http://dx.doi.org/10.17159/2309-8309/2016/v15n4a6
GENERAL
Vitamin D status in patients undergoing arthroplasty
Dr RF SnydersI; Dr JD JordaanII; Dr MN RasoolIII; Prof IE GogaIV
IMBChB(Stell), Orthopaedic Registrar, University of KwaZulu-Natal
IIMBChB(Stell), H Dip Orth, FC Ortho(SA), Consultant, Orthopaedic Surgeon
IIIMBChB(UKZN), FCS Orth(SA), PhD(UKZN), Consultant, Paediatric Orthopaedics, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IVFRCS(Edin), FCS Orth(SA), Head of Department: Orthopaedic Surgery, Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-Natal, South Africa
ABSTRACT
Vitamin D deficiency has, in recent literature, been associated with poorer outcomes following arthroplasty. This is a retrospective chart review of 209 patients presenting to a local arthroplasty unit in one year. The aim was to identify the prevalence of undiagnosed vitamin D deficiency in this group of patients. The results showed a 10% prevalence. In this study, Indian and Coloured female patients were most at risk (15-16% prevalence) and Black patients had the lowest prevalence (6.9%). In conclusion, the population presenting for arthroplasty at this unit is at risk of vitamin D deficiency, and we advocate vitamin D levels to be part of a standard metabolic workup in our environment.
Key words: vitamin D deficiency, arthroplasty, poor outcomes
Introduction
Lack of vitamin D has become a cause for concern in patients undergoing arthroplasty. Undiagnosed vitamin D deficiency has in recent years become very topical in the literature. Multiple studies have demonstrated inadequate vitamin D levels in populations who are otherwise healthy.1-3
Recent literature has shown an association with inferior post-operative outcomes following arthroplasty.3,4 Adverse outcomes are not just confined to arthroplasty, as shown in recent systematic review of prospective and retrospective studies.5
Although the association with adverse outcomes has been identified, the direct causative effect of low vitamin D status is poorly understood and requires further investigation.5
In current literature there is no existing data on vitamin D deficiency from South Africa in the population presenting for arthroplasty.
The purpose of this retrospective chart review was to determine the prevalence of vitamin D deficiency in the population presenting to Inkosi Albert Luthuli Central Hospital for arthroplasty surgical procedures from August 2012 to August 2013.
Materials and methods
Following ethical approval, we retrospectively reviewed the charts of all patients presenting for surgery at the arthroplasty unit for the period August 2012 to August 2013. The data was compiled using theatre registers and ward admissions. Vitamin D levels are routinely done for patients presenting for elective arthroplasty.
All the patients with recorded vitamin D 25(OH)D3 levels were included in this study.
All patients undergoing elective hip and knee replacement surgery were selected. Patients previously diagnosed with, or on treatment, for vitamin D deficiency were excluded.
The total admissions for surgical procedures for the time period numbered 345. Of the total number of admissions, 136 patients were excluded due to incomplete results or files, inconclusive results, or chronically receiving treatment for vitamin D deficiency. The remaining 209 were selected to be included in the study.
The data captured included gender, age, race, vitamin D level, and whether the patient underwent a total hip or knee replacement.
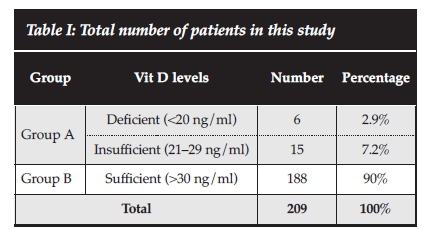
Insufficient and deficient levels were grouped together (Group A) and compared to the sufficient group (Group B). Deficient was classified as <20 ng/ml, insufficient as <30 ng/ml, and sufficient as >30 ng/ml, as described by the Endocrine Society in their clinical practice guidelines.6-8
With regard to statistical analysis, the data was entered in Microsoft Excel and subsequently analysed in SPSS version 21. Categorical variables were described using frequencies and percentages in tables and bar charts. Continuous variables were summarised using mean, standard deviation and range. Where the distribution was asymmetrical, median and interquartile range was used. A p-value of <0.05 was used to indicate statistical significance in the comparison of those with deficiencies or insufficient levels compared to those with sufficient levels. Independent samples' t-tests were used to compare ages between the two groups, and Pearson's chi-square test was used to compare the categorical variables between the two groups.
Results
The results showed that 10% (n=21) of the study population presented with undiagnosed vitamin D deficiency and insufficiency (Table I).
Of the 209 patients, 73.2% (n=153) were female and 26.8% (n=56) male.
According to the race distribution, Black patients were in the majority at 48.3% (n=101), Indian people comprised 28.2% (n=59), White 20.6% (n=43) and Coloured 2.9% (n=6).
Total hip replacements constituted the majority of surgical procedures at 59.3% (n=124) compared with total knee replacements at 40.7% (n=85) (Table II).

The mean age for the insufficient group was 62.43 years and 61.43 years for the sufficient group. There was no statistical difference between group A and B (Table III).

The total number of patients in the insufficient group was 21. Seventeen (81%) were female and four (19%) male. When grouped according to race, there were nine (42.9%) Indian, seven (33.3%) Black, four (19%) White and one (4.8%) Coloured patient. Fifteen presented for total hip replacements and six for total knee replacements.
We used Pearson's chi-squared test to compare categorical variables between the insufficiency and sufficient groups (Table IV). There were no significant statistical differences found regarding gender, age, race or joint involvement comparing group A to group B.
Discussion
Vitamin D deficiency is a common problem in patients presenting for hip and knee arthroplasty. Nawabi et al. showed a prevalence of 24% in their study of 62 patients presenting for hip arthroplasty.4 Jansen et al. similarly measured vitamin D levels in 139 elderly patients presenting for knee arthroplasty and also found a 24% prevalence.3 Both these studies dealt with mainly Caucasian populations. Although they were not specifically described for arthroplasty patients, an even higher prevalence has been found in other studies.2 Data from the United States (US) National Health and Nutrition Survey (NHANES) have found a prevalence nearing 30%.2 It is important to note that there is variation when it comes to the interpretation of vitamin D status. There is currently no consensus on the definition of vitamin D deficiency or which total serum levels are considered optimal.9
We considered the patient population presenting to this unit to be at risk for undiagnosed vitamin D deficiency. Most of these patients present with more than a single risk factor. Documented risk factors include darker skin, increasing age, obesity, and decreased sunlight exposure.10 The NHANES in the US found females and races of darker pigment (African Americans and Hispanics) to have lower vitamin D levels.2 A large percentage of the patients also present in advanced stages of their hip and knee pathology. Socio-economic conditions are poor and therefore nutritional factors may also play a role. Due to the burden of the lower limb pathology, they are constrained with regard to mobility, often presenting as home ambulators, and often have limited exposure to sunshine.
This study population consisted of 81% darker pigmented patients, and 73.2% were female. This study showed only a 10% prevalence, which was lower than expected. Males had a prevalence of 7.1%, and females 11.1%. Therefore, despite multiple risk factors, our overall prevalence is lower than similar previous studies. Further detailed analysis is required to identify why the prevalence in our study is not similar to comparable ones. These results may suggest that the local population's cutaneous and dietary intake of vitamin D is sufficient. Currently, there is no existing comparative data on vitamin D deficiency from South Africa in the arthroplasty population.
Recent literature in vitamin D levels in arthroplasty patients has stimulated interest in this study. Of particular concern is the association with adverse outcomes. The adverse outcomes are not confined to arthroplasty alone, as shown in a recent systematic review of prospective and retrospective studies.5 Iglar and Hogan identified diverse adverse outcomes associated with low pre-operative vitamin D status.5 These adverse outcomes related to orthopaedic procedures include decreased ambulation distance after surgery, increased pain scores, and decreased post-operative knee strength.3,5,11-13 Nawabi confirmed that patients with vitamin D deficiency had lower pre-operative Harris hip scores. Post-operatively, this group was less likely to attain excellent Harris hip scores.4 Jansen and Haddad found similar results in total knee arthroplasty with significantly lower Knee Society Scores pre- and post-operatively in vitamin D deficient patients.3 Further negative effects of vitamin D deficiency include poor bone mineralisation and detrimental effects on fracture healing.7 Maier et al. have shown a statistically significant association with low vitamin D status and peri-prosthetic joint infection in hip, knee and shoulder arthro-plasty.14
It must be highlighted that in this study there was no data collected to determine whether deleterious outcomes were associated with the 10% found to have deficient vitamin D status.
Specific race analysis showed Indian and Coloured race groups to have the highest prevalence. Indian study subjects had a 15% prevalence and Coloured 16% compared to White 9% and Black only 6.9%. Based on these findings the black population presenting for arthro-plasty has the lowest prevalence. It also indicates that Indian and Coloured female patients are most at risk for presenting with vitamin D deficiency in our environment.
Although the mean age in both groups were similar, it was lower compared to similar studies. This may be due to the lower life expectancy of people in KwaZulu-Natal (KZN).15 According to a report published by Statistics South Africa in July 2014 the average life expectancy from birth for males in KZN is only 54.4 years, and 59.4 years for females.15
Another contributing factor may be the increase of younger (<55 years) patients presenting with avascular necrosis (AVN) of the hip. This unit identified AVN to represent 67% of the aetiology of patients under the age of 55 years undergoing total hip replacement surgery.16
Emphasis has mostly been placed on the association of low vitamin D status and adverse outcomes, but there is no current evidence that supplementation is of any benefit.17 It would be logical to use supplementation as treatment to optimise pre-operative vitamin D status. Replacement therapy has shown improvements in intensive care mortality and optimal status is clearly beneficial, but more studies are required to define whether supplementation is beneficial in the peri-operative setting of deficiency relating to arthroplasty.18,19
The strength of this study was the number of patients in the study population as well as the multiracial distribution.
Limitations in this study would include the disproportionate ratio of the various race groups, and the lack of consensus regarding definitions, which impair comparison to similar studies. Since no functional assessment data was captured, we are also unable to comment about adverse outcomes, and whether, if any, association exists with low vitamin D status in our study population.
More studies are required to accurately define the role vitamin D deficiency plays in the population of patients presenting for arthroplasty. Further evidence is required regarding adverse outcomes following arthroplasty in patients with vitamin D deficiency, and whether they correlate with existing literature. This information may be valuable to prevent adverse outcomes in our patients.
Conclusion
We conclude that the patient population presenting for arthroplasty at our unit is at risk of undiagnosed vitamin D insufficiency, although it is less than in similar study groups. More research is required regarding the association vitamin D deficiency has with adverse outcomes, especially in understanding whether there is a direct link or a mere association.
Compliance with ethics guidelines
The content of this article is the original work of the authors. Drs Snyders, Jordaan and Rasool and Prof Goga have no conflicting interests, and received no benefits for writing this article. Ethical approval was obtained.
References
1. Mithal A, Wahl DA, Bonjour JP, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 2009;20:1807-20. [ Links ]
2. Yetley EA. Assessing the vitamin D status of the US population. Am J Clin Nutr 2008;88:558-64. [ Links ]
3. Jansen JA, Haddad FS. High prevalence of vitamin D deficiency in elderly patients with advanced osteoarthritis scheduled for total knee replacement associated with poorer preoperative functional state. Ann R Coll Surg Engl 2013;95:569-72. [ Links ]
4. Nawabi DH, Chin KF, Keen RW, Haddad FS. Vitamin D deficiency in patients with osteoarthritis undergoing total hip replacement: A cause for concern? J Bone Joint Surg Br 2010; 92:496-99. [ Links ]
5. Iglar PJ, Hogan KJ. Vitamin D status and surgical outcomes: a systematic review. Patient Safety in Surgery 2015;9:15. [ Links ]
6. Binkley N, Krueger D, Cowgill CS, et al. Assay variation confounds the diagnosis of hypovitaminosis D: A call for standardization. J Clin Endocrinol Metab 2004;89:3152-57. [ Links ]
7. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30. [ Links ]
8. Patton CM, Powell AP, Patel AA. Vitamin D in orthopaedics. J Am Acad Orthop Surg 2012;20:123-29. [ Links ]
9. LeFevre ML. Screening for Vitamin D Deficiency in Adults: US Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;162:133-40. [ Links ]
10. Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266-81. [ Links ]
11. Unnanuntana A, Rebolledo BJ, Gladnick BP, Nguyen JT, et al. Does vitamin D status affect the attainment of inhospital functional milestones after total hip arthroplasty? J Arthroplasty. 2012;27:482-89. [ Links ]
12. Mak JC, Klein LA, Finnegan T, Mason RS, et al. An initial loading-dose vitamin D versus placebo after hip fracture surgery: baseline characteristics of a randomized controlled trial (REVITAHIP). BMC Geriatr. 2014;14:101- 109. [ Links ]
13. Barker T, Martins TB, Hill HR, Kjeldsberg, et al. Low vitamin D impairs strength recovery after anterior cruciate ligament surgery. J Evid-Based Complement Altern Med. 2011;16:201-209. [ Links ]
14. Maier GS, Horas K, Seeger JB, Roth KE, et al. Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop. 2014;38:1499-1504. [ Links ]
15. Statistics-SA. Mid-year population estimates 2014 - Report P0302/ Statistics South Africa. Pretoria, 2014. [ Links ]
16. Ryan P, Goga IE. Uncemented primary total hip arthroplasty in patients aged 55 years or younger: Results at a minimum of 5 years in a consecutive series. SA ortho J. 2014 Mar;13: 54-60. [ Links ]
17. Straube S, Derry S, Straube C, et al. Vitamin D for the treatment of chronic painful conditions in adults. Cochrane Database Syst Rev. 2015;5:CD007771. [ Links ]
18. Zajic P, Amrein K. Vitamin D deficiency in the ICU: a systematic review. Minerva Endocrinol. 2014;39:275-87. [ Links ]
19. Amrein K, Schnedl C, Holl A, Riedl R, et al. Effect of highdose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA. 2014;312:1520-30. [ Links ]
 Correspondence:
Correspondence:
Dr RF Snyders
Department of Orthopaedic Surgery
University of KwaZulu-Natal
Nelson R Mandela School of Medicine
Private Bag 7
Congella, Durban, 4001
Email: snyders.rob@gmail.com














