Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.2 Centurion Jun. 2015
http://dx.doi.org/10.17159/2309-8309
HAND
Corticosteroid usage in hand and wrist surgery
MW Solomons
MBChB, FCS(Orth)(SA); Martin Singer Hand Unit, Groote Schuur Hospital, University of Cape Town
INTRODUCTION
Hand and wrist surgery probably leads the other orthopaedic disciplines in corticosteroid usage. Despite widespread usage there still remains some scepticism among patients and surgeons about the 'poison 'of steroid injections. For various (often fiscal!) reasons patients are not offered cortisone injections as a simple, quick and effective conservative option to many common hand/wrist maladies.
Key words: cortisone, corticosteroids, trigger finger, carpal tunnel, De Quervain's
General
How does cortisone work?
Short answer: It interferes with the inflammatory process by blocking cytokine production.
Long answer: Glucocorticoid gets taken up into cell and binds with receptor. This receptor-ligand complex binds to specific genes causing upregulation of annexin-1. Annexin-1 is a potent phospholipase inhibitor that blocks the production of prostaglandins and leukotrienes, the primary mediators of inflammation.
What are the fundamental differences in the different preparations?
There are essentially two different groups: soluble and insoluble. All are derivatives of prednisolone with different side chains or chemical tweaking. The phosphate group are soluble and are absorbed rapidly giving them a short onset of action and a more substantial systemic effect. These include betamethasone sodium phosphate which is one of the components of betamethasone injectable suspension.
The ester side chain group include methylprednisolone acetate injectable suspension and betamethasone acetate which makes up the other component of betamethasone injectable suspension. These compounds are insoluble and tend to aggregate and form crystals that take a while to dissolve and exert their effect. The crystals can irritate the synovium causing substantial discomfort.
What is the risk of sepsis?
The reported incidence ranges from 1 in 3 000 to 1 in 50 000. The author advocates a 'no-touch' technique to minimise the risk of this dreaded complication.
What is the effect on blood sugar?
The literature is confusing. Most suggest there will be some hyperglycaemic effect in IDDM patients for as much as five days. They should be warned to keep a close eye on control.
The author advocates a 'no-touch' technique to minimise the risk of the dreaded complication of sepsis
Any other risks or side effects?
One common, one rare. About 25% of patients will develop an acute post-injection flare. It is the author's opinion that this is much more substantial and dramatic with methylprednisolone acetate injectable suspension than betamethasone injectable suspension. It can present as a sepsis-like presentation with pain, redness and warmth. Sometimes the acetate component of betamethasone injectable suspension can precipitate a similar but usually less dramatic clinical picture.
A rare complication is hypopigmentation and skin atrophy at the injection site. It is more common with subcutaneous injections (De Quervain's and trigger) than with intra-articular injections.
Trigger digit
Why does it occur?
Following mechanical trauma the inner gliding layer of the pulley undergoes chondroid metaplasia ultimately replacing it with fibrous tissue. In other words the pathology is in the pulley not the tendon or tenosyn-ovium.
What is the term tenovaginitis?
As the 'inflammation' is in the pulley rather than the tendon or tenosynovium, a better name for trigger finger is tenovaginitis.
If no synovitis then why do steroids work?
Hyperplasia of the outer vascular layer ultimately invades the inner layer causing thickening. This process must be cytokine-mediated inflammation. Steroids will reverse the thickening of the pulley.
Is it necessary to inject into the sheath?
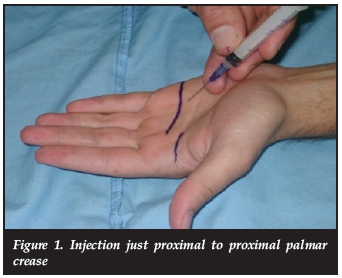
A study by Taras et al. showed no benefit to injecting the bolus under the pulley into the sheath versus injecting outside the sheath (Figure 1)}
What are the results in the literature?
Sixty to 90% positive long-term response to cortisone injections depending on who you read. Worse results are reported in diabetics and in triggering going on for more than 4 to 6 months. Obviously it becomes difficult for the steroids to reverse the fibrocartilaginous metaplasia once it has occurred.
Any point in a second or third injection?
Yes! It has been shown that there can be a 36% positive response to a second injection. A study by Benson and Ptaszek showed no response to a third injection.2
Are there risks associated with injection?
Raised blood sugar in diabetics for up to five days so warn them. Tendon rupture very, very rare. Despite widespread usage only a handful of cases have been reported.
De Quervain's
Why does it occur?
Once again the pathology of De Quervain's is myxoid degeneration rather than acute inflammation. The tendon sheath can be five times thicker than normal. The incidence of a separate sub-sheath for EPB is 70% in patients with De Quervain's versus 20% in a random selection of cadavers.3 Careful exploration at the time of surgery is therefore mandatory to ensure a successful outcome.
What is the natural history?
In a study by Schnellen and Ring,4 95% of patients offered non-interventional treatment including splints and NSAIDs had symptom resolution by one year. A separate study with 6-month follow-up resulted in only 36% resolution in the splint-alone group. Although the natural history is incompletely understood, de Quervain's tenosynovitis seems to be self-limited in the majority of patients.
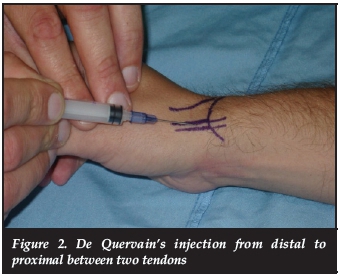
Results of steroid injection?
Effective in 75% to 85%! (Figure 2)
Does ultrasound help in guiding the injection?
Yes it appears so. At least two studies show improved outcomes with US-guided injection techniques. It is the author's opinion that the cost and hassle does not justify the marginal increase in efficacy.56
What about splints?
In a three-armed study, Weiss et al. studied the use of corti-costeroid injections and splinting together and separately to determine their clinical effect. They observed a 67% improvement with injection alone, 57% improvement with both injection and splinting, and 19% improvement with splinting alone.7
Carpal tunnel
What are the risks of injecting the carpal tunnel?
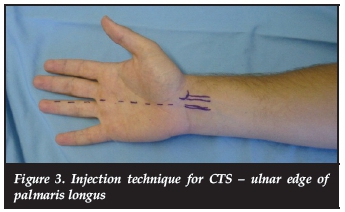
Other than the risks of systemic corticosteroids as mentioned earlier, the author has seen numerous cases of inadvertent intraneural injection. While all resolved over time, the pain and temporary neurological deficit was a substantial cause of treatment morbidity.
Any severe pain at the time of injection or resistance while injecting may be an indication of an intra-neural position of the needle. If this occurs, immediately remove the needle and reinsert in a more ulnar direction (Figure 3). A carpal tunnel injection should not be painful!
What are the long-term benefits?
It is widely accepted that no more than 10 to 15% of patients with clinically suspected CTS will have long-term meaningful response to cortisone injections.8 In certain self-limiting conditions such as pregnancy, cortisone injections can temporise while awaiting resolution.
What about using injections for diagnosis?
Patients whose symptoms improve after a steroid injection to the carpal tunnel also have a significantly better response to surgery than those who do not respond to the injection.
TFCC tears
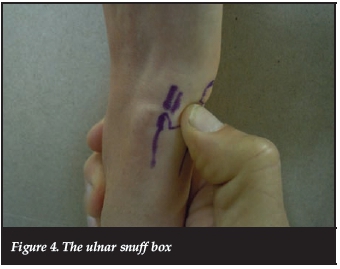
How do I make the diagnosis?
Point tenderness deep in the ulnar snuff box (Figure 4) and pain on end range supination and/or pronation. Note that the literature mentions pain on end range pronation being more specific but it is the author's opinion and experience that this is incorrect.
A carpal tunnel injection should not be painful!
Injection techniques
There are no papers in the literature reporting the techniques and outcomes of TFCC injection. The author prefers an injection from mid lateral on the ulnar side immediately volar to the ECU tendon. The ulnar-sided joint should accept a 2 to 3 cm bolus without any resistance.
My outcomes?
The author presented a series of injections for TFCC pain at the SASSH and SAOA meeting 2013. He reports 60% resolution after a single injection and a further 28% of patients were only occasionally symptomatic and did not require any further intervention.
What does the literature say?
Preciously little. The wrist literature is replete with every conceivable form of operative intervention including open and arthroscopic debridements and repair.
Is there a place for MRI?
Lordache9 took 103 asymptomatic volunteers and submitted them to MRIs. The TFCC was reported as abnormal in 39 with 23 reported as having a complete tear!
Haims et al. reported on MRI arthrography having a sensitivity of 17%, specificity of 79% and an accuracy of 64%.10
Base of thumb arthritis
Do steroids work?
Studies continue to show statistical improvement in pain scores from baseline but a prospective randomised blinded study out of New York failed to show any difference between steroid, hyaluronic acid and placebo!11 The author's experience is that the average response is 4 to 6 weeks with about 20% of patients reporting long-term effects.
In a study by Day et al.,12steroid injection with splinting for the treatment of basal joint arthritis of the thumb provided reliable long-term relief in thumbs with Eaton stage 1 disease but provided long-term relief in only seven of 17 thumbs with Eaton stage 2 and stage 3 basal joint arthritis.
Dorsal wrist syndrome
What is it?
DWS is a clinical entity of dorsal wrist pain directly over the dorsal scaphol-unate interosseous ligament (Figure 5). The pain is exacerbated by loading in wrist extension such as a push-up. It represents an irritation of the terminal fibres of the posterior interosseous nerve by bony impingement or an occult dorsal wrist ganglion.
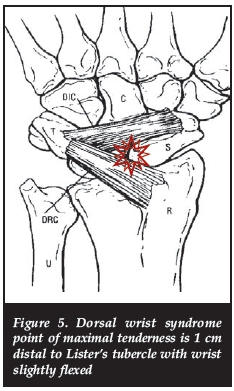
Treatment?
Eighty-six per cent good and excellent results after one or two cortisone injections into the point of maximal discomfort on the dorsum of the wrist.
Conclusion
Accurate diagnosis is critical. Obviously steroid injections can only offer a therapeutic option if the clinical problem is correctly identified and attention is placed on accurate placement of the needle. Steroid injections play a pivotal role in the conservative management of soft tissue and joint wrist and hand conditions. Fifty to 90% of patients can be expected to have meaningful long-term effects.
Failure to incorporate this modality into your practice must be construed as over-servicing.
The content of this article is the sole work of the author. No benefits of any form have been or are to be received from a commercial party related directly or indirectly from this article.
References
1. Taras JS, Raphael JS, Pan WT, Movagharnia F, Sotereanos DG. Corticosteroid Injections for Trigger Digits: Is Intrasheath Injection Necessary? J Hand Surg Am. 1998 Jul;23A(4):712-22. [ Links ]
2. Benson LS, Ptaszek AJ. Injection versus surgery in the treatment of trigger finger. J Hand Surg 1997;22A:138-44. [ Links ]
3. Alemohammad AM, Yazaki N, Morris RP, Buford WL, Viegas SF. Thumb interphalangeal joint extension by the extensor pollicis brevis: association with a subcom-partment and de Quervain's disease. J Hand Surg 2009;34A:719-23. [ Links ]
4. Ring D, Schnellen A. Patient-centered care of de Quervain's disease. J Hand Microsurg. 2009;1(2):68-71. [ Links ]
5. McDermott JD, Ilyas AM, Nazarian LN, et al. Ultrasound-guided injections for de Quervain's tenosynovitis. Clin Orthop Relat Res.2012;470(7):1925-31. [ Links ]
6. Kume K, Amano K, Yamada S, et al. In de Quervain's with a separate EPB compartment, ultrasound-guided steroid injection is more effective than a clinical injection technique: a prospective open-label study. J Hand Surg Eur Vol. 2012;37(6):523-27. [ Links ]
7. Weiss AP, Akelman E, Tabatabai M. Treatment of de Quervain's disease. J Hand Surg 1994;19A:595-59. [ Links ]
8. Graham RG, Hudson DA, Solomons MW, Singer M. A prospective study to assess the outcome of steroid injection and splinting for the treatment of carpal tunnel syndrome. Plast Reconstr Surg. 2004 Feb; 113(2);550-56. [ Links ]
9. Lordache Sd, Rowan R, Garvin GJ, Osman S, Grewal R, Faber KJ. Prevalence of triangular fibrocartilage complex abnormalities on MRI scans of asymptomatic wrists. J Hand Surg Am. 2012 Jan;37(1):98-103. [ Links ]
10. Haims AH, Schweitzer ME, Morrison WB, Deely D, Lange R, Osterman AL, Bednar JM, Taras JS, Culp RW. Limitations of MR imaging in the diagnosis of peripheral tears of the TFC of the wrist. AJR Am J Roentgenol. 2002 Feb;178(2):419-22. [ Links ]
11. Heyworth BE, Lee JH, Kim PD, Lipton CB, Strauch RJ, Rosenwasser MP. Hylan Versus Corticosteroid Versus Placebo for Treatment of Basal Joint Arthritis: A Prospective,Randomized, Double-Blinded Clinical Trial. J Hand Surg Am. 2008 Jan; 33(1):40-48. [ Links ]
12. Day CS, Gelberman R, Patel AA, Vogt MT, Ditsios K, Boyer MI. Basal joint osteoarthritis of the thumb: A prospective trial of steroid injection and splinting. J Hand Surg Am. 2004 Mar;29(2):247-51. [ Links ]
 Correspondence:
Correspondence:
Dr MW Solomons
H49 OMB
Groote Schuur Hospital
Anzio Rd
Observatory
Cape Town














