Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.2 Centurion Jun. 2015
http://dx.doi.org/10.17159/2309-8309
PAEDIATRICS
Dysplasia epiphysealis hemimelica: An interesting case report involving the talus and literature review
N KrugerI; D ThompsonII
IMBChB(UCT), MSc Diagnostic Imaging (OXON), MSc Orth (OXON); Orthopaedic registrar, University of KwaZulu-Natal, Pietermaritzburg Hospital Complex
IIMBChB(UCT), FRCS(Glas); Principal Specialist in Paediatric Orthopaedics, University of KwaZulu-Natal, Grey's Hospital, Pietermaritzburg
ABSTRACT
Dysplasia epiphysealis hemimelica (DEH) is a rare osteochondromatous condition arising unilaterally from an epiphysis in the developing skeleton. Unhindered, this osseocartilaginous lesion continues to grow until skeletal maturity. Characteristic radiographic features are usually sufficient to make the diagnosis. One common site of occurrence is the talus, which has the potential to cause pain, joint deformity or limit range of motion. We report a case of DEH of the talus causing fixed hindfoot valgus deformity, successfully treated with surgery, and review the literature on DEH and its current treatment strategies.
Key words: valgus hindfoot, dysplasia epiphysealis hemimelica, Trevor disease, talus, bone dysplasia
Introduction
Affecting approximately only one in 1 million patients, dysplasia epiphysealis hemimelica (DEH), or Trevor disease, is a rare developmental disorder of the evolving skeleton resulting in asymmetric overgrowth of epiphyseal cartilage. Mouchet and Belot initially termed it 'tarsomegalie', referencing the tarsus as a common site of its occurrence. Trevor then later described 'tarsoepiphyseal aclasis' when referring to this osteochondromatous lesion of the epiphysis.1 Both these names ultimately fell out of favour due to the much broader distribution of DEH, and Fairbank was credited with coining the current term in 1956.2 We present a case of DEH of the talus causing fixed hindfoot valgus deformity and describe the condition and its current treatment strategies.
Case report
An 11-year-old girl presented with a painful left medial ankle mass. It was first noticed as a painless growth two years prior and had since slowly enlarged. There was no history of trauma or family history of similar growths, bone dysplasias or metabolic bone diseases. The child was fully immunised, had no significant childhood illnesses and was HIV-negative. No other joints were involved.
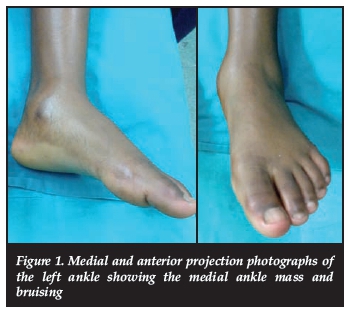
Clinically pathology was confined to the left ankle, with a tender bony growth just inferior to the medial malleolus. The lesion measured approximately 6 cm x 4 cm, with bruising visible over and just inferior to the medial malleolus. The hindfoot was held in fixed valgus of 20° and could not correct to neutral. Dorsiflexion was limited by 10° but there was no inhibition of plantar flexion (Figure 1).
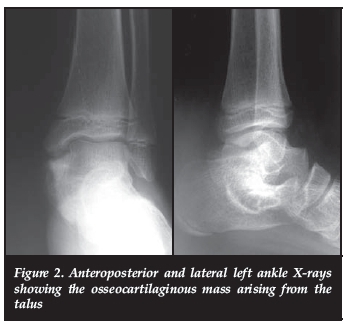
The tendons of tibialis posterior, flexor digitorum longus and flexor hallucis longus were all mildly tender to palpation but no neurovascular fallout was noted. Routine blood work-up was normal. Routine ankle X-rays revealed a bony exostosis that appeared to be originating from the talus and extending medial and cephalad to abut the medial malleolus (Figure 2).
CT and 3D-CT were done to delineate the exact origin and extent of the mass, and to define the osseous from the cartilaginous component. It identified a pedunculated mass arising from the anteromedial border of the talus and extending inferiorly to involve the subtalar joint. This confirmed a diagnosis of DEH (Figures 3 and 4).
Surgery and outcome
Surgical excision was undertaken for pain and fixed valgus hindfoot deformity. We carried out a formal excisional biopsy through a submalleolar C-shaped skin incision. The deltoid ligament was reflected from its tibial insertion, leaving a cuff of tissue for repair. The lesion was macroscopically excised completely and sent for histology. Although this looked pedunculated on the CT scan, it appeared sessile at surgery with no clear demarcation of normal from abnormal bone. This made confident complete excision difficult, and she is at risk for recurrence (Figure 5).
Following excision, the ankle and sub-talar joints had full range of movement. Post-operatively a below-knee cast was applied to protect the deltoid ligament, and changed to a walking cast at 2 weeks for another 4 weeks.
It identified a pedunculated mass arising from the anteromedial border of the talus and extending inferiorly to involve the subtalar joint
The child regained full movement within weeks, and has maintained this with no sign of recurrence at 1 year. Annual follow-up is recommended to monitor for recurrence.
Discussion
Background
DEH occurs peri-articularly, with the ankle being involved approximately a third of the time.3 The other common site is around the knee, with cases involving the upper limbs being significantly less frequent. The disease is overwhelmingly hemimelic, normally confined to the medial or lateral half of the epiphysis in a single limb.4 The medial epiphysis is twice as commonly affected as the lateral,5 and predominantly only a single epiphysis within a limb is affected. It may however occur in multiple epiphyses within the same limb, and rare cases of bilateral disease have been reported.6,7
Unhindered, DEH's natural course is to enlarge until closure of the physes. The usual age of manifestation is between two and 14 years8 and, in contrast to our case, males are affected three times more commonly than females.9 Presentation is usually that of a slow-growing painless mass either on the medial or lateral side of the ankle or knee. In the ankle, the lesion most commonly originates from the talus. Subsequent extension into the subtalar joint or progressive medial growth impinging on the medial malleolus either limits range of motion or produces progressively worsening joint deformity.
Its aetiology remains elusive. Older theories have included dysregulation of cartilage proliferation,10 or Fairbank's original pre- or post-axial apical limb bud disturbance in utero.2 However, more recently published data suggests dysregulation of resident chondroprog-enitor cells11 to be the cause, and lends weight to Connor et al.'s dysregulation of cartilage proliferation theory.10
Classification
DEH has been classified by Azouz et al. into three main forms:5
1. A localised form affecting only one epiphysis
2. A classic form, affecting more than one epiphysis in the same limb
3. A generalised form in which the entire limb is affected.
More recent authors have concentrated on identifying whether or not the lesion is intra- or extra-articular.12 Rosero et al. however emphasise that, as most lesions are intracapsular, the terms 'articular' and 'juxta-articular' are more appropriate in defining their exact location as this has relevance to the joint-deforming potential of the growth.3 Extracapsular lesions are by definition extra-articular.
Diagnosis
Besides the clinical features highlighted above, the diagnosis ultimately relies on typical radiographic characteristics. X-ray usually shows an irregular ossified mass protruding from the epiphyseal cartilage. Initially this mass is cartilaginous, but multiple ossification centres then develop and become confluent with the underlying bone.3 CT is useful in differentiating the cartilaginous component from its bone origin, but this has largely been replaced by MRI as the investigation of choice for defining the extent of the lesion, condition of the articular cartilage and any existing joint deformity. Bone scintigraphy has also shown increased uptake in the cartilage mass and has been proposed as a useful screening investigation to determine whether localised or polyostotic.13
Histology confirmed the diagnosis showing features of an osteochondroma originating from the epiphysis.
Management
Individualised treatment strategies need to be instituted on a case-by-case basis, depending on the location, extent and specific presenting problem.
In patients where there is no articular involvement or pain, observation of the lesion is recommended.4 Patient understanding of their pathology is paramount, as early surgical excision for cosmesis carries both surgical risk and that of recurrence. It is preferable to delay surgery to as near skeletal maturity as possible. Judicious longitudinal follow-up is also safe, as no cases of malignant transformation have been reported.4
If articular problems and pain are prominent, surgery is indicated. Initially, surgical treatment favoured extensive resection, with removal of the cartilaginous articular surface in older patients whose secondary ossification centres had fused with the epiphyses.14 This is in contrast to present practice, where preservation of as much normal articular cartilage is desired, in order to avoid early osteoarthritis or even subsequent arthrodesis.3,9
The diagnosis ultimately relies on typical radiographic characteristics. X-ray usually shows an irregular ossified mass protruding from the epiphyseal cartilage
Specific to DEH of the talus with extension into the subtalar joint, excisional objectives should be the restoration of normal ankle and subtalar joint congruity, with maximum preservation of articular cartilage and removal of all mass inhibiting the range of motion. Both surgeon and patient need to be aware that the operation may need to be repeated prior to skeletal maturity, ultimately attempting to avoid irreversible joint degeneration. Bakerman et al. even recommend annual ankle MRI to identify developing joint incongruity and surgically correct it prior to 'secondary adaptive changes' within the joint.9 Excision of talar DEH provides improved subjective and functional outcome in ankle function,9 but any articular component excision carries the risk of early osteoarthritis. Smaller and juxta-articular lesions have better outcomes and hence early presentation is desirable. In select cases of advanced disease with severe joint destruction, early primary arthrodesis may be the treatment of choice.
Conclusion
Dysplasia epiphysealis hemimelica of the talus is a typical site of occurrence, but extension into the subtalar joint uncommon and disabling. Intra-articular extension causing pain, joint destruction or reduced mobility mandates surgical excision while attempting to preserve all normal articular cartilage. Subsequent risk of recurrence is significant, with accurate delineation between normal and abnormal cartilage difficult. Judicious follow-up until skeletal maturity is recommended.
Informed signed consent was obtained from the mother of the patient for publication of this work. All figures and investigative procedures have been anonymised and patient records are kept on site at the hospital as per hospital data access restrictions.
The content of this article is the original work of the authors. No commercial or other benefits have been or are to be received directly or indirectly related to the publication of this work.
References
1. Trevor D. Tarso-epiphysial aclasis. J Bone Joint Surg (UK) 1950;32B-2:204-13. [ Links ]
2. Fairbank T. Dysplasia epiphysealis hemimelica. J Bone Joint Surg (UK) 1956;38B-1:237-57. [ Links ]
3. Rosero V, Kiss S, Terebessy T, Köllö K, Szöke G. Dysplasia epiphysealis hemimelica (Trevor's disease): 7 of our own cases and a review of the literature. Acta Orthopaedica 2007;78-6:856-61. [ Links ]
4. Azzoni R. Dysplasia epiphysealis hemimelica of the talus. J Orthopaed Traumatol 2009;10-1:43-46. [ Links ]
5. Azouz E, Slomic A, Marton D, Rigault P, Finidori G. The variable manifestations of dysplasia epiphysealis hemimelica. Paediatric Radiology 1985;15-1:44-49. [ Links ]
6. Merzoug V, Wicard P, Dubousset J, Kalifa G. Bilateral dysplasia epiphysealis hemimelica: report of two cases. Paediatric Radiology 2002;32-6:431-34. [ Links ]
7. Takegami Y, Nogami H. A case of bilateral dysplasia epiphysealis hemimelica associated with polydactyly and syndactyly. Clin Orthop Relat Res 1993;296:307-309. [ Links ]
8. Silveira R, Lopes F, Reis A, Granzotto E, Oliveira A. Dysplasia epiphysealis hemimelica (Trevor-Fairbank disease): case report. Radiologia Brasileira 2013;46(1):59-60. [ Links ]
9. Bakerman K, Letts M, Lawton L. Dysplasia epiphysealis hemimelica of the ankle in children. Canadian Journal of Surgery 2005;48(1):66-68. [ Links ]
10. Connor J, Horan F, Beighton P. Dysplasia epiphysialis hemimelica. A clinical and genetic study. J Bone Joint Surg (UK) 1983;65B-3:350-54. [ Links ]
11. Perl M, Brenner R, Lippacher S, Nelitz M. Case report: Dysplasia epiphysealis hemimelica: a case report with novel pathophysiologic aspects. Clin Orthop Relat Res 2009;467(9):2472-78. [ Links ]
12. Acquaviva A, Municchi G, Marconcini S, Mazzarella F, Occhini R, Toti P, Mazzei M, Volterrani L. Dysplasia epiphysealis hemimelica in a young girl: role of MRI in the diagnosis and follow-up. Joint Bone Spine 2005;72(2):183- 86. [ Links ]
13. Teixeira A et al. Scintigraphic findings of dysplasia epiphysealis hemimelica: a case report. Clin Nucl Med 2001;26(2):162. [ Links ]
14. Fasting O, Bjerkreim I. Dysplasia epiphysealis hemimelica. Acta Orthopaedica Scand 1976;47:217-25. [ Links ]
 Correspondence:
Correspondence:
Dr Neil Kruger
162 Waltdorf Complex
771 Townbush Road
Montrose
3201 Pietermaritzburg
Email: neilkruger6@gmail.com
Tel (w): 033 897 3000
Tel (h): 033 347 0979














