Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.15 n.2 Centurion May./Jun. 2016
Expert opinion on published articles
Reviewer: Dr MN Rasool
Department of Orthopaedics
University of KwaZulu-Natal
Tel: (031) 260 4297
The medial epicondyle - ulnar nerve relation with various elbow positions in healthy children
Y Yildrum, M Bawameh, T Balikci and H Bal H
Journal of Pediatric Orthopaedics 2014;34:437-40
The treatment of displaced supracondylar fractures of the humerus in children continues to stimulate interest in the literature. Closed reduction and percutaneous pinning with crossed K-wires has gained support as the preferred method of treatment. Iatrogenic ulnar nerve injury remains a concern. An incidence of 2%-3% has been reported in a few studies in the literature. The dynamic changes that occur in the cubital tunnel during flexion and extension of the elbow are worthwhile knowing as these changes may help to prevent injury to the ulnar nerve during medial pinning.
Yildrum et al. studied the position of the ulnar nerve relative to the medial epicondyle in healthy children (4-12 years), bilaterally, with high resolution ultrasonography, with elbow flexion and rotation manoeuvres which are commonly performed during routine reduction of supra-condylar fractures. The elbow was gradually flexed, and the forearm was alternately placed in pronation and supination. The medial epicondyle-ulnar nerve distance was measured with various positions of the elbow and forearm. Seventy-six elbows were studied (mean age ± 8 years). The ulnar nerve translated anteriorly towards the medial epicondyle with increasing elbow flexion. Using specially designed angle adjustment orthotics, the increments in flexion were recorded.

The mean medial epicondyle-ulnar nerve distance that was 3.7 mm in an extended elbow decreased to 1.1 mm with full elbow flexion. Placement of the forearm in either supination or pronation did not produce a statistically significant difference. The authors concluded that flexion of the elbow brings the ulnar nerve close to the medial epicondyle independent of forearm rotation. The decrease in medial epicondyle-ulnar nerve distance up to 1.1 mm in a fully flexed elbow might be a factor that endangers the nerve during medial pinning in supracondylar fractures.
The above article adds knowledge to the dynamic changes in the position of the ulnar nerve in the cubital tunnel which is crucial to prevent injury following medial pin placement. Biomechanical studies with the elbow in flexion and extension have been shown in previous reports to alter the capacity of the cubital tunnel. With the elbow in flexion, the aponeurosis overlying the ulnar nerve (cubital tunnel retinaculum) is stretched, thereby decreasing the capacity of the cubital tunnel. Placing a medial K-wire through the retinaculum in this position constricts the nerve thereby preventing the nerve from returning to its relaxed position on extension of the elbow.
The possibility of a subluxing or hypermobile ulnar nerve should also be considered before pinning, by examining the opposite elbow. The subluxed nerve can be pinned during flexion of the elbow. Ulnar nerve injury can be prevented by using lateral pins, visualisation of the nerve through a small incision, avoiding placement behind the medial epicondyle, acute angulation of the pin and skin tethering with the wire. With the anterior translation of the nerve in flexion, some authors have suggested placing the lateral pin first and then extending the elbow fully to place the medial wire. Others suggest pinning the fracture in 50°-70° of flexion. We have used 90° of flexion with crossed K-wires, the medial pin at 45°, slightly anteriorly on the medial epicondyle, successfully.
The above article admits that the study was not done on injured elbows and clinical studies are required to verify the accuracy of sonography in the fractured elbow. Sonography permits dynamic observation of the ulnar nerve intra-opera-tively before placement of the medial pin to prevent iatro-genic injury. A thorough clinical examination before and after pinning should be emphasised.
Reviewer: Dr ICM Robertson
Dept of Orthopaedics
Tygerberg Hospital
Private Bag X3
Tygerberg, Cape Town
Tel: 021 938 5458
Long-term patient-reported outcome after fractures of the clavicle in patients aged 10 to 18 years
PH Randsborg, HF Fuglesang, JH Rotterud, OL Hammer, EA Sivertsen
Journal of Pediatric Orthopaedics 2014;34(4):393-99
An increasing trend to treat clavicle fractures in adolescents by open reduction and internal fixation has recently been documented in the literature.1 This probably follows reports that advocate the operative treatment of certain middle third clavicle fractures in adults.2 In keeping with these trends, I am sometimes asked what my approach is to clavicle fractures in older children and adolescents. The article under review is the most recent outcome study in this respect and has offered some insight.
As the title suggests, the purpose of the study was to determine the long-term outcome after a clavicle fracture in older children and adolescents. The study has merit in that it was a patient-reported outcome study. The authors conducted a retrospective review of 185 patients aged 10 to 18 years (median age 14.4 years) treated at their institution with an isolated clavicle fracture. Thirteen had lateral fractures and 172 had midshaft fractures.
Outcomes were assessed using the Oxford Shoulder score (OSS), the Quick version of the Disability of Arm, Shoulder and Hand questionnaire (Quick-DASH score) and a Visual Analog score for pain, cosmesis and overall satisfaction. Of the midshaft fractures, 122 patients (70.9%) responded to the questionnaires. Of the lateral fractures, 8 patients (61.5%) responded to the questionnaires. The mean age of the respondents was 18.7 years and this was at an average of 4.7 years after injury.
Sixty-five midshaft fractures were displaced. Nine of these displaced midshaft fractures were treated surgically. Seven were operated on as primary treatment; however, the actual indication for surgery in these cases was not stated. An additional patient was operated at 23 days for increasing pain and displacement, and another because of symptomatic nonunion at 163 days. The nine operated fractures did not have any difference in terms of initial shortening, displacement or angulation compared to the non-operative group. Of the nine operated patients, six had local irritation which prompted plate removal. One had a disfiguring scar and one complained of decreased sensation distal to the incision.
No patient with a lateral fracture was treated surgically. Of the lateral fracture group of patients at follow-up, one complained of general shoulder discomfort and one of pain while carrying a backpack.
With respect to the overall patient-reported outcomes, 95 per cent of the respondents with conservatively managed fractures reported good to excellent outcomes on both the OSS and Quick-DASH score. However, in the group of midshaft fractures managed non-operatively, shortening of the fracture had a small but statistically significant negative effect on the OSS, cosmetic and overall satisfaction scores.
The degree of angulation and displacement had no effect on the outcome scores in this group.

The authors' opinion was that the overall functional result after non-operatively treated clavicle fractures was good to excellent for most patients. The inferior result associated with shortening was small and most likely of limited clinical significance. The authors also note that nonunion of the clavicle at this age is very rare and therefore cannot be used as an argument to justify operative treatment.
The level of evidence in this study is low, with a high rate of non-responders. The number of operative cases was too small to provide an acceptable comparative group. However, the results support earlier literature3,4 with regards to good functional outcomes of non-operatively treated clavicle fractures in children and adolescents.
We must take cognisance of the available literature, and it is for this reason that I continue to advocate non-operative management as the mainstay of treatment in this age group. I support the authors' recommendation to reserve operative treatment for fractures with absolute indications such as threatened skin integrity, open fractures or associated neurovascular injuries. Whether other selected cases will benefit from operative treatment still needs to be defined.
References
1. Yang S, Werner BC, Gwathmey FW, Jr. Treatment trends in adolescent clavicle fractures. J Pediatr Orthop. 2015;35(3): 229-33. [ Links ]
2. Canadian Orthopaedic Trauma S. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1-10. [ Links ]
3. Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg Am. 2013;95(13):1159-65. [ Links ]
4. Bae DS, Shah AS, Kalish LA, Kwon JY, Waters PM. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop. 2013;33(5):544-50. [ Links ]
Reviewer: Dr MT Ramokgopa
Department of Orthopaedic Surgery
University of the Witwatersrand
Tel: 011 717-1000
Multicenter randomized clinical trial of non-operative versus operative treatment of acute acromio-clavicular joint dislocation
The Canadian Orthopaedic Trauma Society
Journal of Orthopaedic Trauma November 2015;29(11)
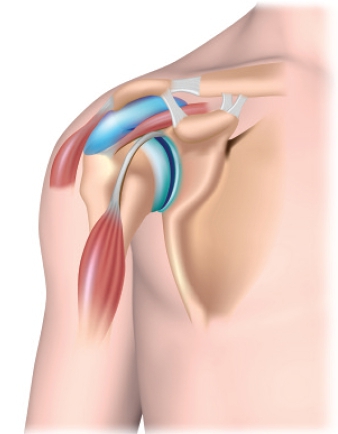
The article under review is a new addition to the ongoing debate on the controversial topic of operative versus non-operative management of the 'high grade' or complete dislocation of the acromio-clavicular joint.
The Canadian Orthopaedic Trauma Society undertook a Therapeutic Level I, prospective, randomised and multi-centre study over a period of 24 months. The study was spread over 11 hospitals with a total of 83 patients being randomised.
This study took place against the backdrop of the previous numerous reports that suggested that there was not much difference in the final outcome between the surgical and non-surgical treatment of the Rockwood types III, IV and V injuries.
The gaps that inspired the replication of this study were identified as:
1. The reviewed orthopaedic literature that was found to be limited to surgeon-based outcomes instead of validated outcome measures.
2. Most studies used outdated and inferior surgical fixation methods.
3. They also lacked statistical power.
4. Some of the research methods used were flawed.
For the purposes of this study, the modern and superior biomechanically proven 'hook plate' fixation was used in the 40 operated patients. The rest were treated conservatively with a sling support and analgesics, and followed by physiotherapy rehabilitation. A proper study design with appropriate ethics committee approvals, informed consent, sample size calculation, independent radiographs assessor and patients' randomisation with clear inclusion and exclusion criteria was employed.
The goals of this research were seen as the following:
1. To define predictive factors for both conservative and surgical care
2. To define the role of surgery
3. To provide the practising orthopaedic surgeon with evidence-based decision-making tools
The outcome measures used included:
1. The DASH Score - Disabilities of the Arm, Shoulder and Hand
2. Constant Score
3. Radiographic evaluation
All the above were assessed at 6 weeks and 3, 6, 12 and 24 months.
The outcome of this research revealed the following:
1. The patients' demographics and mechanisms of injury were similar.
2. The DASH and Constant Scores were almost similar.
3. The X-rays were much better in the operated group with the best anatomical reduction - assessed from the acromio-clavicular joint reduction and the coraco-clavicular distance.
4. The re-operation rate was more prevalent in the operated group.
5. The non-operated group returned to work earlier.
6. The persistently displaced distal clavicle in the non-operated group was cosmetically unacceptable.
The identified complications in the surgical group were: plate loosenings, acromial erosions, clavicular fracture, stiff shoulder, deep wound infection and numbness. The conservative group showed the persistent lateral clavicular end protrusion with soft tissues tethering as well as heterotopic ossification.
A list of key conclusions emerged from this study, namely:
1. The treatment of the high-grade acromio-clavicular joint disruption remains controversial.
2. The study provided valuable insight into the natural history of acute acromio-clavicular dislocations.
3. The modern hook plate design was found to result in good anatomical reductions with horizontal and vertical stability and good shoulder function. It is also a reproducible technique.
4. Surgery was however not superior to non-operative treatment in many respects. The conservative group rehabilitated much earlier.
This study has added more substance to the better understanding and reinforcement of the current approach and treatment of this common, often difficult and controversial injury. The main criticism, also conceded by the authors, is that the sample size may be too small to make very firm conclusions.
However, it is heartening in that the study is a follow-up to the previous reputable Cochrane (2010) and Knut Beitzel et al. systematic reviews (2013) that reached similar conclusions on the approach and treatment of the injuries under discussion.
The Cochrane reviews identified the three relevant and critical clinical trials that involved a larger grouping of 174 patients. Two of those trials were randomised and the one was quasi randomised. None of them used the validated measures for assessing the functional outcomes.
Furthermore, the lesser superior methods of fixation in the form of coraco-clavicular screws, acromio-clavicular pins and slings were used. The clinical evidence was found to be insufficient.
The 20 studies subjected to Beitzel et al.'s systematic review identified the 162 different techniques for the surgical treatment of the acromio-clavicular joint dislocation matched against the conservative measures. Three considerations regarding treatment were made. These were operative versus non-operative (14), early versus late treatment (4) and anatomic versus non-anatomic (2) treatment. Again, the authors concluded that there was lack of evidence to support the treatment options for the patients with acromio-clavicular joint dislocation.
Emilio Calvo et al. (2006) reported a retrospective analysis of 43 patients in which he identified acromio-clavicular joint anatomic reduction-related osteoarthritis and coraco-clavicular joint ossification in some of the 32 patients treated operatively. The group recommended conservative management.
There are several other concurring published reviews regarding this same topic that are worth reading such as Imatani (1975), Bannister (1983), Hootman (2004), Bäthis (2000), Ceccarelli (2008).
The opposing spectrum would include Horn (1954) who raised the problem of shoulder fatigue from the non-attached muscles whereas Kessel (1982) on the other hand alluded to the painful subluxation in the non-operated patient.
From the article under review and backed by the papers quoted and especially Cochrane reviews in particular, there are both clinical and research implications. First the implications for clinical practice are the following:
1. There is no proof that there are long-term benefits from surgery.
2. Surgery is associated with complications.
3. There is concern about the long stay from work following surgery.
4. There is a hospitalisation factor with surgery.
5. Conservative management seems to be the preferred option.
6. Selected patients may benefit from surgery, such as professional athletes and labourers. Treatment must be adapted to the patient's demands.
For the research the implications are:
1. Further well-designed research in this area is justified.
2. Larger, multicentre trials with better standardisation, especially with the appropriate outcome measures, are required.
3. Comparison between conservative treatment and minimally invasive arthroscopic surgery or other modern fixation methods is needed.














