Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.14 n.4 Centurion Oct./Nov. 2015
http://dx.doi.org/10.17159/2309-8309/2015/v14n1a4
PAEDIATRICS
Outcome of displaced supracondylar fractures in children after manipulation and backslab
Dr JL PretoriusI; Dr P RollinsonII; Dr MN RasoolIII
IMBChB(Stell); Registrar, Department of Orthopaedics, University of KwaZulu-Natal
IIMBChB(Sheff), FRCS; Chief Orthopaedic Specialist, Ngwelezane Hospital, Empangeni, KwaZulu-Natal
IIIMBChB(UKZN), FC(Orth)SA, PhD; Paediatric Orthopaedics, Nelson Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
AIM: To assess the functional and cosmetic outcome of displaced supracondylar fractures in children treated by closed reduction and plaster backslab.
METHOD: We retrospectively reviewed 53 patients with Gartland type II and type III fractures that were treated by closed reduction (Blount's technique) and immobilisation in a collar and cuff and above-elbow plaster backslab between December 2011 and May 2012. The mean age was 6.6 years. The mean follow-up time was 12 weeks (range, 6-20). All open injuries and undisplaced fractures were excluded from the study. Flynn's criteria were used to assess functional and cosmetic outcome.
RESULTS: The median loss of motion was 10 degrees and the median change in carrying angle was 4 degrees. Fifty-one patients (96.2%) had satisfactory results, with 87% graded as excellent or good according to the Flynn's criteria for grading of the carrying angle. A range of motion of 100 degrees was achieved in 92.5% of patients at 12 weeks.
CONCLUSION: This method appears to produce less satisfactory results in comparison to closed reduction and fixation with Kirschner wires (K-wires), but it does provide satisfactory results according to Flynn criteria with regard to cosmetic deformity and range of motion at short-term follow-up. It is an acceptable and safe option with which to treat displaced supracondylar fractures.
Key words: supracondylar fractures, closed treatment, outcome
Introduction
Supracondylar fractures of the humerus in children are the commonest elbow injuries. The treatment of these fractures is controversial. The average age at fracture is 6.7 years, and the non-dominant hand is more commonly affected. The mechanism of injury is a fall on an outstretched hand, either from a height or at ground level. Ninety-eight per cent are extension-type injuries. Complications include neurological deficit, vascular injury, compartment syndrome, elbow stiffness, myositis ossificans, non-union, avascular necrosis, angular deformity and rotational deformity.1
Treatment of supracondylar fractures in children is generally determined by using the classification described by Gartland.2 Type I fractures are undisplaced. Type II fractures have partial displacement, but a certain degree of contact is maintained between the proximal and distal fragments. Type III fractures have complete displacement with no bony contact.
Treatment of supracondylar fractures in children is generally determined by using the classification described by Gartland
Various methods of treatment have been described and are based on the degree of displacement They include immobilisation in an above-elbow backslab or even collar and cuff for undisplaced fractures (Gartland I). In displaced fractures (Gartland II and III) cast immobilisation in either flexion or extension,3-9 various forms of traction, including horizontal traction, vertical traction, Dunlop traction,3-6,10-13 skeletal traction through an olecranon pin and traction in pre-fabricated braces have been used.3-6,14-15 The commonly accepted method involves closed reduction and Kirschner-wire (K-wire) fixation, with variation in number of pins and configuration, either medial and lateral wires or only lateral wires, which can be either parallel or crossed.3,616-21
Open reduction is generally reserved for irreducible fractures, vascular compromise and open injuries, but can also be used when attempted reduction is delayed.22,23
The use of Flynn's criteria is a widely accepted method of assessing the results of supracondylar fractures and incorporates a functional element, i.e. range of motion and a cosmetic component with change in carrying angle.24 The Baumann angle after reduction, measured on plain radiograph between the long axis of the humerus and the growth plate of the capitellum, can accurately predict the final carrying angle.25
Over the last 25 years a relatively simple treatment method was used in the orthopaedic department at a regional hospital, which serves as a referral centre for 14 district hospitals as well as serving as a district hospital for a local population of approximately 500 000. Supracondylar fractures are commonly seen in the orthopaedic department each year, approximately 200, and many of these are referred late, often with marked swelling (48 hours).
A treatment protocol was devised which involves placing the fractured arm on vertical skin traction on a drip stand alongside the bed to distract the fracture and reduce swelling
The department is generally staffed by relatively junior medical officers and registrars, and resources are limited. Subsequently a treatment protocol was devised to accommodate these factors. This involves placing the fractured arm on vertical skin traction on a drip stand alongside the bed (Figure 1) to distract the fracture and reduce swelling. A manipulation under anaesthesia is performed at five to six days post injury, flexing the elbow to 110 degrees, securing the reduction with a collar and cuff, and protecting it in an above-elbow backslab.

Patients and method
This is a retrospective review of the functional and cosmetic outcome of all displaced supracondylar fractures in children younger than 13 years of age for a period of 6 months (01 December 2011-31 May 2012) treated by closed reduction, collar and cuff, and protected in an above-elbow backslab.
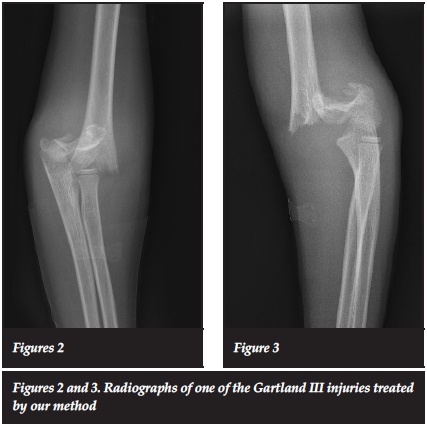
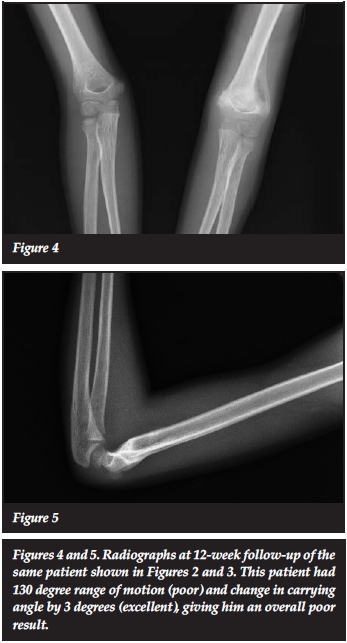
Clinical records and radiographs were reviewed for the demographic details, site and mechanism of injury, clinical and radiographic presentation, mode of treatment before presentation, duration of hospital stay, theatre time and final treatment. Functional outcome was determined by comparing the range of motion and carrying angle with the unaffected arm (Figures 2-5).
Inclusion criteria included: all displaced (Gartland II and III) fractures admitted to the department in the six-month period.
Exclusion criteria: undisplaced supracondylar fractures (Gartland I), fractures that required open reduction and K-wire, open fractures, and patients with poor documentation.
A total of 89 patients with unilateral supracondylar fractures were treated during the study period. Forty-six patients were excluded (undisplaced [30] or needed K-wire fixation [5], or incomplete documentation [11]). There were 53 patients in the study with full documentation and a mean follow-up of 12 weeks. Twenty-nine (54.7%) of the patients were from referral hospitals and the remaining 24 (45.3%) came from the local drainage area. The mean age at time of injury was 6.6 years (13 months to 13 years). Forty-four were male (83%) and nine were female (17%). There were 37 (69.8%) left-sided fractures compared to the right 16 (30.2%). There were no open injuries in the study group.
Neurological examination was documented in all patients; six patients (11.3%) had anterior interosseous nerve palsy and one (1.9%) had a radial nerve palsy. Vascular examination revealed two patients who presented with a pink pulseless hand with normal capillary refill.
These were managed by frequent vascular assessments with the elbow maintained straight on traction and then with reduction and in flexion as per normal with a collar and cuff and backslab when the swelling had diminished, usually after five to six days of straight-arm traction.
Five patients (9.4%) had s and one Salter-Harris II fracture of the distal radius. Fifty-tconcomitant fractures; four distal radius fracturewo patients (98%) sustained extension-type injuries. They were classified into Gartland type II 13 (24.5%) or Gartland type III 40 (75.5%) fractures.
Treatment
All patients received five to six days of vertical traction suspended over a drip stand to allow the swelling to subside and distract the fracture. Thereafter the fracture was reduced in theatre under general anaesthesia under fluoroscopy guidance using Blount's technique, which entails positioning the child at the edge of the operating table with the arm over the image intensifier. Firm traction was applied with a steady continuous force with the elbow in full extension. Once the deformity in the coronal plane was corrected, the surgeon applied countertraction to the proximal fragment while the thumb reached the olecranon and applied an anterior force to the distal fragment to push back the distal fragment to restore the sagittal plane deformity. Concurrently, the other hand flexed the elbow up to 110 degrees.26,27 The reduction was confirmed on Jones view and lateral, a collar and cuff was applied with the elbow maintained strictly at 110 degrees of flexion and then an above-elbow plaster backslab was applied to stabilise the elbow in the flexed position. A neutral position in terms of pronation/supination was used. The radial pulse was assessed after reduction.
The neurovascular status was reviewed again in the ward. Reduction of the fracture was confirmed on plain radiographs, and the child was discharged on the first or second post-operative day.
The collar and cuff and plaster backslab were removed after three weeks and active mobilisation of the elbow encouraged. The patients were then seen at six and twelve weeks after reduction, where the range of motion and carrying angle were measured with a goniometer and documented on a datasheet, and radiographic evaluation was done. If the results were good/excellent (according Flynn's criteria) before 12 weeks, the patients were discharged.
Results
The mean follow-up period was 12.3 weeks (6 weeks to 20 weeks). All neurological deficits resolved by six weeks. The average theatre time was 14.8 minutes (range 3-40) and the average duration of hospital stay was 4.8 days (range 3-8 days). One patient had a failed MUA and had 17 days of vertical traction. The functional and cosmetic outcome was tabulated using Flynn's criteria (Table I).
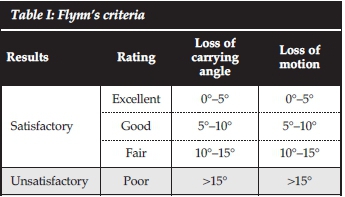
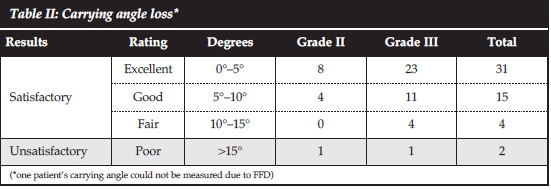
The median loss of carrying angle was 4 degrees. The majority of fractures drifted into varus compared to the unaffected elbow, with only five patients increasing their carrying angle (all within excellent/good range). Fifty-one patients (96.2%) had satisfactory results with 87% graded as excellent or good according to the Flynn criteria for the carrying angle. The two patients who had unsatisfactory results had an 8 and 10 degree varus deformity; they also had unsatisfactory results with regard to range of motion despite the fact that they still had a functional range, i.e. 125 degrees and 135 degrees respectively (Table II).
The median loss of range of motion was 10 degrees. The mean arc of motion was 141 degrees for the Gartland II fractures and 126 degrees for the Gartland III fractures.
In the Gartland II fractures group, 85% of the patients had a satisfactory result with a median loss of motion of 5 degrees, 76% of which were lost at the end range of extension. In the Gartland III fractures group, 55% of the patients had a satisfactory result with a median loss of motion of 10 degrees, again with the majority lost at extreme extension (74%) (Table III).

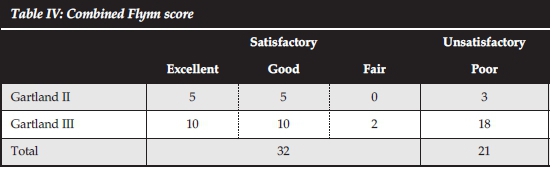
When the carrying angle and loss of motion scores were combined, 60.4% of the patients had a satisfactory result (Table IV).
Discussion
The treatment of supracondylar fractures continues to stimulate interest, especially Gartland III fractures. Various methods have been used to treat supracondylar fractures. Closed reduction and immobilisation in flexion have been used by several surgeons.3-6 Pirone et al. reviewed the results of numerous methods of treatment at a mean of 4.6 years. In the group treated with closed reduction and backslab in flexion, they found 80% satisfactory results.3 The majority of the poor results in this group were due to cubitus varus. De Gheldere et al. used Blount's technique with a cast around the wrist to immobilise the forearm in pronation with the elbow in full flexion.
Our method yielded overall satisfactory results with regard to restoration of the carrying angle
They found that 8% of Gartland III patients had a poor result while all the Gartland II fractures had satisfactory results. They suggested that most Gartland II and III fractures can be treated in this manner but only the postero-lateral Gartland III fractures require K-wires due to their inherent instability in pronation.4
Nejad et al. investigated the effect of supination and pronation on the incidence of cubitus varus deformity after closed reduction and immobilisation in flexion and found no relationship between the position of the forearm and the incidence of deformity but suggested that it is the fracture type and the quality of the reduction that are important.5
Several authors have used various methods of skin traction.6,11-13 Piggot et al.11treated 98 children with displaced supracondylar fractures of the humerus by straight lateral traction. After a mean follow-up period of 3.5 years there were 90 satisfactory and only eight unsatisfactory results; four of these had cubitus varus at final follow-up. Sadiq et al.11treated 20 children with displaced supracondylar fractures with lateral traction in 90 degrees abduction and supination and found no cases of cubitus varus. Urlus et all3 treated 33 patients with reduction in theatre and Dunlop traction for an average of 18 days followed by plaster cast for an average of 16 days; they achieved 97% acceptable results with regard to change in carrying angle.
Immobilisation with plaster cast/moulded gutter-shape slab in extension has also been described.7-' Chen et al.7 compared the incidence of varus in Gartland III fractures treated with either reduction and flexion or reduction and moulded gutter shape plaster slab in extension and 20-30 degrees of valgus. Fifty-seven per cent of his flexion group developed cubitus varus, while none of his extension group developed cubitus varus at 4.6 year follow-up. There was no difference in range of motion in either group. Babar et al' used Chen's technique to treat 70 patients with Gartland III fractures and found 80% acceptable results; this group had a 5 degree change in carrying angle. Gandhi et al.9treated displaced Gartland III fractures with manipulation under anaesthesia and full above-elbow POP in extension and had 69% good/excellent results according to Flynn's criteria.
Traction through an olecranon pin either vertically or in a pre-fabricated brace yielded 84-98% satisfactory results.3,1415
Young et al.6showed 94% satisfactory results using various techniques including plaster casting, overhead skeletal traction and casting and manipulation and K-wires; however, this included undisplaced fractures.
Closed reduction and percutaneous K-wire fixation is considered the gold standard for treatment of displaced supracondylar fractures and results in 99% satisfactory outcome and only a 2% complication rate. Numerous studies on K-wire configuration have been published and even though cross-pin configuration is biomechanically better fixation than lateral only pinning, satisfactory results can be obtained using either technique.316-21
O'Hara et al.19recommended the following conditions to prevent re-operation and malunion: 1) an experienced surgeon should be responsible for the initial management; 2) closed or open reduction of type IIB and type III fractures must be supplemented by stabilisation with K-wires; and 3) K-wires of adequate thickness (1.6 mm) must be used in a crossed configuration.
Neurological injury associated with supracondylar fractures of the humerus in children is a well-known complication. The incidence of traumatic nerve injury varies between 12% and 20%, commonly affecting the anterior interosseous and radial nerve. Iatrogenic nerve injuries associated with this fracture have been reported as being between 2% to 6%, commonly affecting the ulnar nerve; these injuries are a result of blind K-wire placement and ulnar nerve instability in elbow flexion. The majority of these injuries are neuropraxias, and recover between 2-3 months.28-38 The incidence is lowered by using the three lateral pinning technique instead of the cross-pinning or with a minimally open medial approach.20'21-39
A series of patients treated with closed reduction and plaster backslab immobilisation is presented. Our method yielded overall satisfactory results with regard to restoration of the carrying angle. Using the full Flynn criteria, only 60% achieved satisfactory results but this was mainly because of the Flynn's criterion related to range of motion loss. Limitations of the study are that the fractures were assessed only over a 12-week period. Those with a limited range of motion would almost certainly improve and increase their range of motion and consequently their Flynn grading over time. Previous studies looking at return of range of motion found that only 86-92% of range of motion returns by 12 weeks which improves to 98% of uninjured range by 52 weeks.40,41 Baumann's angle, measured on the injured and compared with the uninjured arm would have been a more objective measurement of change in carrying angle, but due to the fact that the AP radiographs of both elbows were taken on the same film, the angle between actual beam and elbow was 30 degrees. This gave distorted views of the Baumann's angle and could thus not be included.25
The Flynn criteria are very 'severe' in that a carrying angle loss of 10 degrees or more is not regarded as a good result. A neutral carrying angle of a few degrees of varus (up to 5°) is generally accepted by patients/parents and is usually not even noticed. Mild varus deformity of the elbow seems to cause more anxiety to orthopaedic surgeons than to patients and parents and may not be as important as implied by Flynn's criteria.
The technique has been refined over 20 years at our institution with almost 100 cases per year managed. Corrective osteotomy for malunion/varus in the cases managed by this method was not indicated or demanded by the parents.
Conclusion
Closed reduction, collar and cuff and plaster backslab immobilisation under general anaesthesia in theatre is an acceptable technique to treat supracondylar fractures in children. It saves theatre time while obtaining anatomical reduction and results in a satisfactory outcome according to Flynn criteria for cosmetic appearance and a functional range of motion for the majority of patients in the short term. It also avoids the possible complications of K-wire fixation including iatrogenic ulnar nerve injury and pin-tract sepsis which could be catastrophic if the patient is lost to follow-up in the rural setting.
This method appears to produce slightly inferior results in comparison with closed reduction and fixation with K-wires, but it provides excellent results with regard to alignment and a range of motion that is comparable with return of motion found in other studies. It is thus a good and safe option to treat displaced supracondylar fractures.
References
1. Beaty JH KJ. Supracondylar fractures of the distal humerus. Rockwood and Wilkins' fractures in children. 5th ed.; 2005. p. 577-615. [ Links ]
2. Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 1959 Aug;109(2):145-54. [ Links ]
3. Pirone AM, Graham HK, Krajbich JI. Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am 1988 Jun;70(5):641-50. [ Links ]
4. de Gheldere A, Bellan D. Outcome of Gartland type II and type III supracondylar fractures treated by Blount's technique. Indian J Orthop 2010 Jan;44(1):89-94. [ Links ]
5. Marashi Nejad SA, Mehdi Nasab SA, Baianfar M. Effect of supination versus pronation in the non-operative treatment of pediatric supracondylar humerus fractures. Arch Trauma Res 2013 Spring;2(1):26-29. [ Links ]
6. Young S, Fevang JM, Gullaksen G, Nilsen PT, Engesaeter LB. Deformity and functional outcome after treatment for supracondylar humerus fractures in children: a 5- to 10- year follow-up of 139 supracondylar humerus fractures treated by plaster cast, skeletal traction or crossed wire fixation. J Child Orthop 2010 Oct;4(5):445-53. [ Links ]
7. Chen RS, Liu CB, Lin XS, Feng XM, Zhu JM, Ye FQ. Supracondylar extension fracture of the humerus in children. Manipulative reduction, immobilisation and fixation using a U-shaped plaster slab with the elbow in full extension. J Bone Joint Surg Br 2001 Aug;83(6):883-87. [ Links ]
8. Babar IU, Shinwari N, Bangash MR, Khan MS. Management of supracondylar fracture of humerus in children by close reduction and immobilization of the elbow in extension and supination. J Ayub Med Coll Abbottabad 2009 Oct-Dec;21(4):159-61. [ Links ]
9. Gandhi J, Horne G. Type III supracondylar fractures of the humerus in children - straught-arm treatment. Acta Ortop Bras 2010(18(3)):132-34. [ Links ]
10. Gadgil A, Hayhurst C, Maffulli N, Dwyer JS. Elevated, straight-arm traction for supracondylar fractures of the humerus in children. J Bone Joint Surg Br 2005 Jan;87(1):82-87. [ Links ]
11. Piggot J, Graham HK, McCoy GF. Supracondylar fractures of the humerus in children. Treatment by straight lateral traction. J Bone Joint Surg Br 1986 Aug;68(4):577-83. [ Links ]
12. Sadiq Z, Syed T, Travlos J. Management of grade III supra-condylar fracture of the humerus by straight-arm lateral traction. MInternational Orthopaedics (SICOT) 2007(31):155-58. [ Links ]
13. Urlus M, Kestelijn P, Vanlommel E, Demuynck M, Vanden Berghe L. Conservative treatment of displaced supra-condylar humerus fractures of the extension type in children. Acta Orthop Belg 1991;57(4):382-89. [ Links ]
14. Matsuzaki K, Nakatani N, Harada M, Tamaki T. Treatment of supracondylar fracture of the humerus in children by skeletal traction in a brace. J Bone Joint Surg Br 2004 Mar;86(2):232-38. [ Links ]
15. Badhe NP, Howard PW. Olecranon screw traction for displaced supracondylar fractures of the humerus in children. Injury 1998 Jul;29(6):457-60. [ Links ]
16. Skaggs DL, Sankar WN, Albrektson J, Vaishnav S, Choi PD, Kay RM. How safe is the operative treatment of Gartland type 2 supracondylar humerus fractures in children? J Pediatr Orthop 2008 Mar;28(2):139-41. [ Links ]
17. Woratanarat P, Angsanuntsukh C, Rattanasiri S, Attia J, Woratanarat T, Thakkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma 2012 Jan;26(1):48-53. [ Links ]
18. Maity A, Saha D, Roy DS. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res 2012 Feb 15;7:6-799X- 7-6. [ Links ]
19. O'Hara LJ, Barlow JW, Clarke NM. Displaced supra- condylar fractures of the humerus in children. Audit changes practice. J Bone Joint Surg Br 2000 Mar;82(2):204-10. [ Links ]
20. Barlas K, Baga T. Medial approach for fixation of displaced supracondylar fractures of the humerus in children. Acta Orthop Belg 2005 Apr;71(2):149-53. [ Links ]
21. Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am 2001 May;83-A(5):735-40. [ Links ]
22. Otsuka NY, Kasser JR. Supracondylar Fractures of the Humerus in Children. J Am Acad Orthop Surg 1997 Jan;5(1):19-26. [ Links ]
23. Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br 2006 Apr;88(4):528-30. [ Links ]
24. Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years' experience with long-term follow- up. J Bone Joint Surg Am 1974 Mar;56(2):263-72. [ Links ]
25. Worlock P. Supracondylar fractures of the humerus. Assessment of cubitus varus by the Baumann angle. J Bone Joint Surg Br 1986 Nov;68(5):755-57. [ Links ]
26. Blount WP. Supracondylar(diacondylar, transcondylar) fractures. In: Wilkins W, editor. Fractures in children. 1st ed.; 1955. p. 26-42. [ Links ]
27. Kinkpe CV, Dansokho AV, Niane MM, Chau E, Sales de Gauzy J, Clement JL, et al. Children distal humerus supra-condylar fractures: the Blount Method experience. Orthop Traumatol Surg Res 2010 May;96(3):276-82. [ Links ]
28. Culp RW, Osterman AL, Davidson RS, Skirven T, Bora FW,Jr. Neural injuries associated with supracondylar fractures of the humerus in children. J Bone Joint Surg Am 1990 Sep;72(8):1211-15. [ Links ]
29. Dormans JP, Squillante R, Sharf H. Acute neurovascular complications with supracondylar humerus fractures in children. J Hand Surg Am 1995 Jan;20(1):1-4. [ Links ]
30. Cramer KE, Green NE, Devito DP. Incidence of anterior interosseous nerve palsy in supracondylar humerus fractures in children. J Pediatr Orthop 1993 Jul- Aug;13(4):502-505. [ Links ]
31. Campbell CC, Waters PM, Emans JB, Kasser JR, Millis MB. Neurovascular injury and displacement in type III supra-condylar humerus fractures. J Pediatr Orthop 1995 Jan- Feb;15(1):47-52. [ Links ]
32. Brown IC, Zinar DM. Traumatic and iatrogenic neurological complications after supracondylar humerus fractures in children. J Pediatr Orthop 1995 Jul- Aug;15(4):440-43. [ Links ]
33. Cheng JC, Lam TP, Shen WY. Closed reduction and percutaneous pinning for type III displaced supracondylar fractures of the humerus in children. J Orthop Trauma 1995;9(6):511-15. [ Links ]
34. Ikram MA. Ulnar nerve palsy: a complication following percutaneous fixation of supracondylar fractures of the humerus in children. Injury 1996 Jun;27(5):303-305. [ Links ]
35. Royce RO, Dutkowsky JP, Kasser JR, Rand FR. Neurologic complications after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop 1991 Mar- Apr;11(2):191-94. [ Links ]
36. Rasool MN. Ulnar nerve injury after K-wire fixation of supracondylar humerus fractures in children. J Pediatr Orthop 1998 Sep-Oct;18(5):686-90. [ Links ]
37. Birch R, Achan P. Peripheral nerve repairs and their results in children. Hand Clin 2000 Nov;16(4):579-95. [ Links ]
38. Zaltz I, Waters PM, Kasser JR. Ulnar nerve instability in children. J Pediatr Orthop 1996 Sep-Oct;16(5):567-69. [ Links ]
39. Green DW, Widmann RF, Frank JS, Gardner MJ. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J Orthop Trauma 2005 Mar;19(3):158-63. [ Links ]
40. Zionts LE, Woodson CJ, Manjra N, Zalavras C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Orthop Relat Res 2009 Aug;467(8):2007-10. [ Links ]
41. Spencer HT, Wong M, Fong YJ, Penman A, Silva M. Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. J Bone Joint Surg Am 2010 Apr;92(4):904-10. [ Links ]
 Correspondence:
Correspondence:
Dr JL Pretorius
Department of Orthopaedic Surgery University of KwaZulu-Natal
Email: johan.doc@gmail.com
The content of this article is the original work of the authors. No benefits of any form have been or are to be received from a commercial party related directly or indirectly to the subject of this article. Ethical approval was obtained.














