Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.3 Centurion Ago./Set. 2015
http://dx.doi.org/10.17159/2309-8309/2015/V14N3A9
TRAUMA
Early application of the Thomas splint for femur shaft fractures in a Level 1 Trauma Unit
S MaqungoI; J AllenII; H CarraraIII; S RocheIV; N RueffV
IDr. FC(Ortho); Department of Orthopaedic Surgery, University of Cape Town, Groote Schuur Hospital, South Africa
IIMr; Medical student (posthumous), University of Witwatersrand, South Africa
IIIMr. MPH; Analytical Epidemiologist, School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IVDr. FCS(Ortho); Department of Orthopaedic Surgery, University of Cape Town, Groote Schuur Hospital, South Africa
VDr. FMH Orthopaedics, Swiss orthopaedics; Department of Orthopaedic Surgery, University of Cape Town, Groote Schuur Hospital, South Africa
ABSTRACT
AIMS: To measure the compliance of our prehospital service and trauma unit with international guidelines relating to the early application of the Thomas splint in patients with a femur shaft fracture on clinical examination.
MATERIALS AND METHODS: Level IV retrospective review of clinical and radiological records of patients presenting from 01 January 2012 to 31 December 2012 at a Level 1 Trauma Unit.
We included all patients with femur shaft fractures independently of their mechanism of injury. Exclusion criteria were: ipsilateral fracture of the lower limb, neck and supracondylar femur fractures, pathological, periprosthetic and incomplete fractures. The database available for review included demographic information, mechanism of injury, side injured and time when a radiological study (Lodox® and/or X-ray) was performed.
RESULTS: We identified 160 fractures. Sixty of these (37.5%) were correctly immobilised with a Thomas splint prior to the first radiological examination being either a Lodox® or an X-ray. Seventeen fractures (45.9%) out of the 37 fractures not splinted or not correctly splinted at the time of the first radiological exam were then correctly splinted before the second radiological exam.
CONCLUSION: Only 37.5% of patients presenting to our trauma unit with a femur shaft fracture have a Thomas splint applied before radiological examinations are performed. This deficiency needs to be addressed at all levels of healthcare, i.e. prehospital, peripheral and tertiary hospitals.
Key words: femur, fracture, splint, application, trauma
Introduction
The traction splint for a femur shaft fracture is an orthopaedic device made of a metallic frame that extends from the proximal thigh to an area distal to the heel (Figure 1). The proximal padded portion fits against the ischial tuberosity and the distal part serves as a traction site in order to mimic normal bone stability and limb length. To improve the efficacy of the Thomas splint, the thigh and leg should be supported by several soft supports or one long support, usually a Kramer wire.

Hugh Owen Thomas (1834-1891) first described in 1875 a model of traction splint for treating diseases of the knee.1-3 Only later in 1875 was it used for conservative treatment of isolated femur fractures. Its wider use was implemented in the British army by Sir Robert Jones during the First World War at Level Three facilities.2
Regular Army Medical Officer Meurice Sinclair (1878-1966) revolutionised the management and treatment of gunshot fractures with his system of traction added to the Thomas splint.3 Secondary to the use of the Thomas splint on the battlefields, soldiers with ballistic femur fractures saw their morbidity and mortality decrease significantly from 80% to less than 8%.2,3
Traction splints should only be applied when the fracture is isolated to the femur. Use of a traction splint in the presence of other ipsilateral fractures in the leg will cause the weaker fracture site to pull apart and not the targeted femur fracture.4,5
During the Gulf conflict (1990-1991) Rowlands stated that the reduction and stabilisation of the fracture reduced further soft tissue lesions and facilitated transport/evacuation of the patient.6 According to other authors, patients in the setting of prehospital care or awaiting definitive management should be immobilised in a traction splint.2,7-9
The Thomas splint is a cost-effective device, reusable, non-invasive, easy to apply, and should be applied with a soft posterior cushion or Kramer wires along with a skin traction. The force applied when the skin traction is tightened to the Thomas splint should be around 3 kg to avoid soft tissues lesions. The force applied is not sufficient to reduce the fracture but enough to maintain an alignment and decrease the complications associated with femur shaft fracture.
The benefits largely outweigh the known complications associated with the application of a Thomas splint which include peroneal nerve palsy, pressure sores, compartment syndrome and soft tissues injuries.5
The aim of our study is to measure the compliance of our prehospital service and trauma unit with international guidelines relating to the early application of the Thomas splint in patients with a femur shaft fracture on clinical examination in order to improve its adoption and improve patients' standard of care especially in the setting of delayed access to theatre.
Materials and methods
This retrospective study has been approved by the Ethics Committee of our Institution (HREC REF 499/2014).
We reviewed the clinical and radiological records of patients admitted in the Trauma Unit between 01 January 2012 and 31 December 2012. Radiological records were screened for any Lodox® (Lodox Systems (Pty) Ltd, Sandton, Johannesburg, South Africa), and X-rays in which a femur shaft fracture was present. The Lodox® Statscan is a low-dose full-body digital X-ray imaging device capable of screening a patient in 13 seconds while emitting ten times less harmful dose (0.12 mGy) than regular X-ray systems.10
Only type AO/OTA 32 fractures were included.11 Intertrochanteric, neck of femur and distal metaphyseal fractures were excluded. One undisplaced distal femur fracture due to a gunshot injury and one periprosthetic (THR) Vancouver C fracture were also excluded as one could not suspect a fracture in the first case and as the second case could have been mistaken for a hip prosthesis dislocation. Twenty-one femur shaft fractures were excluded in 21 patients with an ipsilateral fracture of the lower limb (15 tibia, three medial malleoli, two ankle and one calcaneus fractures).
In total, 160 femur fractures were identified in 157 patients (three patients had bilateral femur fractures). The database was reviewed for date and time of admission, age, gender, mechanism of injury, side injured and time when a Lodox® and/or an X-ray were performed. When a Lodox® was available, it qualified as a first radiological exam. When no Lodox® was available, we took the first X-ray as the first radiological exam. The second radiological exam was an X-ray when a Lodox® had been performed before it or if it was a repeated X-ray when no Lodox® was available.
Statistical analysis was performed using STATA version 13.1 (StataCorp LP, 4905 Lakeway Station), with the statistical significance set at P<0.05.
The distribution of continuous variables was assessed for normality graphically and using the Shapiro Wilk test. When skewness was observed medians and interquartile ranges were reported and the Mann-Whitney test applied to compare the data between two groups. Categorical data were analysed using the chi-square test or the Fisher's exact test as appropriate.
Patients in the setting of prehospital care or awaiting definitive management should be immobilised in a traction splint
Furthermore the relationship between the binary variable (no splint/splint) and a number of explanatory variables was assessed by estimating prevalence ratios and their 95% CIs estimated using a general linear model.
The median age of the patients (N = 157) was 32 years, the range was 13.6-92.2 years and the interquartile range was 24-43 years.
Results
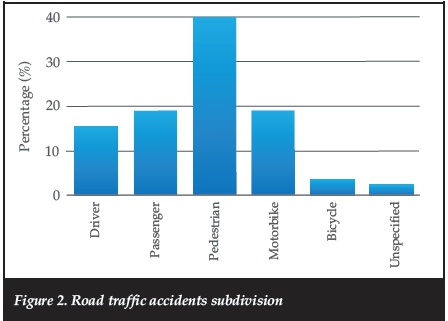
Of the 160 patients identified, 110 (70.1%) were males and 47 (29.9%) were females, with three females having bilateral femur shaft fractures. The causes of injury were: road traffic accident (RTA) (n = 84); gunshot wound (gSW) (n = 40); fall (low and high energy) (n = 23); and ten others (Figure 2). Every day was split between the day shift (07h00-19h00), the early night shift (19h01-23h59) and the late night shift (00h00-06h59) (Table I).
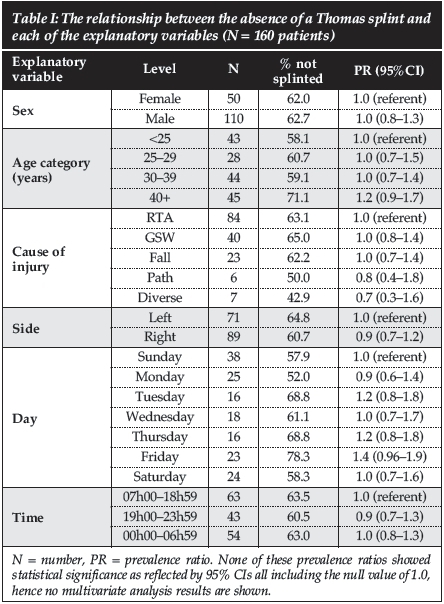
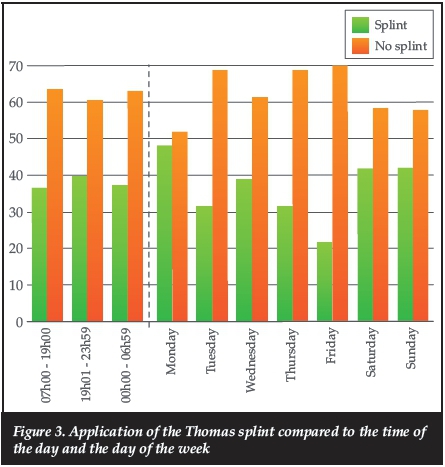
The application of the Thomas splint was compared to gender, side and cause of injury, and also to the time of the day and the day of the week (Figure 3). All those variables were not statistically significant using either the chi-square test or Fisher's exact test as appropriate.
The relationship between not being splinted and each of the explanatory variables is shown in Table I and it shows no statistical significance.
Proportions splint/no splint according to these variables above were not statistically significant using either the chi-square test or Fisher's exact test as appropriate.
Of the 160 fractures, 60 fractures were immobilised with a Thomas splint prior to the first radiological exam (Lodox® or X-ray), corresponding to a 37.5% compliance rate. A 41.1% compliance rate was noted when the first radiological exam was an X-ray and 33.1% when the first radiological exam was a Lodox®.
In 37 patients, the presence of a femur shaft fracture was diagnosed on the Lodox® but the patient was not properly immobilised (backslab [n = 1] or Kramer wires [n = 6]) or not immobilised at all (n = 30). 45.9% were then correctly immobilised with a Thomas splint prior to the X-ray (X-ray as second radiological exam).
None of these associations were shown to be statistically significant.
Discussion
During the initial assessment, femur shaft fractures can be easily diagnosed with an obvious deformity and tenderness of the affected limb.12
In the Trauma Unit where Thomas splints are readily available, the internal guideline of the Trauma Department is to systematically apply them in the setting of a femur shaft fracture (Figure 4), in order to align the fracture, provide immobilisation, control muscle spasm, reduce pain, reduce the incidence of fat embolism, decrease blood loss and prevent further damage to blood vessels, neurovascular structures and soft tissue. 2,3,5,6,8,12,13

Our study demonstrates that when a patient sustained a femur shaft fracture, they have a 37.5% chance of having a Thomas splint applied before the first radiological exam regardless of the patient, the cause of injury and the day and time at which the patient is admitted to the Trauma Unit.
One hundred and seven fractures were diagnosed on an X-ray only and the application rate of the Thomas splint was 40.2%.
When a femur fracture is seen on the Lodox®, appropriate action is taken and a Thomas splint is applied before the patient is sent for further X-rays in 47.5% of the patients.
Our initial application rate of 37.5% is less than ideal. This figure is made lower by the fact that we have access to a Lodox Statscan whole body scanner which most institutions do not. This is meant to scan for life-threatening injuries before secondary survey is completed. Screening for femur fractures and applying Thomas splints is part of the secondary survey which we do after the Lodox® has been done. The Lodox® scans the whole body in 13 seconds and therefore does not unnecessarily delay secondary survey.
Femur shaft fractures can be easily diagnosed with an obvious deformity and tenderness of the affected limb
Ambulances and paramedics are also meant to have femur splints available for application in the prehospital setting. This is important in a country like ours where distances between accident scenes and hospitals can be vast. Our low rate of Thomas splint application also speaks to this deficiency in our pre-hospital patient care. Also, often enough patients are not taken to the definitive care hospital initially; they are taken to the nearest hospital. These local hospitals are not usually equipped with Thomas splints to apply while patients are awaiting transfer and are therefore not immobilised or are immobilised inappropriately, for example in backslabs.
If we look at splintage rates after Lodox then a further 46% of patients are splinted before formal X-rays are obtained. Then there are those who were immobilised in backslabs or Kramer wires. The combined splintage figure of 77% is more respectable and more in keeping with acceptable clinical guidelines.
The following limitations of our study must be reported: retrospective study design and its limitations; pain score, outcome scores and complications related to the use of the Thomas splint were not recorded.
Conclusion
Cause of injury, time of the day and day of the week did not have any statistical significance for the early application of a Thomas splint in our Trauma Unit. Ambulances and peripheral hospitals should be supplied with Thomas splints to ensure early application as there are often delays experienced before patients can be transferred to secondary or tertiary hospitals for definitive care.
The authors have no financial disclosures and/or conflicts of interest to declare with respect to the content of this article. Mr H Carrara was responsible for the statistical components.
References
1. Kirkup J. Thomas splint. J Med Biogr. 2008 May;16(2):104. [ Links ]
2. Robinson PM, O'Meara MJ. The Thomas splint: its origins and use in trauma. J Bone Joint Surg Br. 2009 Apr;91(4):540-44. [ Links ]
3. Austin RT. Meurice Sinclair CMG: a great benefactor of the wounded of the First World War. Injury. 2009 May;40(5):567-70. [ Links ]
4. Abarbanell N. Prehospital midthigh trauma and traction splint use: recommendations for protocols. American Journal of Emergency Medicine. 2001 Mar;19(2). [ Links ]
5. Bledsoe B, Barnes D. Traction splint. An EMS relic? JEMS. August 2004;29(8):64-67. [ Links ]
6. Rowlands TK, Clasper J. The Thomas splint: a necessary tool in the management of battlefield injuries. J R Army Med Corps. 2003 Dec;149(4):291-93. [ Links ]
7. Henry BJ, Vrahas MS. The Thomas splint. Questionable boast of an indispensable tool. Am J Orthop. 1996 Sep;25(9):602-604. [ Links ]
8. Ellerton J, Tomazin I, Brugger H, Paal P, RECM 0024 Immobilization and splinting in Mountain Rescue, Official recommendations of the International Commission for Mountain Emergency Medicine, 2009. [ Links ]
9. American College of Surgeons, American College of Emergency Physicians: equipment for ambulances. 2000. [ Links ]
10. Beningfield S, Potgieter H, Nicol A, van As S, Bowie G, Hering E, Lâtti E. Report on a new type of trauma full-body digital X-ray machine. Emerg Radiol. 2003 Apr;10(1):23-29. [ Links ]
11. Marsh JL, Slongo TF, Agel J, et al. Fracture and Dislocation Classification Compendium 2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma. 2007;21 Supplement 10 pp: S1-S133. [ Links ]
12. Amer M, Thomas E. Initial management of pelvic and femoral fractures in the multiply injured patient. Crit Care Clin. 2004;20:159-70. [ Links ]
13. Irajpour A, Kaji NS, Nazari F, Azizkhani R, Zadeh AH. A comparison between the effects of simple and traction splints on pain intensity in patients with femur fractures. Iran J Nurs Midwifery Res. 2012 Nov;17(7):530-33. [ Links ]
 Correspondence:
Correspondence:
Dr Sithombo Maqungo
Orthopaedic Trauma Service
Groote Schuur Hospital, University of Cape Town
Cell: +27832341723;Tel: +27214043427
email: ithombo@msn.com














