Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.15 no.2 Centurion may./jun. 2016
http://dx.doi.org/10.17159/2309-8309/2016/v15n2a5
SPINE
Debilitating sciatica following a sacral fracture: A case report
Dr Anria HornI; Dr Antony ThomasII; Professor Robert DunnIII
IMBChB(Pret), FC Orth(SA), MMed(Orth)(UCT) Registrar, Orthopaedic Surgery, Groote Schuur Hospital, Cape Town
IIMBBS(Mangalore), MMed(Neurosurgery)(Wits) AOSpine Observer, Orthopaedic Surgery, Groote Schuur Hospital, Cape Town
IIIMBChB(UCT), FCS (SA)Orth, MMed(UCT)Ortho Consultant Spine and Orthopaedic Surgeon, Professor and Head of Department of Orthopaedic Surgery, University of Cape Town, Groote Schuur and Red Cross Children's Hospitals
ABSTRACT
Following a horse-riding accident, a 16-year-old female sustained a minimally displaced sacral fracture extending into the S1 and S2 foramina on the left. The patient was initially treated conservatively but neuropathic pain, dysaesthesia and weakness in the L5 and S1 distributions developed and persisted. CT and MRI revealed a fracture fragment abutting the L5 nerve root. Epidural anaesthesia and aggressive neural mobilisation by physiotherapy failed to improve symptoms. Surgical decompression via the sub-iliacus approach was then performed 6 weeks following the injury. Symptoms resolved immediately but recurred in the L5 distribution, presumably due to neuritis, and were successfully managed conservatively. Six weeks following surgery, all symptoms had resolved and the patient mobilised independently and returned to her pre-injury level of activity.
Key words: sacral spine, sacral fracture, sciatica, surgery for sacral fractures
Introduction
The optimal treatment for sacral fractures is dependent on the radiographic fracture pattern and the presence of neurological deficit. The most commonly used classification system is that of Denis et al. which classifies these fractures based on the location relative to the sacral foramina, and the incidence of neurological injury.1 Zone I fractures involve the sacral ala lateral to the border of the neural foramina; zone II fractures involve the neural foramina; and zone III fractures involve the central sacral canal medial to the foramina. Indications for surgery for sacral fractures are varied, but usually involve stabilisation of unstable pelvic ring injuries. Surgical decompression without stabilisation is seldom indicated.2 We report on the assessment, management and clinical course of a patient with a minimally displaced zone II sacral fracture and persistent debilitating neurological symptoms.
Consent was obtained from the patient prior to publication of this case report.
Case report
A 16-year-old girl was admitted to the hospital after she fell off her horse and landed on her right side. The horse had fallen and landed on her left side causing a lateral compression injury to the pelvis. A zone II fracture of the left sacrum was diagnosed and she was discharged on crutches. She initially had numbness down the left leg followed by gradually worsening dysaesthetic pain requiring re-admission 3 weeks after the accident. She complained of severe pain, predominantly in the ball of the left foot and the lateral aspect of the foot, as well as marked hypersensitivity of the heel. She complained of numbness around the anus but had full voluntary control of both bladder and bowel. On examination she preferentially lay with the left hip flexed and externally rotated, knee flexed and ankle plantar flexed, most likely in an attempt to reduce tension on the lumbosacral plexus. She had normal power and sensation in the right leg and could straight leg-raise up to about 70 degrees before she had some discomfort on the left. On the left there was marked hypersensitivity of the L5 and S1 dermatomes but normal power. Active dorsiflexion exacerbated the pain in the foot. She required a variety of analgesics and was on strict bed rest with some improvement of the pain.
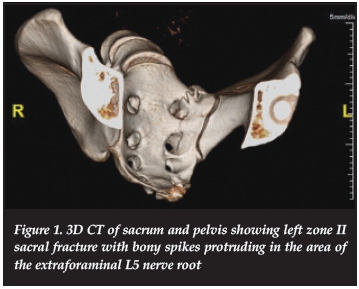
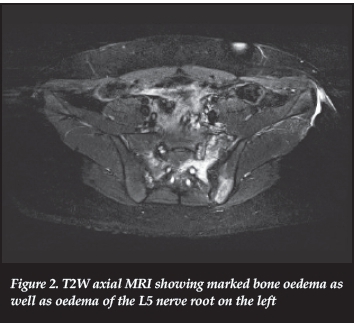
CT (Figure 1) and MRI (Figure 2) confirmed a left-sided sacral fracture with the fracture line running along the ala extending into the foramina of S1, S2 and below. Initially the neurological symptoms were ascribed to plexus irritation from underlying haematoma. After careful scrutiny of the 3D reconstructed CT, a bony fracture spur was identified near the suspected course of the lumbosacral plexus. A spinal epidural catheter for infusion of low dose bupivacaine was placed in an attempt to control the pain while allowing aggressive physiotherapy to mobilise the neural structures in bed, but strictly no weight bearing. Following a week of this therapy, the catheter was removed with instant recurrence of the pain. It was then decided to progress to surgical management.
With the patient supine, a sub-iliacus approach was utilised and an anterior sacral osteotomy with decompression of the lumbosacral plexus was performed. The periosteum of the internal aspect of the pelvis was lifted and the sacro-iliac joint exposed. The medial structures were mobilised and a bony fragment lying perpendicular to the sacral ala was identified and resected with an upcut. The rest of the fracture zone was smoothed off but the foramina were left untouched. Post-operatively there was immediate resolution of the pain with some persistent numbness and weakness of dorsiflexion which resolved, and she was discharged home 3 days following surgery.
She developed new neuropathic pain 2 weeks following surgery, this time predominantly in the L5 distribution. The pain gradually worsened and was associated with functional S1 weakness and a decreased ankle reflex on the left. MRI was repeated demonstrating bone and lumbar plexus oedema, but no residual bony fragments were noted to be causing compression. Conservative management was continued in the form of mobilisation and oral analgesics including pregabalin, amitriptyline, etoricoxib and a sedative as needed. The pain dissipated over a few weeks and by 6 weeks post-surgery, the patient had recovered fully and was discharged ambulant. In time she returned to all her pre-injury activities.
Discussion
Sacral fractures are easily missed and therefore require a high index of suspicion following serious trauma. The presence of a neurological injury greatly increases the rate of diagnosis of sacral fractures, but may often be masked by other distracting injuries.2 The majority of sacral fractures can be diagnosed on plain pelvic inlet and outlet X-rays, but CT-scan remains the modality of choice for diagnosing occult fractures and defining the nature and complexity of the fracture.2-6
Historically, the majority of sacral fractures were managed conservatively, and reports of good outcomes in patients treated non-operatively do exist.2,7 Definitive indications for surgery are relative and include marked displacement, instability, neurological compromise and open fractures. Patients with neurological deficit resulting from compression and contusion of the cauda equina have been shown to do better with surgical decompression, either direct or indirect, than those that were managed conservatively.2-4 Authors also recommend early decompression, less than 24 hours following injury but at most 2 weeks following injury, for improved outcomes in patients with neurological deficit following a sacral fracture.
Here we describe a patient with an apparently benign sacral fracture but persistent neurological deficit and pain. She did not respond to a protracted course of conservative care and was operated almost 5 weeks following injury with eventual full resolution of symptoms. The majority of decompressive surgeries performed for this indication are done via a posterior approach by means of a laminectomy or laminotomy.2 In this case, the offending structure was on the anterior aspect of the sacral ala and therefore an anterior approached was used. No surgical stabilisation of the fracture was required.
We conclude that conservative management should be attempted in undisplaced sacral fractures with minimal neurological deficit, but in the presence of ongoing disability and clinical or radiological evidence of neural impingement, surgical management should be considered.
Compliance with Ethics Guidelines
A Horn, A Thomas and R Dunn declare they have no conflict of interest. Consent was obtained from the patient prior to publication of this case report.
References
1. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67-81. [ Links ]
2. Vacarro AR, Kim DH, Brodke DS et al. Diagnosis and management of sacral spine fractures. J Bone Joint Surg. 2004;84:166-75. [ Links ]
3. Zelle BA, Gruen GS, Hunt T et al. Sacral fractures with neurological injury: is early decompression beneficial? Int Orthop. 2004;28(4):244-51. [ Links ]
4. Aresti N, Murugachandran G, Shetty Rohit et al. Cauda equina syndrome following sacral fractures: a report of three cases. Journ Orthop Surg: 2012;20(2):250-53. [ Links ]
5. Schmidek HH, Smith DA, Kristiansen TK. Sacral Fractures. Neurosurgery. 1984;15(5): 735-46. [ Links ]
6. Phelan ST, Jones DA, Bishay M. Conservative Management of Transverse Fractures of the Sacrum with Neurological Features: a report of four cases. J Bone Joint Surg.1991;73(6):969-71. [ Links ]
 Correspondence:
Correspondence:
Prof RN Dunn
Department of Orthopaedic Surgery
H49 Old Main Building
Groote Schuur Hospital
Anzio Road
7925 Observatory
Cape Town, South Africa
Email: prof@spinesurgery.co.za














