Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.4 Centurion Out./Nov. 2015
Expert opinion on published articles
P Greyling; SJ Mabusha
Reviewer: Dr P Greyling
Department of Orthopaedic Surgery
Steve Biko Academic Hospital
Tel: 012 354 2851
Fracture-dislocations demonstrate poorer postoperative functional outcomes among pronation external rotation IV ankle fractures
Stephen J Warner, MD, PhD, Patrick C Schottel, MD, Richard M Hinds, MD, David L Helfet, MD, and Dean G Lorich, MD
Foot and Ankle International 2015,36(6):641-47
This study compared short-term (12-month) functional outcomes in pronation external rotation (PER) IV ankle fractures with and without a dislocation.
Ankle fractures were categorised using the Lauge-Hansen classification. Preoperative MRI scans were obtained to accurately identify the osseoligamentous injuries and help with the correct classification.
Pronation external rotation IV injuries are uncommon but serious (16-22% of ankle injuries). PER IV injuries are defined as having:
- Deltoid ligament rupture or a medial malleolus fracture
- Anterior inferior tibiofibular ligament (AITFL) rupture
- Anterosuperior to posteroinferior fibula fracture
- Posterior inferior tibiofibular ligament (PITFL) or a posterior malleolus fracture
All fractures were treated by a single surgeon in an injury-specific manner.
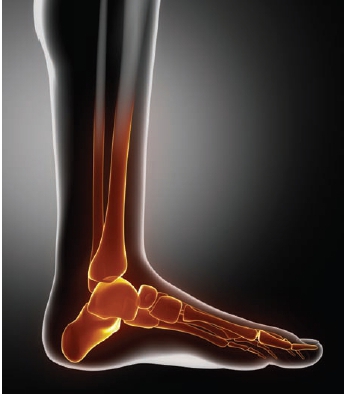
Fixation included:
• Fibula - antiglide plate
• Posterior malleolus - mini-fragment reconstruction plate
• PITFL - 3.5 mm cortical screw with a soft tissue washer
• Medial malleolus - 2.0 mm fragment reconstruction plates
• Deltoid ligament ruptures repaired with suture anchors
• Syndesmotic repair with one or two syndesmotic screws catching four cortices
Bilateral ankle computed tomography scans were obtained prior to discharge to confirm reduction of the syndesmosis. Postoperatively all patients were immobilised in a lower leg splint; at the two-week follow-up they were placed in a controlled ankle motion (CAM) boot and range of motion (ROM) exercises were started. All patients were kept non-weight-bearing for a total of six weeks. Syndesmotic screws were removed no earlier than four months.
The PER TV fracture dislocation group had statistically and clinically poorer outcomes in all five subcategories of the FAOS
Clinical outcome was assessed using the Foot and Ankle Outcome Score (FAOS). Secondary clinical outcomes included ROM, presence of articular and syndesmotic malreduction, complete synostosis, postoperative infection and wound complications.
The PER IV fracture dislocation group had statistically and clinically poorer outcomes in all five subcategories of the FAOS.
A fracture of the posterior malleolus may predispose to instability and risk of articular malreduction, and have inferior outcomes.
This article highlights the severity of a PER IV fracture associated with a dislocation and the importance of reducing the articular surface.
Reviewer: Dr SJ Mabusha
University of KwaZulu-Natal
Department of Orthopaedic Surgery NR Mandela
School of Medicine
Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis
Anthony Rinella, MD, Lawrence Lenke, MD, Camden Whitaker, MD, Yongjun Kim, MD, Soo-sun Park, MD, Michelle Peelle, MD, Charles Edward, MD, and Keith Bridwell, MD Spine 2005;30(4):475-82
The authors retrospectively assessed 33 patients who underwent perioperative halo-gravity traction as an adjunct to modern instrumentation methods in the treatment of severe scoliosis and kyphosis.
Stagnara popularised halo-gravity traction as a safe alternative using the weight of the patient as a counterforce. The traction force can be transferred between the patient's bed, a wheelchair and a walking frame.
Other methods of traction are halo-femoral, halo-tibial and halo-pelvic which provide significant corrective forces but require prolonged periods of bed rest.
The purpose of the study was as follows:
1) To review the safety and efficacy of halo-gravity traction;
2) To review complications associated with traction; and
3) To establish a safe protocol for halo-gravity traction. The placement of the halo device was done in theatre. The pins were tightened to 6- to 8-inch pounds of torque. The duration of perioperative traction is usually two to twelve weeks depending on the patient's overall medical condition.
If an anterior spinal release and fusion is performed, the patient is placed back in traction during the recovery period. Often two to eight more weeks of traction is provided before a definitive posterior instrumentation and fusion with ultimate curve correction. The authors achieved a significant improvement in sagittal and coronal alignment with segmental pedicle screw construct.
The authors should be applauded for this work, which raises a greater sense of awareness for the need for halo-gravity traction before surgical treatment of severe congenital kyphoscoliosis. Rapid correction of severe kyphoscoliosis can increase the risk of neurological compromise, especially if there is a significant kyphotic component. Their work underscores the need for thorough preoperative preparation and evaluation of the patient.
Patients were analysed by age at date of examination, gender, major coronal curve magnitude, major compensatory coronal curve magnitude, major sagittal curve magnitude, traction protocol and procedure type.
Halo-traction-related, early and late complications were noted in each case.

The authors should be applauded for this work, which raises a greater sense of awareness for the need for halo-gravity traction before surgical treatment of severe congenital kyphoscoliosis
Complications were classified into halo-ring related, traction-force related or pathology-patient related.
Complications related to the halo itself include pin loosening, and superficial and deep pin tract infections.
Two forms of cranial nerve involvement have been reported. Cranial nerve 6 palsy (abduscent) was most common, probably due to kinking of the nerve at the petrosphenoidal junction. The palsy presented as a loss of lateral gaze.
The second pattern, a combination of cranial nerves 9, 10 and 12 (glossopharyngeal, vagus and hypoglossal) palsies, presented as dysphagia, loss of palatal and pharyngeal reflexes and weakness of tongue protrusion.
In terms of halo-related symptoms, there were four cases of halo-pin loosening requiring replacement, one infected pin site, one case of pin site, one case of nystagmus and one case of nausea and dizziness. These symptoms resolved immediately with lowering of the amount of traction.
The treatment of severe scoliosis can be very challenging despite the benefits of modern instrumentation methods. Halo-gravity traction is a safe, well-tolerated method of applying gradual, sustained traction to maximise postoperative correction in this difficult population.














