Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.15 n.3 Centurion Aug./Sep. 2016
http://dx.doi.org/10.17159/2309-8309/2016/v15n3a10
SHOULDER
Treatment of chronic anterior shoulder dislocations: Limited goal surgery
Dr B GreyI; Dr P RyanII; Dr N BhagwanIII
IMBChB(Pret), HDip Orth(SA), FCOrth(SA), MMed(Orth); Orthopaedic Surgeon, Edendale Hospital, Pietermaritzburg and Department of Orthopaedics, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
IIMBChB(UCT), HDip Orth(SA), FCOrth(SA), MMed(Orth); Orthopaedic Surgeon, Inkosi Albert Luthuli Central Hospital and Department of Orthopaedics, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
IIIMBChB, FCOrth(SA); Orthopaedic Surgeon, Mediclinic Pietermaritzburg
ABSTRACT
BACKGROUND: Chronic anterior shoulder dislocations are encountered relatively frequently in KwaZulu-Natal, South Africa. Various surgical options exist to treat these injuries; however, the reported results of such interventions are not uniformly favourable. There remains the opinion that such cases are perhaps best treated with 'skilful neglect'.
METHODS: We present a combined case series of chronic anterior shoulder dislocations treated surgically. Patients were identified retrospectively using departmental databases and their case files, available X-rays, CT scans and MRI scans were reviewed. Surgical outcome was assessed using range of movement, change in pain severity, the Oxford Shoulder Instability Score, the Rowe and Zarins score, as well as a patient satisfaction score.
RESULTS: Twenty-six patients were included in the study. The average duration of dislocation was 9 months (range 2 weeks to 7 years). The most common reason for chronicity was delayed presentation to clinic or hospital (nine patients). A Hill-Sachs lesion was present in 20 patients, and a pseudo-glenoid was often encountered in dislocations present for more than 4 weeks (16 of 23 patients). Three supraspinatus ruptures and four biceps tears were encountered, while neurological injury was uncommon (two patients). Surgical treatment included open reduction (one patient), open reduction and Latarjet (15 patients), hemi-arthroplasty (two patients), hemi-arthroplasty and Latarjet (three patients) and reverse total shoulder arthroplasty (five patients). Eighteen patients were available for clinical review. Regardless of the type of surgery done, postoperative range of motion and surgical outcome scores were generally poor. Despite this, most patients (16 of 18 patients) were satisfied with their outcome due to reduction in pain. Two patients were dissatisfied, due to re-dislocation.
CONCLUSION: Surgical treatment of chronic anterior shoulder dislocation results in limited improvement in range of motion and overall shoulder function. However, high patient satisfaction levels and significant improvement in pain levels can be expected. Patients should be counselled pre-operatively regarding this 'limited goal surgery'.
Key words: subclinical hypoperfusion, occult, lactate, meta-analysis
Background
Chronic shoulder dislocations are a relatively rare occurrence. Rowe and Zarins reported that 51% of orthopaedic surgeons in practice for 5-10 years had encountered a chronic shoulder dislocation.1 However, in KwaZulu-Natal, South Africa, they are seen more frequently. Even though posterior shoulder dislocations frequently present as chronic dislocations, chronic anterior shoulder dislocations are encountered twice as often as posterior dislocations.1-3 Different durations have been used to define a dislocation as chronic. Rowe and Zarins used three weeks to define chronicity because closed reduction is seldom possible after three weeks.1 Goga used one week to define a shoulder dislocation as being chronic.4 He further sub-classified them into early (1-3 weeks), late (3-12 weeks) and ancient (> 12 weeks).
Chronic shoulder dislocations are commonly caused by seizures and are more common in elderly patients as well as in polytrauma patients with diminished levels of consciousness.2,3 The anterior dislocation presents with a variety of associated bony pathology including postero-lateral humeral head impression fractures, proximal humerus fractures, glenoid rim fractures, coracoid fractures and pseudoglenoid formation.1,2,5 Associated soft tissue pathologies include rotator cuff injuries, capsulo-labral detachments and biceps tendon injuries.1,2Neurological injuries and axillary artery injuries have also been reported, especially after attempts at closed reduction.2,6 The duration of dislocation influences the associated pathology which in turn influences the surgical treatment chosen and subsequent outcome.3 As the patient attempts to increase glenohumeral movement in the dislocated shoulder, the abnormal osseous contact leads to progressive enlargement of the humeral head and glenoid rim defects.5
Early literature on the treatment of chronic anterior shoulder dislocations suggested that non-operative treatment termed 'skilful neglect' yielded satisfactory results and should be considered in elderly low-demand patients or when pain and functional deficit is limited.2,3However, shoulder pain and severe loss of function is common in patients with unreduced dislocations.1
Recent studies have shown good outcomes following surgical treatment of chronic shoulder dislocations.4,7,8Various surgical methods have been attempted. Open reduction is usually done via a delto-pectoral approach. Posterior capsular release or complete capsular release is often required to achieve reduction. Options to improve anterior stability include Bankart repair8 or the Latarjet procedure.4 Iliac crest autograft can also be used to address glenoid insufficiency. Additional temporary gleno-humeral or acromio-humeral K-wire fixation has also been utilised to maintain reduction.2,4,7 Stiffness and re-dislocation are common complications following surgical treatment.3
Arthroplasty is indicated for chronic anterior shoulder dislocations with humeral head defects exceeding 40%, or when severe degenerative changes have developed. It can also be considered in dislocations of longer than six months' duration. Different types of arthroplasty have been performed. Pritchett and Clark treated seven patients with chronic shoulder dislocations (four anterior, three posterior) with hemiarthroplasty or total shoulder arthro-plasty.9 More than 30% of the humeral head was damaged in each case. Five patients had a good result and two had a fair result. There were no re-dislocations. Excisional arthroplasty, also known as the Jones procedure, has been performed in low demand patients but outcomes are less favourable.1,2 More recently Drignei et al. treated six patients with chronic anterior shoulder dislocations with a reverse total shoulder replacement.10 All patients were stable post-operatively with improved shoulder mobility and outcome scores.
Methods
We present a combined case series of patients with chronic anterior shoulder dislocations treated surgically during the last 5 years. Patients were identified and their hospital records traced using departmental databases. Patient demographics, duration of dislocation, mechanism of injury and reason for delayed treatment were recorded. When available, patient X-rays, CT scans and MRIs were reviewed to identify associated bony and soft tissue pathology. The surgical procedure performed was identified. Patients were then contacted to be reassessed in clinic. Surgical outcome was assessed using current shoulder range of movement, change in pain severity, patient satisfaction, as well as the Oxford Shoulder Instability Score11 and Rowe and Zarins score.1 Postoperative complications were also recorded.
Results
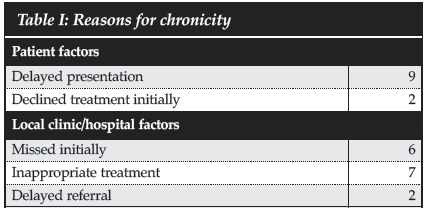
Twenty-six patients with chronic anterior shoulder dislocations were identified (23 males and three females). The average age was 48 years (range 25-84 years). Thirteen left shoulders and 13 right shoulders were affected. In patients where dominance had been recorded, the non-dominant side was found to be more commonly affected (13 of 21 shoulders). The average duration of dislocation was 9 months, ranging from 2 weeks to 7 years. The mechanism of injury was a fall in 13 (50%) patients, a seizure in six (23%), motor vehicle accident in three (12%), assault in three (12%) and a low energy injury in one patient. The reasons for chronicity are shown in Table I.
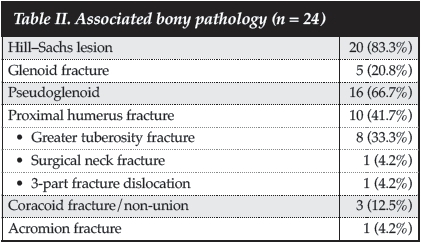
CT scans and/or X-rays were available for review in 24 patients and the associated bony pathology identified is summarised in Table II. Associated soft tissue pathology consisted of three supraspinatus ruptures, four long head of biceps ruptures and two patients with neurological injuries.
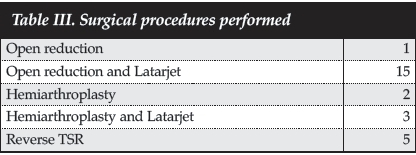
Pre-operatively all patients complained of pain and this was the main indication for surgery. Due to the retrospective nature of this case series, the pain severity was not graded. Shoulder range of movement was assessed pre-operatively in 17 patients. The average shoulder abduction was 37° (5°-80°), average forward flexion was 40° (5°-90°) and average external rotation was -3° (-20° to 10°). Neurological symptoms were present in two patients. One patient complained of paraesthesia in his hand and one patient had an incomplete distal brachial plexus palsy with 3/5 power. None of the patients had axillary nerve injuries. The various surgical procedures are tabulated in Table III. A temporary K-wire was used in four patients (gleno-humeral wire in three patients after open reduction and Latarjet; acromio-humeral wire in one patient following hemi-arthroplasty and Latarjet). The K-wires were removed between 1 and 4 weeks.
Eighteen patients were available for clinical review. Four patients had demised and four patients could not be contacted. The average follow-up duration at the latest visit was 17 months (range 3-72 months). The average shoulder abduction was 68° (20-160°), average forward flexion 71° (20-160°) and average external rotation 14° (-5° to 60°). Pain improved in all but one patient and was completely absent in three patients. According to the Oxford Instability Score, four patients achieved an excellent outcome, eight good, three fair and one poor.
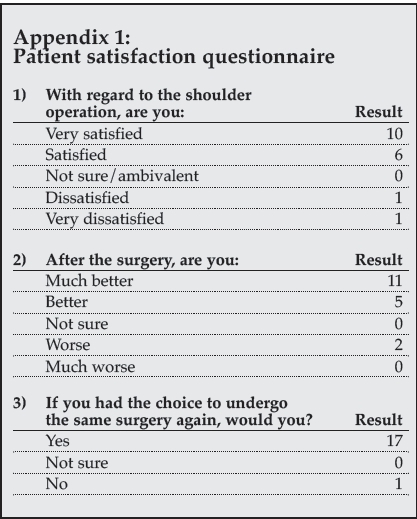
Using the Rowe and Zarins Score, five patients had poor outcomes and only two patients had excellent results, six good and four fair. Following the questionnaire, 16 out of 18 patients were very satisfied or satisfied with the outcome and felt either much better or better following surgery and would choose surgery again (Appendix 1). All of these patients related their satisfaction to the improvement of pain even if range of motion was still restricted.
The following complications were encountered: One patient sustained an iatrogenic rotator cuff injury which required repair at the same setting. One patient developed superficial wire site sepsis after 4 weeks which resolved following wire removal. One patient developed deep surgical site infection 18 months following open reduction and Latarjet. This resolved following debridement and a course of antibiotics. Following open reduction and Latarjet procedure, three patients developed severe osteoarthritis with deformation of the humeral head and one patient re-dislocated her shoulder. She had not followed post-operative instructions and started to bear weight on the affected upper limb on day 1 post-opera-tively. Although she was dissatisfied with her outcome, she declined further surgery. The other patient who was dissatisfied with his outcome was treated with hemiarthroplasty and Latarjet procedure due to severe bone loss of the humeral head and glenoid. His Latarjet procedure failed after a physical altercation and had to be revised with iliac crest autograft. The hemiarthroplasty eroded through the autograft soon after revision and now articulates against the screws through the graft. He is awaiting removal of the screws.
Discussion
Chronic anterior shoulder dislocations are encountered relatively frequently in KwaZulu-Natal, South Africa. We found that the most common reason for chronicity was delayed presentation to hospital. Unfortunately hospitals and clinics were also at fault, with a large number of dislocations being missed or managed inappropriately initially (Table I).
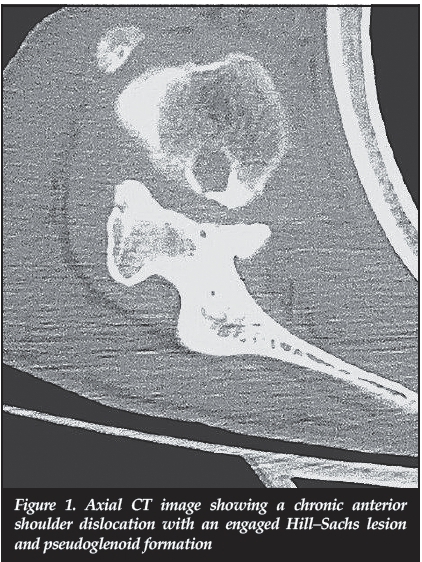
Hill-Sachs lesions were commonly encountered and were typically engaged at presentation, making closed reduction virtually impossible and dangerous due to the risk of fracture. A pseudoglenoid5 was present on the anterior aspect of the glenoid neck in 16 patients (66.7%) and in all of these patients the duration of dislocation was longer than 4 weeks (Figure 1). This false articulation develops with time as the humeral head progressively erodes the anterior part of the glenoid neck. A glenoid fracture fragment can form part of the medial edge of the pseudoglenoid as shown in Figure 2a.
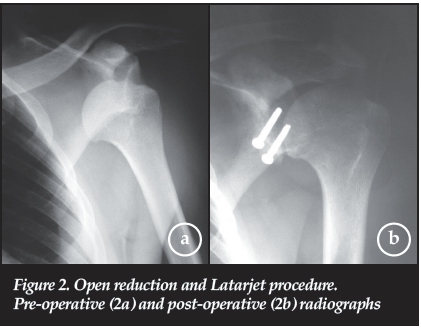
Various surgical procedures were performed and it was not the aim of this study to compare treatment options. Most patients were treated with open reduction and Latarjet procedure if the Hill-Sachs lesion was smaller than 40% of the humeral head (Figure 2). A coracoid osteotomy is often required to improve access during an open reduction, especially when the humeral head is located very medial and by performing a Latarjet procedure following open reduction, the glenoid rim erosion as well as the soft tissue imbalance is addressed.
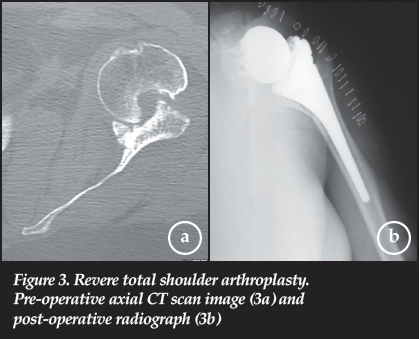
Hemiarthroplasty was chosen in cases where more than 40% of the humeral head was destroyed, and this was combined with a Latarjet procedure if a coracoid osteotomy was required during surgical exposure or if glenoid erosion was present. Reverse total shoulder replacement was performed in select cases with severe humeral head bone loss and significant rotator cuff atrophy and fatty infiltration (Figure 3). One patient required a reverse shoulder replacement following a failed open reduction. Although all of these patients did very well post-operatively, the long-term outcome of reverse total shoulder replacements in this patient group is still unknown.
Some improvement in shoulder range of motion was observed in all patients, regardless of treatment method. However, elevation was typically still below shoulder level. Range of motion only returned to near normal in one patient who had an open reduction and Latarjet for a chronic shoulder dislocation of only 2 weeks' duration. This dramatic improvement in range of motion and the ease of open reduction in this case underscores the need to differentiate the early chronic dislocation (<3 weeks) from the late chronic dislocation (3-12 weeks) as classified by Goga.4 The surgical outcome scores used in this study differed remarkably in judging clinical outcome. The Rowe and Zarins Score1 is a 100 unit scoring system that rates pain, motion and function in patients with chronic shoulder dislocations.
The Oxford Shoulder Instability Score11 is normally used in patients with recurrent shoulder instability, and did not correlate well with the Rowe and Zarins Score. Its usefulness is therefore questioned in patients with chronic shoulder dislocations. We found that the simplest tool to gauge outcome was a questionnaire regarding patient satisfaction.
Conclusion
Chronic anterior shoulder dislocations are still frequently encountered in KwaZulu-Natal, mostly due to delayed presentation. An engaged Hill-Sachs lesion is commonly present and a pseudoglenoid is typically formed after 4 weeks. Regardless of surgical treatment chosen, the gain in shoulder range of motion is limited, but surgery is still advocated due to the relief of pain.
Compliance with Ethics Guidelines
Drs Grey, Ryan and Bhagwan declare that this article is their original work. They have no conflict of interests and have received no commercial benefits of any kind for the writing of this article. Ethics clearance was obtained for the use of the patient information.
References
1. Rowe CR, Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am. 1982 Apr;64(4):494-505. [ Links ]
2. Schulz TJ, Jacobs B, Patterson RL, Jr. Unrecognized dislocations of the shoulder. J Trauma. 1969 Dec;9(12):1009-23. [ Links ]
3. Loebenberg MI, Cuomo F. The treatment of chronic anterior and posterior dislocations of the glenohumeral joint and associated articular surface defects. Orthop Clin North Am. 2000 Jan;31(1):23-34. [ Links ]
4. Goga IE. Chronic shoulder dislocations. J Shoulder Elbow Surg. 2003 Sep-Oct;12(5):446-50. [ Links ]
5. Kirtland S, Resnick D, Sartoris DJ, Pate D, Greenway G. Chronic unreduced dislocations of the glenohumeral joint: imaging strategy and pathologic correlation. J Trauma. 1988 Dec;28(12):1622-31. [ Links ]
6. Verhaegen F, Smets I, Bosquet M, Brys P, Debeer P. Chronic anterior shoulder dislocation: aspects of current management and potential complications. Acta Orthop Belg. 2012 Jun;78(3):291-95. [ Links ]
7. Akinci O. Open reduction of old unreduced anterior shoulder dislocations: a case series including 10 patients. Eur J Orthop Surg Traumatol. 2010;20:123-29. [ Links ]
8. Rouhani A, Navali A. Treatment of chronic anterior shoulder dislocation by open reduction and simultaneous Bankart lesion repair. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:15. [ Links ]
9. Pritchett JW, Clark JM. Prosthetic replacement for chronic unreduced dislocations of the shoulder. Clin Orthop Relat Res. 1987 Mar(216):89-93. [ Links ]
10. Drignei M SM. Treatment of chronic dislocations of the shoulder by reverse total shoulder arthroplasty: a clinical study of six cases. Eur J Orthop Surg Traumatol. 2009;19(8):541-46. [ Links ]
11. Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br. 1999 May;81(3):420-26. [ Links ]
 Correspondence:
Correspondence:
Dr B Grey
Department of Orthopaedics
Nelson R Mandela School of Medicine
University of KwaZulu-Natal
3200 Pietermaritzburg
South Africa
Tel: +27 31 2604297
Email: bcgrey@gmail.com