Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.15 n.3 Centurion Aug./Sep. 2016
http://dx.doi.org/10.17159/2309-8309/2016/v15n3a2
TRAUMA
Short-term results of grade III open tibia fractures treated with circular fixators
Dr L NieuwoudtI; Dr N FerreiraII; Dr LC MaraisIII
IMBChB, H Dip Orth, FC Orth(SA), Department of Orthopaedic Surgery, Grey's Hospital, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
IIBSc, MBChB, FC Orth(SA), MMed(Orth), PhD, Department of Orthopaedic Surgery, Grey's Hospital, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
IIIMBChB, FCS Orth(SA), MMed(Orth), PhD, Department of Orthopaedic Surgery, Grey's Hospital, Nelson R Mandela School of Medicine, University of KwaZulu-Natal
ABSTRACT
Grade III open tibia fractures have previously been shown to have high infection and non-union rates, and the optimal treatment remains controversial. We present the short-term results of 94 consecutive Gustilo-Anderson grade III open tibia fractures, definitively treated with circular external fixators in this retrospective study. A total of 94 patients (80 males and 14 females), with a mean age of 36.5 years (range 8-73) were followed up for a mean period of 12 months (range 6-52). Deep infection occurred in four patients (4.3%) and non-union in three patients (3.2%). The mean time to union was 23 weeks (range 11-79). The prevalence of HIV infection was 32.9% and no statistically significant association between HIV infection and an increased risk of deep infection (p = 0.601) or nonunion (p = 0.577) could be demonstrated. Pin-site infection occurred in 16% with the majority being low-grade infections. The management of grade III open tibia fractures with definitive circular external fixation delivered promising short-term results with low complication rates in terms of infection and non-union.
Key words: tibia, open fracture, circular fixator, Ilizarov, non-union, HIV, infection
Introduction
The optimal treatment of Gustilo-Anderson Grade III open tibia fractures remains controversial.1-2 The tibia has a poor blood supply in the distal third and lacks muscular cover over the antero-medial border. This unforgiving soft tissue envelope and poor blood supply coupled with a propensity for high-energy trauma, increases the risk of infection and non-union in open tibia fractures. Non-union rates of 30% for intramedullary nailing and 40% for mono-lateral external fixators have been reported, while infection may occur in up to 40% of open diaphyseal tibia fractures.3
Preventing infection and achieving union and functional restoration are the fundamental principles in treating these fractures. How best to achieve these goals remains contentious; time to initiation of antibiotic therapy,4 timing of surgical debridement,5 timing of wound closure,6 duration of antibiotic cover,7 what type of dressing to use,8 timing and choice of fracture fixation,9-12 and the effect of HIV infection on the outcome of management13-18 have all been investigated in the literature.
Circular fixators are gaining popularity due to their minimally invasive application and inherent stability that allow early functional rehabilitation. In addition circular external fixation offers certain mechano-biological advantages that may promote bone formation.19 Mono-lateral fixators employ cantilever loading that can lead to shear forces at the fracture site, predisposing to fibrocartilage formation and non-union.20 Circular fixators use beam loading through tensioned fine wires to provide stability with high bending and translational rigidity while maintaining a degree of axial motion. These properties promote bone formation, making circular fixators ideal for complex fracture management.21,22
We report the short-term results of a retrospective series of Gustilo-Anderson grade III open tibia fractures treated with circular external fixation. In addition we investigate the effect of HIV infection on the incidence of deep infection and non-union following open tibia fractures.
Materials and methods
Between January 2008 and January 2015 all patients that presented to our institution with grade III open tibial fractures were eligible for evaluation. Inclusion criteria were patients with high-grade open tibia fractures who completed treatment with definitive circular external fixation. Patients were excluded if they did not complete at least six months' follow-up. Institutional ethics committee approval was obtained prior to commencement of this study.
All patients were treated according to a standardised treatment protocol, starting with emergency department antibiotic administration (cefazolin and aminoglycoside), wound irrigation and splinting (Figure 1). Subsequent urgent surgical debridement was performed in combination with temporary fracture stabilisation with a mono-lateral external fixator together with intra-operative classification according to Gustilo-Anderson23,24(Figure 2). At 48 hours a wound inspection and closure was performed by either delayed primary closure (grade IIIA), soft tissue flap or split skin graft (grade IIIB). All patients were offered voluntary counselling and testing for HIV during their hospital stay.


The temporary mono-lateral external fixator was converted to circular fixation within a period of two weeks, once the soft tissues had healed. Each circular fixator was individually designed and applied according to the specific fracture configuration. All frames were applied under the supervision of a consultant with limb reconstruction experience. The surgical technique followed meticulous pre-operative planning and involved the use of pre-constructed frames. For Ilizarov-type fine wire circular fixators a proximal reference wire was inserted parallel to the knee joint, followed by frame application and a distal reference wire parallel to the ankle joint. This aligned the fracture in the coronal plane. Sagittal plane alignment was achieved under fluoroscopy and all wires were tensioned to 130 kg. Fixation was completed through the application of at least two tensioned wires per ring.25
Hexapod external fixators were used in cases where acute fracture reduction was unsuccessful or where intentional fracture site deformity was used to facilitate soft tissue closure. These fixators were applied using the 'rings first' method entailing the independent, orthogonal application of the proximal and distal rings to each bone segment.26 The hexapod was completed by attaching six variable length struts between the rings. Post-operative radiographs were used for planning correction of any deformity, which was commenced once the soft tissues were deemed suitable.
Fractures involving segmental bone loss of more than 4 cm were treated with bone transport using a standard five-ring transport frame construct. Following a metaphyseal osteotomy, bone transport was performed at 0.25 mm four times per day. Formal docking procedures consisted of debridement of the fibrous tissue within the docking site and Phemister-type autograft.27 Fractures involving segmental bone loss of less than 4 cm were managed with acute shortening followed by subsequent lengthening through a metaphyseal osteotomy.
Fibular osteotomies were performed in cases where acute shortening was required, in bone transport cases once docking occurred, and if a tibia fracture was associated with an intact fibula. Under tourniquet and via a lateral approach, between the peroneal and soleus muscles, 10 mm of fibula was resected. Fascia and skin were closed in layers over a drain and the tourniquet deflated for the remainder of the operation.
Post-operatively, all patients were instructed to mobilise fully weight bearing before discharge and a standardised pin-site care regimen was followed28(Figure 3). Functional rehabilitation was encouraged under the guidance of a physiotherapist to facilitate early joint mobility and normalisation of gait pattern. Outpatient follow-up was scheduled at two-weekly intervals until a robust rehabilitation program was established. The importance of early transition from two to one or even no crutches was emphasised at each visit. Thereafter, the interval between follow-up appointments was increased to four weeks.

Radiological union was assessed by evidence of union of at least three out of four cortices. At this point, a staged 'trial of union' protocol was initiated by dynamisation of the external fixator. The site of the uniting fracture was manually stressed and if this did not cause any pain or deformity, the patient was instructed to bear weight. If the patient was able to walk without pain, they were allowed to return home with a fully dynamised frame and encouraged to mobilise, fully weight bearing, for a period of two weeks. Repeat radiographs were then compared with those before the trial of union; if no deformity had developed, union was deemed confirmed and the external fixator removed (Figure 4).

Deep infection was defined as an infection involving any tissue deep to the skin and subcutaneous tissue, including bone, at any point in time. Non-union was defined as no clinical or radiological evidence of union after a minimum of six months treatment. Pin-site infection was defined and classified according to the Checketts, Otterburn and MacEachern system.29 Statistical analysis of the results was undertaken using the chi-square test. A p-value of < 0.05 was considered to be statistically significant.
Results
Ninety-eight patients met the inclusion criteria. Two patients were excluded because they died of systemic complications of injuries sustained during polytrauma, which were unrelated to their tibia fractures. Two patients required amputation and were excluded. The first was a polytrauma patient with an irreparable vascular injury who refused initial amputation. He agreed to the amputation four weeks later. The second patient was undergoing bone transport for segmental bone loss and was unwilling to continue the reconstructive process. This patient requested amputation five months post-injury.
The final cohort comprised 80 men and 14 women with a mean age of 36.5 years (range 8 to 73 years) (Table I). Mean follow-up was 12 months (range 6 to 52). Diaphyseal fractures were seen in 78 (82%) patients; three patients had segmental fractures and the remaining 14 patients were equally divided into seven open plateau fractures and seven open plafond fractures. In total, 46 fractures (49%) were classified as Gustilo-Anderson IIIA and 48 (51%) as Gustilo-Anderson IIIB open fractures. Details of results are listed in Table I.

The mechanism of injury included motor vehicle accidents (n = 41), pedestrian vehicle accidents (n = 31), falls (n = 9), assaults (n=11) and motorcycle accidents (n=2). Forty-seven patients had associated injuries, illustrating the high-energy trauma that is often associated with these fractures (Table II).
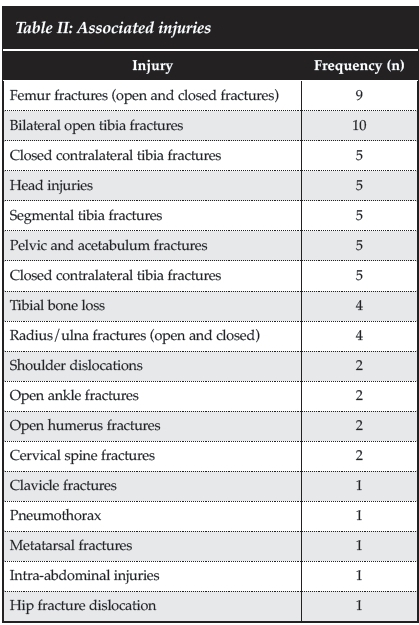
Medical co-morbidities were identified in five patients, including schizophrenia, previous cerebrovascular accident, pulmonary tuberculosis, hypertension and diabetes mellitus. HIV infection was found in 31 out of 94 (32.9%) patients with CD4 counts ranging from 82 to 1005 cells / mm3 (median = 347.8 cells/mm3). Seventeen patients (54.8%) were on highly active anti-retroviral treatment (HAART). Twenty-five (26%) patients were active smokers.
The majority of patients (82 out of 94) were treated in traditional Ilizarov-type fine wire circular external fixators. These included 49 TrueLok fixators (Orthofix, Verona, Italy) and 33 Ilizarov fixators (Smith & Nephew, Memphis, Tennessee). Hexapod external fixators were used in 12 patients and consisted of seven Taylor Spatial Frames (Smith & Nephew, Memphis, Tennessee) and five TrueLok-Hex fixators (Orthofix, Verona, Italy). The median duration of external fixator treatment was 26.5 weeks (11 to 79). Three patients underwent planned bone grafting as part of a formal docking procedure following bone transport. One patient had acute shortening at the time of initial debridement and required limb lengthening to equalise leg lengths.
Deep infection developed in four out of 94 (4.25%) cases. One patient with a grade IIIA and three patients with grade IIIB injuries developed deep infection. Three infections developed following diaphyseal fractures while the remaining infection occurred after a meta-diaphyseal fracture of the distal tibia. Two patients united in the presence of sepsis and two developed infected non-unions. One patient with an infected non-union was treated by debridement and bone transport while the other refused any further surgical management. There was no statistically significant difference between infection rates in grade IIIA and IIIB injuries (p = 0.617). Two of the four deep infections occurred in HIV-positive individuals. There was no statistically significant association between HIV status and the development of deep infection (p = 0.601). No superficial infection cases were reported.
Non-union occurred in three out of 94 (3.2%) patients. All three non-unions developed after grade IIIB open diaphyseal fractures in HIV-negative individuals. These included two patients who sustained open fractures with segmental bone loss and one patient who was an active smoker.
Both patients with segmental bone loss were treated with circular external fixator bone transport. The third patient was treated with hexapod closed distraction of their stiff hypertrophic non-union. There was no statistically significant association between the initial injury classification (p = 0.117) or HIV status (p = 0.577) and the development of a non-union.
Pin-site infection was the most common complication and occurred in 15 of 94 (16%) cases. The majority of these infections were minor grades according to the Checketts, Otterburn and MacEachern classification and responded well to local pin-site care and oral antibiotics.29 Two patients developed major pin-site infections and were treated with local hydrosurgical debridement with no further infection noted on follow-up. Other complications included one ankle equinus contracture, one knee flexion contracture and five mal-unions of less than 10°.
Discussion
Grade III open tibia fractures are high-energy injuries with extensive soft tissue damage and bony comminution, and are often contaminated. Complications are common following these injuries, with deep infection and nonunion being the most prevalent. The optimal treatment of open tibia fractures remains to be established. In this study we set out to determine the short-term result of the treatment of Grade III open tibia fractures with circular external fixation. In addition we examined the influence of HIV infection on the incidence of infection and non-union.
Deep infection is an important complication following open fractures. Incidences of between 11% and 38% have been quoted following grade III open tibia fractures.30-38 This is as a result of the high-energy transfer associated with these injuries that frequently result in devitalisation of tissues. Early administration of antibiotics,4 adequate debridement39 and early wound cover40 have all been shown to decrease the incidence of infective complications. A recent review by Dickson et al. compared deep infection rates following severe open tibia fractures across multiple publications and treatment modalities. They reported deep infection rates of 0.9% in 420 patients treated in circular fixators, compared with 11% in 492 patients treated with plate fixation, 10.7% in 625 patients treated with mono-lateral external fixators, 8.7% in 547 patients treated with reamed nailing, and 7.1% in 1 223 patients who were treated with unreamed nails.41 The difference in deep infection rates between circular fixators and these other fixation methods was found to be statistically significant. (p < 0.001) Deep infection occurred in 4.25% of cases in our series and compares favourably to the published results of other treatment modalities.
Non-union is particularly prevalent following open tibia fractures.42 Gaebler et al. found that grade III open fractures were five times more likely to develop delayed union compared to closed, grade I and grade II fractures.43
In a review of 104 patients, Karladani et al. reported a relative risk of 8.2 for developing non-union in open fractures.44 Gaston et al. reviewed 100 patients with tibial shaft fractures. They also reported a higher risk of non-union after open fractures with a relative risk of 3.4.45 The use of definitive circular fixation in these injuries also has a potential benefit in this regard. These devices can be applied with minimal disruption of soft tissues and preservation of biological potential at the fracture site. The biomechanical properties of circular fixators result in a high bending and translational rigidity while maintaining a degree of axial motion at the fracture site.19 This aids in creating a local milieu that is conducive to bone formation and fracture union. Dickson et al. also compared union rates after severe open fractures across multiple publications and treatment modalities. They found 98.6% union in 420 patients treated in circular fixators, compared with 83.1% in 492 patients treated with plate fixation, 89.3% in 625 patients treated with mono-lateral external fixators, 93.3% in 547 patients treated with reamed nailing, and 92.6% in 1 223 patients who were treated with unreamed nails.41 The difference in union rates between circular fixators and these other fixation methods was found to be statistically significant (p < 0.001). Union was achieved in 96.8% of cases in our series and supports the findings of the abovementioned review.
The effect of HIV infection on open fracture outcome is controversial, with conflicting evidence on infective complications and non-union rates.13-18 Open fractures in particular appear to have an increased risk of non-union in HIV-positive individuals. Chandanwale et al. reported a significantly increased risk for non-union after open fractures in HIV-positive patients treated with mono-lateral external fixation (50% vs. 15%).17 Aird et al. reported a nonunion risk of 15% in HIV positive patients compared with 4% in HIV negative patients with open fractures treated with mono-lateral external fixators.46 Gardner et al. contradicted these findings and concluded that HIV did not increase the risk of non-union with internally fixed fractures. Their cohort however included only five open fractures.47 Our series found no statistically significant association between HIV infection and non-union after grade III open tibia fractures. (p = 0.577) In terms of infection, Harrison et al. reported a statistically significant (p = 0.020) increased risk for infection after open tibia fractures treated with monolateral external fixation.15 Bates et al. found no significant difference in the rate of infection between HIV positive and HIV negative patients with open or closed fractures in his study of internally fixed fractures.48 Hao et al. reported that HIV infection did not correlate with a higher risk for postoperative infection with the use of internal fixation.49 Aird et al. concluded that HIV was not a significant risk factor for acute implant infection after open fractures.46 Our series found no statistically significant risk for deep infection in HIV-positive patients who sustained grade III open tibia fractures (p = 0.601). This could be due to a significant number of patients being on HAART (54.8%) compared to the study by Harrison et al. that had no patients on HAART.
There are several limitations of this study including a retrospective design, single-centre cohort and lack of a control group. Our study was also underpowered to draw strong conclusions regarding the effect of HIV status on deep infection or non-union following these injuries. Future research aimed at investigating this further is currently underway.
Conclusion
Definitive circular external fixation of grade III open tibia fractures provides excellent short-term results with low infection and non-union rates. HIV infection did not appear to be associated with an increased risk for deep infection or non-union.
Acknowledgement
I would like to thank Dr R Rodseth PhD for his contribution to this study.
Compliance with Ethics Guidelines
Institutional ethics committee approval was obtained prior to commencement of this study.
Luan Nieuwoudt, Nando Ferreira and Len Marais declare that they have no conflict of interest.
Additional informed consent was obtained from all patients for which identifying information is included in this article.
References
1. O'Brien CL. Controversies in the management of open fractures. Open Orthop J 2014;8(Suppl 1:M7):178-84. [ Links ]
2. Ryan SP, Pugliano V. Controversies in initial management of open fractures, Scand J Surg. 2013;103:132-37. [ Links ]
3. Webb LX, Bosse MJ, Castillo RC, MacKenzie EJ. Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Joint Surg[Am]. 2007;89A:923-28. [ Links ]
4. Lack WD, Karunaker MA, Angerame MR, Seymour RB, Sims S, Kellam JF, Bosse MJ. Type III open tibia fractures: Immediate antibiotic prophylaxis minimizes infection. J Orthop Trauma. 2015 Jan;29(1):1-6. [ Links ]
5. Namdari S, Baldwin KD, Matuszewski P, et al. Delay in surgical debridement of open tibia fractures: An analysis of national practice trends. J Orthop Trauma. 2011;25: 140-44. [ Links ]
6. Gopal S, Majumder S, Bathelor AGB, Knight SL, De Boer P, Smith RM. Fix and flap: The radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg [Br]. 2000;82-B: 959-66. [ Links ]
7. Dunkel N, Uçkay I, Macedo M, Pittet D. Short duration of antibiotic prophylaxis in Gustilo grade III open extrem ities fractures does not enhance risk of subsequent infection. 50th Interscience Conference on Antimicrobial Agents and Chemotherapy, Boston, September 2010 (Abstract). In press. [ Links ]
8. Schlatterer DR, Hirschfeld AG, Webb LX. Negative pressure wound therapy in grade IIIB tibial fractures: fewer infections and fewer flap procedures? Clin Orthop Relat Res. 2015 May;473(5):1802-11. [ Links ]
9. Tornetta P, Bergman M, Watnik N, Berkowitz G. Treatment of grade IIIB open tibial fractures: A prospective randomized comparison of external fixation and unreamed locked nailing. J Bone Joint Surg [Br]. 1993: 75-B:13-19. [ Links ]
10. Almazedi B. Intramedullary nailing versus external fixation for the treatment of grade III open tibial fractures. J Bone Joint Surg (Br). 2011 vol.93-B no.SUPP III 310. [ Links ]
11. Stanton T. Plating vs. external fixation for open tibia fractures. AAOS Now. December 2014 Issue. http://www.aaos.org/news/aaosnow/dec14/clinical1.asp. [ Links ]
12. Xiao Fang, Lei Jiang, Ying Wang, Liangyu Zhao, Med Sci Monit. Treatment of Gustilo grade III tibial fractures with unreamed intramedullary nailing versus external fixator: A meta-analysis. 2012; RA49- RA56. PMCID: PMC3560815. [ Links ]
13. Hoekman P, Van Den Perre P, Nellisen J, Kwisanga B, Bogaerts J, Kanyangabo F. Increased frequency of infection after open reduction of fractures in patient who are seropositive for human immunodeficiency virus. J Bone Joint Surg Am 1991;73-A(5):675-79. [ Links ]
14. Jellis JE. Orthopaedic surgery and HIV disease in Africa. Int Orthop. 1996;20:253-56. [ Links ]
15. Harrison WJ, Lewis CP, Lavy CBD. Wound healing after implant surgery in HIV-positive patients. J Bone Joint Surg Br. 2002;84-B:802-806. [ Links ]
16. Harrison WJ, Lavy CBD, Lewis CP. One-year follow-up of orthopaedic implants in HIV-positive patients. Int Orthop. 2004;28:329-32. [ Links ]
17. Chandanwale A, Nawale S, Bhosale S, Jadhav S, Anantraman C. Fracture healing rate in HIV positive patients in India. XVI International AIDS conference. 2006. Toronto, Ontario. [ Links ]
18. Harrison WJ, Lewy CP, Lavy CBD. Open fractures of the tibia in HIV positive patients: a prospective controlled single-blind study. Injury. 2004;34:852-56. [ Links ]
19. Podolsky A, Chao EY, Mechanical performance of Ilizarov circular fixators in comparison with other external fixators. Clin Orthop Relat Res. 1993;293:61-70. [ Links ]
20. Cunningham JL. The biomechanics of fracture fixation. Current Orthopaedics. 2001;15:457-64. [ Links ]
21. Caja VJ, Kim W, Larsson S, Chao EYS. Comparison of the mechanical performance of three type of external fixators: linear, circular and hybrid. Clin Biomech. 1995;10:401-406. [ Links ]
22. Bronson DG, Samchukov ML, Birch JG, Browne RH, Ashman RB. Stability of external circular fixation: a multi variable biomechanical analysis. Clin Biomech. 1998;13:441-48. [ Links ]
23. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analysis. J Bone Joint Surg Am. 1976;58:453-58. [ Links ]
24. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fracture. J Trauma. 1984;24:742-46. [ Links ]
25. Ferreira N, Mare PH, Marais LC. Circular external fixator application for midshaft tibial fractures: Surgical technique. SA Orthop J. 2012;11(4):39-42. [ Links ]
26. Taylor JC. Correction of general deformity with the Taylor Spatial Fixator. Jcharlestaylor.com [ Links ]
27. Phemister DB. Treatment of ununited fractures by onlay bone grafts without screw or tie fixation and without breaking down of the fibrous union. J Bone Joint Surg [Am]. 1947:29(4):946-60. Pubmed PMID: 20270359 [ Links ]
28. Ferreira N, Marais LC. Prevention and management of external fixator pin track sepsis. Strat Traum Limb Recon. 2012;7(2):67-72. PubMed PMID: 22729940. Pubmed Central PMCID: 3535127 [ Links ]
29. Checketts RG, Otterburn M, MacEachern G. Pin track infection: definition, incidence and prevention. Int J Orthop Trauma. 1993;3(suppl):16-18. [ Links ]
30. Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281-89. [ Links ]
31. Yokoyama K, Uchino M, Nakumura K, Ohtsuka H, Suzuki T, Boku T, Itoman M. Risk factors for deep infection in secondary intramedullary nailing after external fixation for open tibial fractures. Injury. 2006;37:554-60. [ Links ]
32. Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson BM, McCarthy ML, Travison TG, Castillo RC. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347: 1924-31. [ Links ]
33. MacKenzie EJ, Bosse MJ, Pollak AN, Webb LX, Swiontkowski MF, Kellam JF, Smith DG, Sanders RW, Jones AL, Starr AJ, McAndrew MP, Patterson BM, Burgess AR, Castillo RC. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg Am. 2005;87:1801-809. [ Links ]
34. Bednar DA, Parikh J. Effect of time delay from injury to primary management on the incidence of deep infection after open fractures of the lower extremities caused by blunt trauma in adults. J Orthop Trauma. 1993;7:532-35. [ Links ]
35. Harley BJ, Beaupre LA, Jones CA, Dulai SK, Weber DW. The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. J Orthop Trauma. 2002;16:484-90. [ Links ]
36. MacKenzie EJ, Bosse MJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders R, Jones AL, McAndrew MP, Patterson B, McCarthy ML, Rohde CA; LEAP Study Group. Factors influencing the decision to amputate or reconstruct after high-energy lower extremity trauma. J Trauma. 2002;52:641-9. Erratum in: J Trauma. 2002;53:48. [ Links ]
37. Bosse MJ, McCarthy ML, Jones AL, Webb LX, Sims SH, Sanders RW, MacKenzie EJ; The Lower Extremity Assessment Project (LEAP) Study Group. The insensate foot following severe lower extremity trauma: an indication for amputation? J Bone Joint Surg Am. 2005;87: 2601-608. [ Links ]
38. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Curr Orthop Practice. June 1989. [ Links ]
39. Giannoudis PV, Papakostidis C, Roberts C. A Review of the management of open fractures of the tibia and femur. J Bone Joint Surg (Br). March 2006;88-B(3):281-89. [ Links ]
40. Reuss BL, Cole JD. Effect of delayed treatment on open tibial shaft fractures. Am J Orthop. 2007;36(4):216-20. [ Links ]
41. Dickson DR, Moulder E, Hadland Y, Giannoudis PV, Sharma HK. Grade 3 open tibial shaft fractures treated with a circular frame, functional outcome and systematic review of literature. Injury. 2015;46:751-58. [ Links ]
42. Bhandari M, Guyatt GH, Swiontkowski MF, Schemitsch EH. Treatment of open fractures of the shaft of the tibia. A Systematic overview and meta-analysis. J Bone Joint Surg [Br] 200;82-B;62-68. [ Links ]
43. Gaebler C, Berger U, Schandelmaier P, Greitbauer M, Schauwecker HH, Applegate B, Zych G, Vecsei V. Rates and odds ratios for complications in closed and open tibial fractures treated with unreamed, small diameter tibial nails: a multicenter analysis of 467 cases. J Orthop Trauma. 2001;15(6):415-23. PubMed PMID: 11514768 [ Links ]
44. Karladani AH, Granhed H, Karrholm J, Styf J. The influence of fracture etiology and type on fracture healing: a review of 104 consecutive tibial shaft fractures. Arch Orthop Trauma Surg. 2001;121(6):325-28. PubMed PMID: 11482464. [ Links ]
45. Gaston P, Will E, Elton RA, McQueen MM, Court-Brown CM. Fractures of the tibia. Can their outcome be predicted? J Bone Joint Surg [Br]. 1999;81(1):71-76. PubMed PMID: 10068007. [ Links ]
46. Aird J, Noor S, Rollinson P. Is fracture healing affected by HIV in open fractures? J Bone Joint Surg [Br]. 2012; 94-B(SUPP XIX):16. [ Links ]
47. Gardner RO, Bates JH, Ng'oma E, Harrison WJ. Fracture union following internal fixation in the HIV population. Injury. 2013;44(6):830-3. PubMed PMID: 23267724. [ Links ]
48. Bates J, Mkandawire N, Harrison WJ. The incidence and consequence of early wound infection after internal fixation for trauma in HIV-positive patients. J Bone Joint Surg [Br]. 2012;94-B(9):1265-70. [ Links ]
49. Hao J, Herbert B, Quispe JC, Cuellar DO, Chadayammuri V, Kim JW, Young H, Hake ME, Hammerberg ME, Hak DJ, Mauffrey C. An observational case series of HIV-positive patients treated with open reduction and internal fixation for a closed lower extremity fracture. Eur J Orthop Surg Traumatol. 2015;25:815-19. [ Links ]
 Correspondence:
Correspondence:
Dr Luan Nieuwoudt
Department of Orthopaedic Surgery
Grey's Hospital
Nelson R Mandela School of Clinical Medicine
University of KwaZulu-Natal
3200 Pietermaritzburg
South Africa
Tel: +27 33 897 3000
Email: luanndt@hotmail.com














