Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.15 n.3 Centurion Aug./Sep. 2016
http://dx.doi.org/10.17159/2309-8309/2016/v15n3a6
HIP
Lower limb deep vein thrombosis as a complication of posterior dislocation of a total hip replacement: A case report
Prof PK OrokoI; Prof KL MutisoII
IMMed(Surg), FRCS(Ed & Eng), FRCS(Tr & Orth); Assistant Professor, Department of Surgery, Aga Khan University Hospital, Nairobi
IIMRCP, FRCR; Assistant Professor, Department of Radiology, Aga Khan University Hospital, Nairobi
ABSTRACT
CASE: A 56-year-old woman who developed deep venous thrombosis 6 weeks after dislocating her ipsilateral total hip replacement is presented. She was found to have an organising haematoma in her psoas and iliacus muscles compressing the common femoral and external iliac veins proximal to the thrombus on imaging. The haematoma was considered to have been caused by abrasion of the muscles against the sharp edge of the acetabular shell.
CONCLUSION: Deep venous thrombosis should be considered a cause of ipsilateral lower limb swelling in a patient who has recently had a posterior total hip replacement dislocation.
Key words: deep vein thrombosis, total hip arthroplasty, dislocation
Introduction
Symptomatic deep venous thrombosis (DVT) was shown, in a large Scottish study, to occur in 2.7% of patients following hip arthroplasty with the increased risk continuing for about 3 months.1 In addition, the patient has the general population risk of development of DVT of 5/10 000.2 The case of a 56-year-old woman who had a well-functioning total hip replacement done 18 months previously and developed ipsilateral deep venous thrombosis is presented. She had dislocated her total hip replacement 6 weeks before presentation and this was considered to be the cause of her DVT. A literature search did not reveal previously reported cases of DVT occurring after a total hip replacement dislocation.
Case report
A 56-year-old woman was seen at our hospital while visiting the country on international official duty. She gave a history of swelling of the left leg of 2 days' duration.
This was painless and at the time of presentation had reduced significantly. She had had a left uncemented total hip replacement carried out abroad 18 months previously. She did well post-operatively and her function was excellent. However, while on a long trip to a third country 2 months before presentation, she had a posterior dislocation of the hip. This was reduced after two attempts. The first reduction was very difficult and was thought to have been successful but on X-ray the hip was clearly dislocated, warranting a second attempt. Following reduction, she used a knee brace for about a week and travelled back to the country of her residence in the brace. She had swelling of her lower limb which lasted about 2 days. Following this, she had another episode of swelling of the left lower limb which started 2 weeks before presentation and lasted 2 days. Apart from three episodes of swelling since her hip dislocation, she had no other symptoms in her left leg.
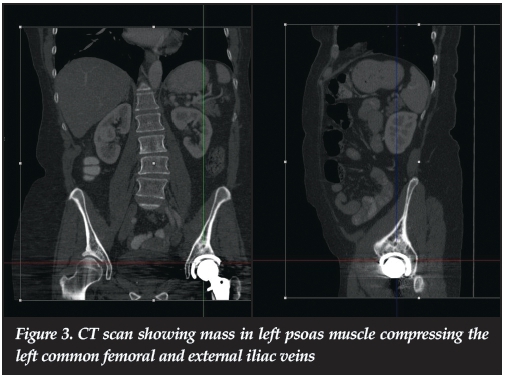
On clinical examination, she had mild swelling of her left lower limb without any area of tenderness. A Doppler ultrasound scan, ordered on the suspicion of DVT, showed a thrombus at the left common femoral vein. Because of a history of possible axillary lymph nodes and the DVT, a CT scan of her chest, abdomen and pelvis was carried out.
This showed a large mass in the left psoas muscle which was pressing on the left external iliac vein and extending to the left common femoral vein. A further ultrasound of her left groin was carried out and this confirmed a soft tissue mass which was smooth, regular and having the echogenicity of soft tissue with no fluid being seen in the mass. An MRI scan of her pelvis was then carried out. This showed a well encapsulated T2w high/intermediate signal intensity lesion in the left psoas and iliacus muscles measuring approximately 10 cm x 2.9 cm x 5.2 cm which was compressing the left external iliac and common femoral veins. There was a further smaller lesion with similar MRI characteristics measuring about 1 cm across in the iliacus muscle. These appearances were most suggestive of organising haematomas. She was started on treatment with Clexane (enoxaparin) and warfarin and discharged for follow-up in her country of residence.
She had follow-up in her country of residence with pelvic CT scans with contrast being carried out at 5 weeks and 16 months from the start of treatment. The first scan showed a markedly diminished lesion in her left iliopsoas muscle measuring 17 mm x 14 mm with restoration of the dimensions of the ipsilateral external iliac and common femoral veins. The 16-month scan showed complete resolution of the lesion in the iliacus and psoas muscles with normal external iliac and common femoral veins which were devoid of thrombus.
Discussion
Dislocations occur in 1-3% of primary and 5-20% of revision hip arthroplasties.3 The most cited study is that of the Mayo database which reported a dislocation rate of 3.2% in 10 500 primary total hip replacements.4 As there are a large number of procedures carried internationally, there are many patients who experience this complication. A literature search, however, did not reveal any case reports of DVT accompanying this complication of arthroplasty.
The cause of the DVT in this case appears to be due to compression of the femoral and common iliac veins from haematomas in the iliacus and psoas muscles. The compression caused stasis in these veins and consequent thrombosis. The cause of the haematoma was most likely due to direct trauma to the iliacus and psoas muscles during the posterior dislocation. Such a dislocation could cause direct abrasion of the muscles against the edge of the metallic shell at the anterior aspect of the acetabulum. The resulting haematoma then led to compression of the veins leading to limb swelling soon after the dislocation. That the haematoma was organising would indicate that the haematoma had occurred some time ago and 2 months would be a suitable duration. The patient had other risk factors for development of DVT which included immobilisation of her lower limb in a knee brace and a long haul flight. The presence of muscular haematomas, however, supports trauma associated with dislocation as the cause of her DVT.




Treatment of this condition was complicated by the persisting swellings in the iliacus and psoas muscles. Acute decompression of the haematomas was thought too risky as it would lead to immediate widening of the lumen of the veins leading to a risk of thrombo-embolisation. A decision to first treat the DVT with anticoagulants was therefore made, with resolution of the muscular haematomas expected with time. This resolution was confirmed with follow-up imaging.
Complicating intramuscular haematomas causing DVT should be considered in a swollen limb after a total hip replacement dislocation.
Compliance with Ethics Guidelines
Profs PK Oroko and KL Mutiso declare that the content of this article is their original work. No benefits of any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. The study was done in accordance with the institutional ethics guidelines.
References
1. Howie C, Hughes H, Watts AC. Venous thrombo-embolism associated with hip and knee replacement over a 10 year period. A population based study. J. Bone Joint Surg Br 2005;87-B(12):1675-80. [ Links ]
2. Fowkes FJ, Price JF, Fowkes FG. Incidence of diagnosed deep vein thrombosis in the general population: Systematic review. Eur J Vasc Endovasc Surg 2003 Jan;25(1):1-5. [ Links ]
3. D'Angelo F, Murena L, Zatti G, Cherubino P. The unstable total hip replacement. Indian J Orthop 2008;42:252-59. [ Links ]
4. Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am 1982;64(9):1295-306. [ Links ]
 Correspondence:
Correspondence:
Prof Parmenas K Oroko
Aga Khan University Hospital
3rd Parklands Avenue
PO Box 30270 code 00100
Nairobi, Kenya
Email: parmenas.oroko@aku.edu
Tel: +254 705137186














