Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.15 no.3 Centurion ago./sep. 2016
http://dx.doi.org/10.17159/2309-8309/2016/v15n3a3
TRAUMA
Open reduction and internal fixation of calcaneus fractures through a sinus tarsi approach
P JordaanI; S MaqungoII; S RocheIII; R MagampaIV; G McCollumV
IMBChB(Stell), DA(SA); Registrar, Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
IIMBChB(Natal), MMed(UCT), FCOrth(SA); Consultant Orthopaedic Surgeon, Groote Schuur Hospital
IIIMBChB(UCT), FCS(SA)Orth; Consultant Orthopaedic Surgeon, Groote Schuur Hospital
IVMBChB(Pret); Registrar, Orthopaedic Surgery, Groote Schuur Hospital, University of Cape Town
VMBChB(UCT), Dip Pec(SA), MMed(UCT), FCOrth(SA); Consultant Orthopaedic and Foot and Ankle Surgeon, Groote Schuur Hospital
ABSTRACT
INTRODUCTION: The wound complication rate for open reduction and internal fixation of calcaneus fractures through the extensile approach is 30%. Due to this high rate of wound complications, many surgeons prefer conservative management. If post-traumatic arthritis develops, the clinical results of a subtalar fusion are better if the posterior facet is reduced and the shape of the calcaneus restored. The sinus tarsi approach utilises a much smaller incision and indirect reduction techniques limiting the need for a large incision while still providing good exposure of the posterior facet for anatomic reduction
The purpose of this study is to present the technique for open reduction and internal fixation through a sinus tarsi approach, to assess the adequacy of reduction and the complication rate.
METHODS: A retrospective chart and X-ray review was performed of all patients who had an open reduction and internal fixation of the calcaneus performed since 2013. We report on the interim results of the adequacy of reduction and maintenance thereof and the incidence of wound complications. Follow-up was for a minimum of 6 weeks
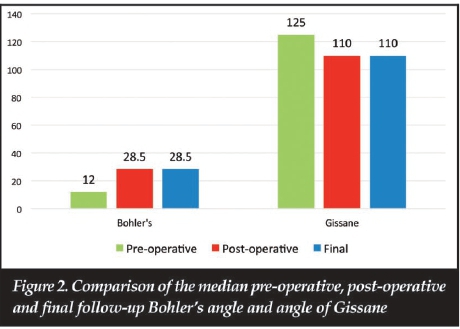
RESULTS: Twelve procedures were performed in this time. The Bohler's angle improved from a median of 12° pre-operatively to 28.5° (p=0.002) post-operatively. The angle of Gissane improved from a median of 125° to 110° (p=0.0001). Two patients had minor wound complications, both of which were managed without surgery, using dressings for 10 to 12 days
CONCLUSION: Open reduction and internal fixation of calcaneus fractures through a sinus tarsi approach allows adequate reduction with a low incidence of wound complications
Key words: calcaneus fracture, sinus tarsi approach, open reduction, internal fixation
Introduction
The calcaneus is the most frequently fractured tarsal bone. Up to 75% of calcaneus fractures are intra-articular.1 The optimal treatment for displaced intra-articular calcaneal fractures remains unknown.2 Buckley et al.3 performed a prospective, randomised, controlled multicentre trial, comparing operative with non-operative treatment of displaced intra-articular calcaneus fractures. They found no difference between the outcomes of the two groups, but in certain subgroups (women, those not seeking workers' compensation, and less severe injuries) those patients who had operative care fared better on functional scoring. The non-operative group was 5.5 times more likely to receive an arthrodesis. It has been shown that patients requiring a subtalar arthrodesis after a calcaneus fracture who had an open reduction and internal fixation have better functional scores than patients who had their fractures managed non-operatively.1 The operative group can be managed with an in-situ fusion compared to the non-operative group who often needs a debridement, osteotomy and bone block fusion, which is a more technically difficult procedure with more complications and worse functional results.1
The traditional extensile approach to the calcaneus provides excellent exposure, but has a high wound complication rate.4 This has led to the development of minimally invasive approaches with the sinus tarsi approach being the most commonly used." The approach is used to visualise the posterior facet and the calcaneocuboid joint and fixation is achieved by percutaneous screws6, K-wires7 or plates.8,9 One of the concerns with this approach is poor visualisation of the fracture and inadequate reduction, but adequate reduction, fewer wound complications and fewer iatrogenic sural nerve injuries have been reported with this approach.6,8-12 This approach has also been advocated in high risk patients such as diabetics, smokers, obese patients and patients with peripheral vascular disease.2,10
This approach has been used in our unit for two years and is not widely described in local literature. It should be stressed that the technique is challenging and requires a thorough understanding of fracture patterns and calcaneal anatomy and should be performed by experienced surgeons. The purpose of this study is to act as an interim study to assess our short- to intermediate-term results in terms of radiological adequacy of reduction and rate of wound complications.
Methods
Following institutional ethics approval, we performed a retrospective review of all patients who had an open reduction and internal fixation of their calcaneus performed through a sinus tarsi approach. Consecutive patients presenting with a displaced intra-articular articular fracture where the posterior facet was in less than three pieces (Sanders III or less) were included.
Unreconstructable Sanders IV fractures were managed with a primary reconstruction, subtalar fusion and not included in the study. We excluded any patient with a follow-up shorter than 6 weeks.
Specific data was collected, and included the Bohler's angle and the angle of Gissane of each patient as measured on the pre-operative, post-operative and last follow-up radiographs. Three of the authors measured these angles independently and an average value was used. Other data included the presence of wound complications, Sander's computed tomography classification, background history of diabetes and smoking, and standard demographic data.
The paired t-test was performed to analyse the difference between the pre-operative, post-operative and last follow-up radiographic angles. Significance was regarded as p<0.05.
Surgical technique (Figure 1)

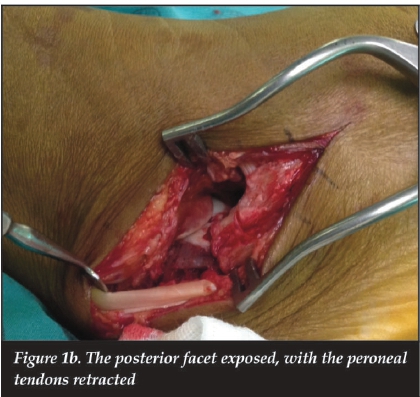

Surgery is performed with the patient supine with a bolster or sandbag under the buttock of the affected side. After administration of prophylactic antibiotics the tourniquet is inflated. An incision is made along a line drawn from the tip of the fibula to the base of the fourth metatarsal. The extensor digitorum brevis is then retracted to expose the anterior process and the posterior facet. At this stage the peroneal tendons can be inspected for dislocation and can be relocated if indicated through this approach. The calcaneo-fibular ligament is sectioned and using an elevator the posterior facet fragment is mobilised and reduced onto the susten-tacular fragment. This is then held in place with a K-wire. A percutaneous Steinman pin is inserted posteriorly through the tuberosity and is used to manipulate the tuberosity fragment under fluoroscopic guidance. An elevator is used to free the tuberosity from under the posterior facet and help mobilise it. In certain cases it may be necessary to manipulate the tuberosity fracture to achieve adequate reduction of the posterior facet. Once reduction is achieved, the Steinman pin is advanced into the articular fragment to maintain the reduction. An axial fluoroscopic view is obtained to confirm the tuberosity is out to length and out of varus or valgus.
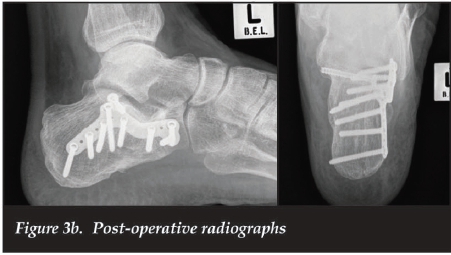
If required, the anterolateral fragment can then be reduced and is held in position with K-wires. Using a subchondral cannulated screw the posterior facet fragment is fixed to the sustentacular (constant) fragment. A full thickness pocket is created along the lateral wall towards the tuberosity to allow placement of the plate. Care must be taken to ensure the plate is placed lateral and not medial to the lateral wall. In all cases we used the Acumed® MINI-Calc® (Hillsboro, Oregon) plates. If the primary surgeon is concerned about a tongue-type component and feels the plate does not provide stable fixation, a percutaneous cannulated screw is placed across this fracture line. We do not use bone graft to fill the defect after reduction. The K-wires and Steinman pin are removed and the surgical site washed with sterile normal saline. The wound is closed in layers and the skin with non-absorbable sutures. The tourniquet is released and the foot placed in a well-padded below-knee posterior plaster splint. Postoperatively the patient's foot is elevated in the ward and once radiographs have been done and the patient can mobilise non-weight bearing the patient is discharged. At 2-week follow-up the wound is reviewed and the patient is placed in a moon boot. From 4 weeks the patient can start physiotherapy for subtalar and ankle range of motion. At 6 weeks partial weight bearing is allowed and from 8 weeks full weight bearing.
Results
Twelve patients were included; ten males and two females. There were nine smokers, one ex-smoker and in two patients the smoking status was not known. There were no diabetics, one psychiatric patient and one HIV-positive patient with a CD4 count of 331. All fractures were closed injuries. The median age was 38 (range 20-59) years. Median time to surgery was 10 (range 4-17) days with a median follow-up of 27.5 (range 6-82) weeks. Only two patients had a follow-up of less than 12 weeks. According to the Essex-Lopresti Classification there were
three tongue-type and nine joint depression fractures. On CT scan six cases were a Sanders II and six cases were a Sanders III. No peroneal tendon dislocations were noted. Only two (16.7%) cases had wound complications. One patient had a superficial wound dehiscence which settled with regular dressings and the other had superficial wound infection which settled with oral antibiotics for five days (Table 1). The median Bohler's angle changed from 12° (-5° to 44°) pre-operatively to 28.5° (19° to 36°) postoperatively (p=0.002) and was 28.5°(19° to 37°) at the last follow-up (p=0.101). The median angle of Gissane changed from 125° (94° to 139°) pre-operatively to 110° (102° to 117°) post-operatively (p=0.0001) and was 110° (104° to 125°) at final follow-up (p=0.288) at a median final follow-up of 27.5 weeks (Figure 2 and Table II). All the patients were walking unaided at the final reported follow-up. All patients followed up for 12 weeks were ambulating without assistance. There was no evidence of advance subtalar arthritis, although this might change with longer term follow-up.
Discussion
The traditional extensile approach to the calcaneus provides excellent exposure for fracture reduction, but at the cost of a high wound complication rate as well as greater risk to the sural nerve. The soft tissue flap needs significant retraction for visualisation of the posterior facet and the anterior process. This has led to the development of minimally invasive approaches, which have fewer wound complications, but there are concerns about sufficient exposure and adequacy of reduction. The primary goal of this study was to assess our adequacy of reduction at short-term follow-up. Better reduction of the height and width of the calcaneus as well as the posterior facet leads to better clinical results. If a fusion of the subtalar joint is required later, a far simpler procedure with better outcomes can be performed.1
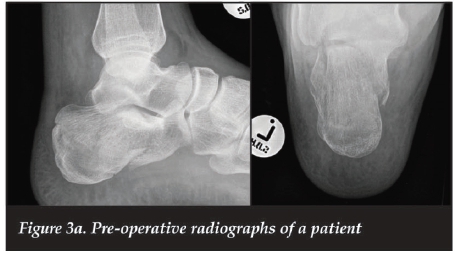
Pre- and post-operative radiographs of a patient are shown in Figure 3.
The general recommendation is to perform surgery within 2 weeks of the injury.2 After this the fracture becomes sticky and more difficult to reduce which could lead to consideration of the traditional extensile approach.
The sooner the surgery is performed, the easier it is to reduce the fracture with percutaneous techniques. With the small incision, operating through swollen tissue is less of a concern. There is more subcutaneous tissue over the sinus tarsi and the wound is not under tension after closure A large haemorrhagic fracture blister over the sinus tarsi or a contaminated open fracture would be the only soft tissue-related contraindications to operate early. The median time to surgery was 10 (4-17) days. This delay was attributable to the delay of referral from other hospitals, and the delay in obtaining adequate imaging and access to theatre time.
With the sinus tarsi approach we achieved sufficient exposure of the posterior facet. There was a significant improvement in Bohler's angle from a median 12° to 28° (p=0.002), which is within the 20° to 40° recommended in Rockwood and Green.13 The angle of Gissane also showed significant improvement from a median 125° to 110° (p=0.0001), even though this was still not within the 95° to 105° recommended in Rockwood and Green.13 Our results compare favourably with previous authors. Su et al.14 showed that restoration of the Bohler's angle leads to better functional results.
Nosewicz et al.6 in 2012 found that the sinus tarsi approach gave them sufficient exposure and they achieved an adequate restoration of calcaneal height and Bohler's angle. In 2013 Xia et al.8 assessed the outcomes of using the sinus tarsi approach with plate fixation and found an adequate radiographic reduction of calcaneal fractures. Kikuchi et al.9 showed a statistically significant improvement in Bohler's angle, but not in the angle of Gissane in their series of patients treated with fixation through a sinus tarsi approach. Kline et al.15 performed a retrospective review comparing the extensile approach to the sinus tarsi approach and found no difference in adequacy of reduction. In 2014 Xia et al.11 published their data on a randomised controlled trial comparing open reduction and internal fixation through an extensile approach to the sinus tarsi approach. They found no difference in adequacy of reduction. Meraj et al.12 achieved an adequate reduction in their series of fractures treated through a sinus tarsi approach.
We had a low incidence of wound complications. Only two patients (16.7%) required treatment with local dressings and antibiotics in one case. Both were males, one was a smoker and one an ex-smoker. The time to surgery was 17 days in one and 15 days in the other. Surgical times were not recorded, but it is possible that the longer time to surgery made reduction using indirect techniques more difficult, leading to longer surgical times. The wound complications were minor and required no further surgical intervention. This result is not as good as some other authors'. Xia et al. had no wound complications in their series." Kikuchi et al.9 had wound complications in 13.6% of their 22 fractures, but all were managed without surgical intervention. In a systematic review10 of calcaneal fractures treated through a sinus tarsi approach, wound complications were seen in 0% to 15.4% (average 4.8%) of cases. Kline et al.15 had wound complications in 29% of the extensile group and in only 6% in the sinus tarsi group.
Six Sanders II and six Sanders III calcaneal fractures were included in this study population. Most authors6-8,15 only included Sanders II and Sanders III fractures, with only Kikuchi et al9 including Sanders IV fractures. There was no statistical difference in the adequacy of reduction comparing Sanders II with Sanders III fractures.
Smoking and even a previous history of smoking is regarded as a risk factor for wound complications and would even be seen as a contraindication for surgery.16,17 Those advocating the use of the sinus tarsi approach would recommend it in high risk patients such as diabetics and smokers.2,9,10 Nine of our patients were smokers, one patient an ex-smoker and for two patients this data was not recorded. Of the two patients with wound complications, one was a smoker and one an ex-smoker, but the other seven smokers had no wound complications.
The limitations of this study is the small number of cases, the lack of a control group with the extensile approach and the short follow-up, but this serves as an interim study to assess the short-term results in terms of radiographic adequacy of reduction and short-term wound complications. With our current results we can now continue with recruiting more cases and will in future report on a bigger series with longer follow-up. Another limitation was not performing CT scans on all the patients post surgery to assess the quality of reduction. This was not possible with our resources and we had to rely on standard X-rays.
Conclusion
Open reduction and internal fixation of intra-articular calcaneus fractures through a sinus tarsi approach provides sufficient exposure of the posterior facet for adequate reduction without the risk of serious wound complications in even high-risk patients such as smokers.
Compliance with Ethics Guidelines
This research was approved by the University of Cape Town Department of Surgery Research committee (2015/010) and the University of Cape Town Faculty of Health Sciences Ethics Committee (HREC/REF: 142/2015).
P Jordaan, S Maqungo, S Roche, R Magampa and G McCollum declare that they have no conflict of interest, and received no funding for this research.
References
1. Radnay C, Clare M, Sanders R. Subtalar fusion after displaced intra-articular calcaneal fractures: Does initial operative treatment matter? The Journal of Bone and Joint Surgery American volume. 2009;91:541-46. [ Links ]
2. Hsu AR, Anderson RB, Cohen BE. Advances in surgical management of intra-articular calcaneus fractures. J Am Acad Orthop Surg. 2015;23(7):399-407. [ Links ]
3. Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures. The Journal of Bone and Joint Surgery American volume. 2002;84-A(10):1733-44. [ Links ]
4. Carr JB. Surgical treatment of intra-articular calcaneal fractures - A review of small incision approaches. J Orthop Trauma. 2005;19(2):109-17. [ Links ]
5. Zhang T, Su Y, Chen W, Zhang Q, Wu Z, Zhang Y. Displaced intra-articular calcaneal fractures treated in a minimally invasive fashion: longitudinal approach versus sinus tarsi approach. The Journal of Bone and Joint Surgery American volume. 2014;96(4):302-309. [ Links ]
6. Nosewicz T, Knupp M, Barg A, Maas M, Bolliger L, Goslings JC, et al. Mini-open sinus tarsi approach with percutaneous screw fixation of displaced calcaneal fractures: a prospective computed tomography-based study. Foot & Ankle International. 2012;33(10):925-33. [ Links ]
7. Ebraheim NA, Elgafy H, Sabry FF, Freih M, Abou-Chakra IS. Sinus tarsi approach with trans-articular fixation for displaced intra-articular fractures of the calcaneus. Foot & Ankle International. 2000;21(2):105-13. [ Links ]
8. Xia S, Wang X, Lu Y, Wang H, Wu Z, Wang Z. A minimally invasive sinus tarsi approach with percutaneous plate and screw fixation for intra-articular calcaneal fractures. International Journal of Surgery. 2013;11(10):1087-91. [ Links ]
9. Kikuchi C, Charlton TP, Thordarson DB. Limited sinus tarsi approach for intra-articular calcaneus fractures. Foot Ankle Int. 2013;34(12):1689-94. [ Links ]
10. Schepers T. The sinus tarsi approach in displaced intra-articular calcaneal fractures: a systematic review. International Orthopaedics. 2011;35(5):697-703. [ Links ]
11. Xia S, Lu Y, Wang H, Wu Z, Wang Z. Open reduction and internal fixation with conventional plate via L-shaped lateral approach versus internal fixation with percutaneous plate via a sinus tarsi approach for calcaneal fractures - a randomized controlled trial. International Journal of Surgery. 2014;12(5):475-80. [ Links ]
12. Meraj A, Zahid M, Ahmad S. Management of intra-articular calcaneal fractures by minimally invasive sinus tarsi approach-early results. Malaysian Orthopaedic Journal. 2012;6(1):13-17. [ Links ]
13. Bucholz RW, Heckman JD, Court-Brown CM, editors. Rockwood and Green's Fractures in Adults. 6 ed: Lippincott Williams & Wilkins; 2006. [ Links ]
14. Su Y, Chen W, Zhang T, Wu X, Wu Z, Zhang Y. Bohler's angle's role in assessing the injury severity and functional outcome of internal fixation of displaced intra-articular calcaneal fractures: a retrospective study. BMC Surgery. 2013;13(40):1-8. [ Links ]
15. Kline AJ, Anderson RB, Davis WH, Jones CP, Cohen BE. Minimally invasive technique versus an extensile lateral approach for intra-articular calcaneal fractures. Foot Ankle Int. 2013;34(6):773-80. [ Links ]
16. Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: Analysis of 190 fractures. J Orthop Trauma. 1999;13(5):369-72. [ Links ]
17. Buckley R, Tough S. Displaced intra-articular calcaneal fractures. J Am Acad Orthop Surg. 2004;12:172-78. [ Links ]
 Correspondence:
Correspondence:
Dr Graham McCollum
Department of Orthopaedic Surgery
H49 Old Main Building
Groote Schuur Hospital
Anzio Road
7925 Observatory, Cape Town
Email: grahammac@discoverymail.co.za














