Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.14 n.3 Centurion Aug./Sep. 2015
http://dx.doi.org/10.17159/2309-8309/2015/V14N3A10
SPINE
Stand-alone cage neck fusions: A long-term review
MM MaineI; I ZondaghII
IMBChB(Medunsa); Orthopaedic registrar, Department of Orthopaedics, University of Pretoria
IIMBChB(Pret), FCS Orth(SA), MMed(Orth); Spinal consultant, Department of Orthopaedics, 1 Military Hospital, University of Pretoria
ABSTRACT
BACKGROUND: Anterior cervical decompression and fusion (ACDF) is a well-known treatment for persistent cervical radiculopathy or myelopathy. Fusion is performed to stabilise the segment, maintain foraminal height, and maintain the normal sagittal profile. The stand-alone cage concept, initiated by Bagby, has been used in the human spine since 1988. There are some concerns with stand-alone cages regarding expulsion and migration of the cage.
AIM: To review the long-term outcome of stand-alone cage fusions done from 2000-2010 at 1 Military Hospital and describe our experience with this procedure.
METHODS: A retrospective review of stand-alone cage neck fusion of 55 levels in 35 patients performed between January 2000 and December 2010 at 1 Military Hospital was done. Clinical notes and X-rays were reviewed. Fusion rate was assessed using standard X-rays with flexion/extension views.
RESULTS: Seven patients (14%) had a non-union, giving a fusion rate of 86%. Five non-unions were painful. One patient had a revision for a painful non-union (NDI score: 35/50). One patient refused to have a revision at last visit despite having significant pain (NDI score: 27/50). One patient with a double level non-union has phaeochromocytoma with significant risk to revision and chose not to have the surgery (NDI score: 14/50). Two patients are on the waiting list for a revision in the near future (NDI scores: 24/50 and 19/50). The two remaining patients with non-unions are asymptomatic (NDI scores: 0/50 and 7/50.
CONCLUSION: Stand-alone cage fusion is a safe and effective procedure providing a favourable clinical and radiological outcome. Good fusion rates can be obtained (86% in our study) with this method.
Key words: radiculopathy, myelopathy, anterior cervical discectomy and fusion, stand-alone cage fusion, fusion rate
Introduction
Anterior cervical decompression and fusion (ACDF) is a well-known treatment in the management of cervical degenerative disease causing persistent radiculopathy or myelopathy. Anterior surgery of the cervical disc with fusion using iliac crest autograft was introduced in the 1950s.1
After decompression, a fusion is performed to stabilise the segment, restore the height and recreate the normal cervical lordosis. Initially ACDF was performed using tricortical iliac bone graft with good fusion rates.
The use of autologous bone graft gave rise to complications, especially acute and chronic pain at the donor site. Donor site morbidity favoured development of cage technology.
Anterior cervical plating was added to un-instrumented autograft fusion to prevent graft settling and collapse and to enhance a solid fusion. Plating however has its own challenges.
PEEK (polyether ether ketone) cervical synthetic cages have recently been used. PEEK has biomechanical properties similar to bone and is radiolucent allowing for post-operative radiographic fusion evaluation. The standalone cage concept was initiated by Bagby and has been used in the human spine since 1988. The rectangular cages used resemble the dimensions and anatomy of the disc space and vertebral end plates. There are concerns with stand-alone cage usage regarding expulsion and migration of the cage.
The purpose of the study is to review the long-term outcome of stand-alone cage fusions done from 2000 to 2010 at 1 Military Hospital and to describe our experience with the procedure.
The impact of the study is aimed to show that standalone cage fusion is a safe and effective procedure which provides a good clinical and radiological outcome.
Methods
A retrospective review was done on patients who underwent anterior cervical decompression and fusion using stand-alone cage at 1 Military Hospital between January 2000 and December 2010.
Patients were operated by a spinal team consisting of an orthopaedic surgeon and a neurosurgeon working together.
A standard right-sided Smith Robinson approach was used. After discectomy and decompression the end plates were prepared and the cage, packed with either autogenous bone, allograft bone or synthetic bone substitutes, was inserted. The cage size was determined by releasing distractor pins and assessing resistance to pull-out.
Post-operative immobilisation in a Philadelphia brace for 12 weeks was the standard of care.
Fusion rates were assessed using standard X-rays with flexion/extension views as shown in Figure 1. Trabecular continuity and bone bridging across the disc space, absence of motion with flexion/extension views and absence of a dark halo around the implant on AP and lateral views were assessed.

Patient clinical outcome was assessed using the Neck Disability Index score (NDI). The NDI was developed in 1989 by Vernon.2 Each of the ten items is scored from 0-5. The maximum score is therefore 50 (see Appendix A). The obtained score can be multiplied by 2 to produce a percentage score. The scoring intervals for interpretation are as follows:

Results
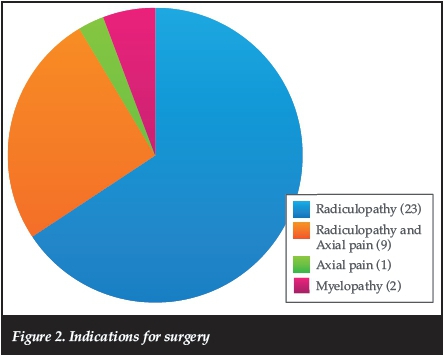
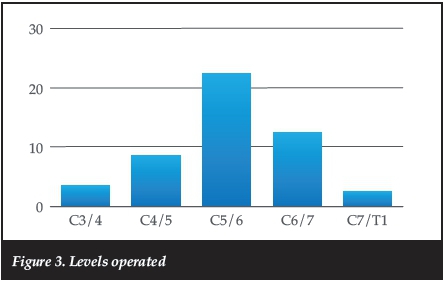
Thirty-five patients were treated with stand-alone anterior cervical cages between January 2000 and December 2010 at 1 Military Hospital. Seventeen patients were male and 18 were female, with an average age of 58 years. Indications for surgery are shown in Figure 2. Follow-up was from 2 to 12 years with an average of 5 years. Most patients (22) underwent C5/C6 fusion, followed by C6/7 (11) as shown in Figure 3.
Eighteen patients had a 1-level fusion, 14 patients had a 2-level fusion and three patients had 3-level fusion (18 single level and 17 multilevel). Thus a total of 55 levels were fused. The average theatre time was 195 minutes.
The most frequently used cage height was 6 mm as depicted in Figure 4.

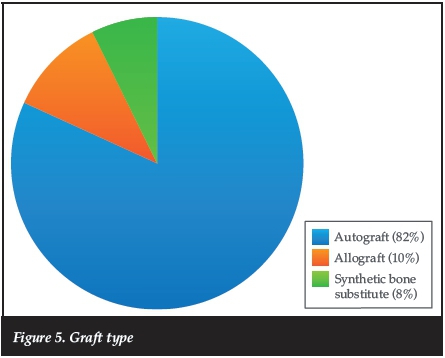
The graft material used was autograft in 82%, allograft in 10% and synthetic bone substitute in 8% as illustrated in Figure 5.
Seven patients (14%) had a non-union, giving a fusion rate of 86%. Of the seven non-unions, there were no nonunion in the three level fusions. In the two-level fusion group there was one patient who had non-union at both operated levels. The remaining six non-union patients were all single-level surgery. Five non-unions were painful. One patient had a revision for a painful non-union (NDI score: 35/50), one patient refused to have a revision at last visit despite having significant pain (NDI score: 27/50), one patient with a double-level non-union has phaeochromocytoma with significant risk to revision and chose not to have the surgery (NDI score: 14/50). Two patients are on the waiting list for a revision in the near future (NDI scores: 24/50 and 19/50). The two remaining patients are asymptomatic (NDI scores: 0/50 and 7/50).
Results of our study are comparable to other recent publications for stand-alone cage fusions
From the seven non-unions reported, with regard to bone graft material used, six out of seven non-unions were from autograft, and for the one, non-union synthetic graft was used.
In this study some complications were noted. One patient had a recurrent laryngeal nerve injury after a two-level fusion (C5-C7) and had a persistent speech problem at 9 years' follow-up. Another patient had an internal jugular vein injury which was ligated intra-operatively to control bleeding, theatre time was 390 minutes, and the patient was started on long-term anticoagulants. Another patient had a fracture of end plate at C7 which needed additional plate and screw fixation. Two cages were mal-positioned, one anterior and one lateral, but they did not cause any clinical problems. There were no infections, cerebrospinal fluid leaks or cage migrations in our study.
Fifteen of 35 patients (42%) demonstrated radiological evidence of adjacent segment disease at 5-years' follow-up; however, only one patient required revision for adjacent segment disease (ASD).
Discussion
Degenerative disease of the cervical spine can result in significant radiculopathy, myelopathy or both. The anterior approach is the preferred method for decompression of the roots because of the easy patient positioning and surgical approach by blunt dissection through anatomical planes. With an anterior approach, however, interbody fusion is often required to maintain foraminal height and prevent localised kyphosis, especially with multiple-level surgery.
Results of our study are comparable to other recent publications for stand-alone cage fusions. Marota et al? in their study of 132 patients showed an 87% fusion rate at 5-years' follow-up. Dunn et al.1had a 92% fusion rate in 34 patients at 2-years' follow-up. Fraser et al? did a meta-analysis of fusion rates comparing different anterior fusion methods.
They found fusion rate to be 84.99% using anterior cervical decompression, 92.1% using anterior cervical decompression and fusion, and 97.1% using anterior cervical decompression and fusion with anterior plating. Plating is however more costly, requires longer operative times, and may be associated with problems such as breakage or dislocation of the screws and perforation of adjacent structures.
The use of interbody cages for anterior cervical fusion was introduced to prevent problems such as graft resorption and expulsion and therefore loss of alignment as seen with tricortical iliac bone graft.6
Cho et al.7used cages to replace plate function in multilevel cervical fusion. They demonstrated that the PEEK cage results are statistically better than those of the plating group in total complications, p< 0.05. They also showed that PEEK cage without plating and autogenous iliac crest graft with plating are good methods for interbody fusion in multilevel cervical degenerative diseases.
We feel stand-alone cage fusion is a safe and effective procedure providing a good clinical and radiological outcome
Shousha et al.8showed that stand-alone cage fusion is an acceptable line of treatment for four-level cervical disc disease, both clinically and radiologically, though the addition of posterior instrumentation yielded better radiological results; the difference, however, did not reach the statistical significance level.
Clinical follow-up was attempted but the clinical information/NDI scores were only obtained in 20 patients. There was a trend in our patients with a radiological nonunion to have a higher NDI score than those with radiological union.
Our ASD incidence is high compared to other literature (±25%), but our revision rate for ASD remains low despite the radiological picture. This brings us to question the clinical relevance of ASD.
McCormick et al.9studied adjacent segment disease and demonstrated that adjacent segment disease is not clinically relevant. They also support the idea that ASD is the consequence of natural degeneration of the discs.
Conclusion
Almost 50% of our study group underwent multilevel fusion with one reported non-union. We feel stand-alone cage fusion is a safe and effective procedure providing a good clinical and radiological outcome for the management of cervical degenerative disease, even in multilevel disease.
Good fusion rates can be obtained (86%) using this method.
The high incidence of adjacent segment disease seems not to be clinically relevant at long-term follow-up.
This study is the authentic work of the authors. No financial benefits were received from any commercial party for this study.
References
1. Cloward RB. The anterior approach for removal of ruptured cervical discs. J Neurosurg 1958;15:602-17. [ Links ]
2. Vernon H, Moirs S. The neck disability index: a study of reliability and validity. J Manip Physiol Ther 1991;14(7):409-15. [ Links ]
3. Marota N, Landi A, Tarantino R, Mancarella C, Ruggeri A, Delfini R. Five-year outcome of stand-alone fusion using carbon cages in cervical disc arthrodesis. Eur Spine J 2011;20(Suppl 1):S8-S12. [ Links ]
4. Dunn RN, Pretorius C. Cervical PEEK cage standalone fusions - the issue of subsidence. SA Orthopaedic Journal 2011;10(1):25-29. [ Links ]
5. Fraser JF, Hârti R. Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. Neurosurg Spine 2007;6:298-303. [ Links ]
6. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty patients. J Bone Joint Surg Am)1993;75:1298-1307. [ Links ]
7. Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol 2004;62:378-86. [ Links ]
8. Shousha M, Ezzati A, Boehm H. Four-level anterior cervical discectomies and cage-augmented fusion with and without fixation. Eur Spine J 2012;21:2512-19. [ Links ]
9. McCormick PC. The adjacent segment. J Neurosurg Spine 2007;6:1-4. [ Links ]
 Correspondence:
Correspondence:
Dr MM Maine
Department of Orthopaedics
University of Pretoria
1 Military Hospital
Private Bag x1026
0143 Thaba Tshwane
Tel: (012) 314 0044;Fax: 086 632 9182
Email: motsapim@yahoo.com
Appendix















