Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.2 Centurion Jun. 2015
http://dx.doi.org/10.17159/2309-8309
SHOULDER
Sonographic assessment of the shoulders in asymptomatic elderly diabetics in a Nigerian population
E UchenduI; OO AyoolaII; VA AdetiloyeIII; RT IkemIV; IC IkemV
IMBBS; Senior Registrar, Radiology Department, Obafemi Awolowo University, Ile-Ife, Osun State 230001, Nigeria
IIMBChB, FMCR; Senior Lecturer, Radiology Department, Obafemi Awolowo University, Ile-Ife, Osun State 230001, Nigeria
IIIMBBS, FWACS, FMCR; Professor, Radiology Department, Obafemi Awolowo University, Ile-Ife, Osun State 230001, Nigeria
IVBM BCh, FMCP, FACE; Associate Professor, Endocrinology Unit, Department of Internal Medicine, Obafemi Awolowo University, Ile-Ife, Osun State 230001, Nigeria
VBM BCh, FMCS Orthop, FWACS, FICS; Associate Professor, Department of Orthopaedics and Traumatology Obafemi Awolowo University, Ile-Ife, Osun State 230001, Nigeria
ABSTRACT
BACKGROUND: There is an increased risk of developing shoulder lesions in diabetics especially with increasing age. Ultrasonography provides a low risk and cost effective method of evaluating shoulder disorders in the general population.
METHODS: This is a study of 60 diabetic subjects and 60 controls that were asymptomatic of shoulder joint disease. An ultrasound examination of both shoulders was performed according to standard protocol. Data were analysed using the SPSS data analysis software.
RESULTS: Of the 60 diabetic subjects, 32 were male and 28 were female, while there were 35 males and 25 females in the subject group. Supraspinatus (SST) tendon thickness was greater in diabetics than in controls, (6.44 ± 1.00 mm vs 5.25 ± 0.87 mm, P = 0.000) and (6.02 ± 0.90 mm vs 5.06 ± 0.81 mm, P = 0.000) in the dominant and non-dominant shoulders respectively. Biceps tendon (BT) thickness was also significantly greater in diabetics (4.16 ± 0.57 mm vs 3.20 ± 0.49 mm, P = 0.000), and (3.99 ± 0.48 mm vs 3.99 ± 0.48 mm, P = 0.000) in the dominant and non-dominant shoulders respectively.
CONCLUSION: There was an increase in asymptomatic shoulder pathology in diabetic patients that was associated with ageing.
Key words: diabetes mellitus, elderly, shoulder, sonography, asymptomatic
Introduction
The upper limbs perform diverse functions related to activities of daily living, sports and labour. This occurs due to the considerable range of motion of the shoulder. The shoulder is a complex of muscles, tendons and bony articulations that allow greater mobility than in any other joint in the human body. However, this mobility is achieved at the cost of structural stability.1
Diabetes mellitus is a chronic metabolic condition characterised by persistent hyperglycaemia with resultant morbidity and mortality related to its associated microvascular and macrovascular complications. This can affect the shoulder in several ways as part of its effect on the glycation of musculoskeletal system. This has made shoulder pathology more common with diabetics than the general population.2-4 The lesions identifiable around the shoulder on ultrasonography include rotator cuff and biceps muscle tears, subacromial/subdeltoid bursa (SAD) and biceps tendon effusions along with tendon thickening or thinning.56 These findings are largely as a result of tendon degeneration which is due to tendon overload, leading to microscopic collagen fibre failure and a failed healing response. It should be noted that inflammation is not part of the pathologic process, because inflammatory cells are not seen in biopsies obtained at the time of surgery in the patients.7
Imaging methods used for the assessment of the shoulder includes plain radiography, single or double contrast arthrography, sonography, magnetic resonance imaging (MRI), magnetic resonance (MR) arthrography and CT arthrography. MRI and ultrasound remain the preferred imaging modalities as they have better soft tissue resolution for the non-bony components of the shoulder and do not involve radiation. Ultrasound is however less expensive and more accessible than MRI, which is a very important factor to be considered in evaluation of patients especially against the background of living in a developing world, low-income country with limited resources.
Subjects and methods
This is a prospective, non-randomised, cross-sectional case-controlled study which was carried out in a Nigerian tertiary hospital between August 2011 and May 2012. The study population consisted of 60 diagnosed type II diabetic subjects and 60 age- and sex-matched controls. Approval for the study was obtained from and approved by the (local) OAUTHC Ethical and Research Committee.
MRI and ultrasound remain the preferred imaging modalities as they have better soft tissue resolution for the non-bony components of the shoulder and do not involve radiation
All study subjects were 50 years and above, had no history of symptomatic shoulder disease either previously or currently, and confirmed having type II DM by WHO criteria;8 they were recruited consecutively from the diabetic outpatient clinic. Control subjects with no history of diabetes and normal fasting blood glucose levels were recruited from apparently healthy volunteers asymptomatic of shoulder disease. An informed consent was obtained from all study participants.
The participants were verified to have healthy and normally functioning shoulders by physical examination in which range of movement of the shoulder in all directions was assessed to be normal and without pain. Exclusion criteria were previous history of trauma or surgery to either of the shoulder joints, renal failure, and a history of steroid or chronic NSAID use. The age of onset of diabetes, hand dominance, previous occupation and hobbies were noted and documented. Previous working activity was classified as either clerical which includes civil servants, teachers, typists (entailing more light work) or non-clerical which includes drivers, traders, light farmers (relatively heavy work). Non-clerical workers were excluded from the study.
Real-time grey-scale ultrasound was performed using a Mindray ultrasound scanner model DC-6 and a variable high-frequency linear array transducer (5 to 10 MHz). All study subjects had ultrasonography of both shoulders using standardised procedure.9-11
The examination was performed by a fourth-year radiology resident, who was blinded to the status of the subjects. Measurements were carried out three times, and the mean values obtained were recorded for each patient. All sonographic images were recorded and copied for repeated reviews and re-evaluation to confirm documented findings.
Data were reported as mean and standard deviation (mean ± SD) for continuous variables, whereas categorical variables were reported as frequencies and percentages. The independent samples i-test was used to compare mean tendon thickness and mean age in diabetics with those of the controls. The Chi-square test was used to evaluate associations between shoulder disease and sex, hand dominance and grouped duration of diabetes. The significance level was determined at p < 0.05. Analyses were done using SPSS, version 16.0. The statistical analysis was done by a qualified statistician and checked by the first author.
Results
The 60 study subjects along with their age- and sex-matched controls did not differ in age, gender and hand dominance for both the diabetic and non-diabetic groups as shown in Table I. The median duration of diabetes among subjects was 5.00 years, ranging from 0.2 to 26 years.

In the diabetic group, the mean duration of diabetes was 4.17 ± 2.57 years in the diabetics that had been diagnosed for less than ten years, while the mean duration was 15.79 ± 3.84 years in diabetics that had the disease for over ten years.
As shown in Table II, the thickness of the supraspinatus tendon (SST) was significantly greater in diabetics (6.44 ± 1.00 mm) compared to controls (5.25 ± 0.87 mm) in the dominant shoulder, (p = 0.000). For the nondominant shoulder SST, the thickness was 6.02 ± 0.90 mm in the diabetic subjects and 5.06 ± 0.81mm in the control group (p = 0.000). Similarly, the tendon thickness of the dominant long head of the biceps tendon (BT) and that of the non-dominant were 4.16 ± 0.57 mm and 3.99 ± 0.48 mm in diabetics and 3.20 ± 0.49 mm and 3.13 ± 0.50 mm in the control group, respectively (p = 0.000).
With regard to the sonographic features indicating tendon degeneration, there were more partial thickness tears in the supraspinatus tendons (SST) compared to the long head of biceps tendons (BT) in both diabetics and controls (Figure 1). Also a greater proportion of diabetics, ten (16.7%) had a significant proportion of partial SST tears compared to controls, three (5.0%) in the dominant shoulder (Table II). All the partial thickness tears were less than 1 cm in size, and no tear of the infraspinatus tendon was observed. Full thickness tears of the SST were demonstrated in two (3.3%) diabetics while full thickness BT tears were noted in one (1.7%) in the same group. No full thickness tear of both tendons was observed in the control group for the dominant shoulder (Table II). The dominant shoulder showed near similar pattern of lesions for both study groups, with BT effusion (41.7% vs 20%) as the commonest sonographic feature of tendon degeneration. In the non-dominant shoulder, the control subjects had BT effusion (36.7%) as the most frequent lesion followed by SAD effusion. The infraspinatus tendon did not show any sonographic features of degeneration in either of the groups (Table II).
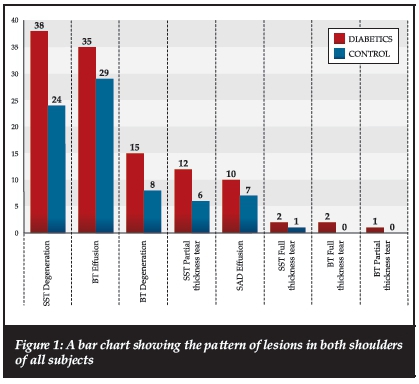
More diabetics than controls had SAD and biceps sheet effusion for both shoulders combined and was significant for dominant side BT effusion (Figure 1, Table II).
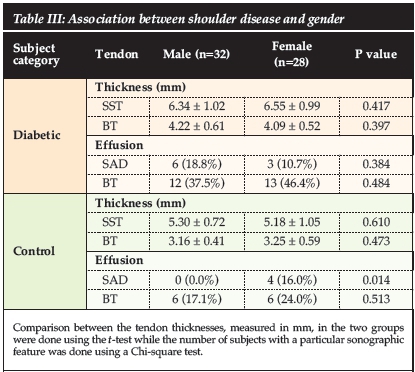
The sonographic features of tendon degeneration elicited in men were generally not different from women in terms of shoulder abnormalities in both study groups. The only significant difference was the higher prevalence of dominant SAD effusion in female controls compared with male controls (16.0% vs 0.0%, p = 0.014) (Table III).
Subjects with more than ten years' duration of diabetes, who were 19 in number, had significantly higher SST thickness than those with less than ten years, who were 41 in number (7.04 ± 0.71 vs 6.16 ± 1.00, p = 0.001) while BT thickness in diabetics was not significantly higher (4.35 ± 0.49 vs 4.07 ± 0.59, p = 0.083). The subjects who had diabetes greater than ten years also had higher prevalence of SAD effusion compared to those with those that had the disease for less than ten years (31.6% [n = 6] vs 7.3% [n = 3], p = 0.014.) BT effusion between both groups were not significantly different but higher in those with diabetes for more than ten years (52.6% [n = 10] vs 36.6% [n = 15]). A positive correlation was also noted between the duration of diabetes and dominant limb tendon thickness with an r value of 0.481 (p = 0.000) for supraspinatus thickness and 0.317 (p = 0.01) for biceps tendon thickness.
There was a positive correlation between the dominant and non-dominant SST thickness with increasing subjects age in the diabetics. The r values were 0.5 (p = 0.000) and 0.51 (p = 0.000) respectively.
The dominant shoulder showed near similar pattern of lesions for both study groups, withBT effusion (41.7% vs 20%) as the commonest sonographic feature of tendon degeneration
Discussion
Rotator cuff disease is a group of diverse conditions with multiple causes and mechanisms of injury, some symptomatic and others non-symptomatic. Theories postulated as to the cause of rotator cuff disease include impingement, normal ageing, avascularity of the tendon, trauma, and compression from narrowing of the acromial space. Several studies have shown an increase in prevalence of shoulder disease, with or without symptoms, in elderly12-15 subjects and in diabetics.2-4,16
This study demonstrated that asymptomatic shoulder lesions were more common in the diabetic subjects than the non-diabetics; this is shown by the significantly greater tendon thickness for both the SST and BT in the dominant and non-dominant shoulders, higher prevalence of the SST partial thickness tears in the dominant shoulder, and the effusion in the BT sheet (Table II). These findings are in concordance with those of other studies.5,17
The significance of these findings is the clinical implications of symptom progression for asymptomatic shoulder lesions, especially rotator cuff tears with time as shown by other investigators.18,19 They observed the development of pains and a decrease in the ability to perform activities of daily living as the natural history of most asymptomatic tears. In one of the studies, 51% of the previously asymptomatic patients became symptomatic over a mean of 2.8 years.18
Abate et al? recorded higher percentages of tears in both the SST and BT with associated higher percentages of effusion in the BT sheet and the SAD when compared to this study. A possible explanation may be related to the difference in races of the subjects used in both studies, raising the possibility of this study group being more resilient to tears, which may agree with the works of Tashjian20 and other investigators21 that showed a strong genetic predisposition for rotator cuff disease.
The BT and SAD effusions observed are strongly associated with tears and are said to be an expression of early reactive inflammation to minimal tendon tears, following minor and unrecognised trauma.22
A good correlation between diabetes and increased shoulder lesions was also emphasised by the demonstration of an increased prevalence of shoulder pathology with the duration of diabetes. This supports the studies which suggested diabetes as a major risk factor in rotator cuff disease.4
The study also showed that there was a positive correlation between age and shoulder pathology as demonstrated by the significant increase in the thickness of the SST in both the dominant and non-dominant shoulders of the diabetics.
A strong suggestion from this study is that diabetes has an effect on the established age-related background tendon lesions as shown by the higher prevalence of tendon pathologies in the diabetics. This supports the studies which suggested diabetes as a major risk factor in rotator cuff disease.4,12
Rotator cuff disease is multi-factored and has been attributed to both intrinsic and extrinsic factors. Extrinsic factors contribute to compression of the rotator cuff tendons, impingement syndrome, while the intrinsic factors result in tendon degradation due to the natural process of ageing,13 poor vascularity,22 altered biology,23 and inferior mechanical properties resulting in damage with tensile or shear loads.24 An inherited predisposition for the development of rotator cuff disease has also been identified.20,21
Ageing and diabetes have a common biochemical mechanism of tendon degeneration secondary to non-enzymatic glycosylation of collagen with formation of advanced glycation end products (AGEs). The AGEs crosslink formation in the collagen fibres affects their physical and chemical properties, reducing their solubility with a resultant tougher, stiffer, less elastic and a weaker matrix.25
Diabetics show excessive glycosylation and cross-linking of the collagens25 and, added to the microvascular complications, may explain the higher prevalence of the rotator cuff and long head of biceps tendon lesions in this group of subjects.
Apart from the unexplained statistically significant higher prevalence of SAD effusion in the female control group, no other significant correlation was observed with the subjects' gender and shoulder pathology which also agrees with other investigators that found no gender difference in the shoulder lesions (Table III).5 This finding is not in keeping with the work of Yamamoto and co-workers15 who established a male preponderance which may be due to the inclusion of both symptomatic and asymptomatic subjects, and the males are more likely to be engaged in heavy labour and have a history of trauma that could cause cuff disease than the females.
Limitations of study
Some limitations to this study must be acknowledged. Assessment of absence of pain and functional impairment was mainly based on patients' judgment making it wholly subjective, as active and passive range of shoulder motion was not objectively measured. Secondly, the researcher was not blinded to the status of both subject groups which may increase the chance of bias.
Conclusion
There is an increase in the prevalence of asymptomatic shoulder pathology in diabetics that is aggravated by ageing. Real-time ultrasound with its high sensitivity and specificity, provides a well-tolerated, convenient and cost-effective method of evaluating these shoulder lesions.
References
1. Schenkman M, De Cartaya VR. Kinesiology of the shoulder complex. J Orthop Sports Phys Ther. 1987;8:438-50. [ Links ]
2. Aydeniz A, Gursoy S, Guney E. Which musculoskeletal complications are most frequently seen in type 2 diabetes mellitus? J Int Med Res. 2008;36(3):505-11. [ Links ]
3. Viikari-Juntura E, Shiri R, Solovieva S, Karppinen J, Leino- Arjas P, et al. Risk factors of atherosclerosis and shoulder pain-is there an association? A systematic review. Eur J Pain 2008;12(4):412-26. [ Links ]
4. Cole A, Gill TK, Shanahan EM, Phillips P, Taylor AW, et al. Is diabetes associated with shoulder pain or stiffness? Results from a population based study. J Rheumatol 2009;36(2):371-77. [ Links ]
5. Abate M, Schiavone C, Salini V. Sonographic evaluation of the shoulder in asymptomatic elderly subjects with diabetes. BMC Musculoskeletal Disorders 2010;11:278. [ Links ]
6. Zanetti M, Hodler J. Imaging of degenerative and posttraumatic disease in the shoulder joint with ultrasound. Eur J Radiol. 2000;35:119-25. [ Links ]
7. McKee, Jennie. Rethinking tendinopathy treatments. AAOS Now, 2011;5:8. [ Links ]
8. World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications; Part 1: Diagnosis and classification of diabetes mellitus. Department of Noncommunicable Disease Surveillance, Geneva, 1999. [ Links ]
9. American College of Radiology. ACR practice guideline for the performance of a shoulder ultrasound examination. ACR Practice Guideline, 2006;867-70. [ Links ]
10. American Institute of Ultrasound in Medicine. AlUM Practice Guideline for the performance of a shoulder ultrasound examination. J Ultrasound Med. 2003;22:1137- 41. [ Links ]
11. Papatheodorou A, Ellinas P, Takis F, Tsanis A, Maris I, et al. US of the shoulder: rotator cuff and non-rotator cuff disorders. Radiographics 2006;26(1):e23. [ Links ]
12. Northover JR, Lunn P, Clark DI, Phillipson M. Risk factors for the development of rotator cuff disease. Int J Shoulder Surg. 2007;1:82-86. [ Links ]
13. Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8(4):296-99. [ Links ]
14. Schibany N, Zehetgruber H, Kainberger F, Wurnig C, Ba-Ssalamah A, et al. Rotator cuff tears in asymptomatic individuals: a clinical and ultrasonographic screening study. Eur J Radiol. 2004;51(3):263-68. [ Links ]
15. Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116-20. [ Links ]
16. Arkkila PE, Kantola IM, Viikari JS, Ronnemaa T. Shoulder capsulitis in type I and II diabetic patients: Association with diabetic complications and related diseases. Ann Rheum Dis. 1996;55(12):907-14. [ Links ]
17. Mujde A, Selma K, Mahmut K, Osman M. Thickness of the supraspinatus and biceps tendons in diabetic patients. Exp Clin Endocrinol Diabetes 2007;115:92-96. [ Links ]
18. Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, et al. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199-203. [ Links ]
19. Mall NA, Kim HM, Keener JD, Steger-May K, Teefey SA, et al. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010;92:2623-33. [ Links ]
20. Tashjian RZ, Farnham JM, Albright FS, Teerlink CC, Cannon-Albright LA. Evidence for an inherited predisposition contributing to the risk for rotator cuff disease. J Bone Joint Surg Am. 2009;91:1136-42. [ Links ]
21. Harvie P, Ostlere S, Teh J, McNally E, Clipsham K, et al. Genetic influences in the aetiology of tears of the rotator cuff. Sibling risk of a full-thickness tear. J Bone Joint Surg Br. 2004;86:696-700. [ Links ]
22. Rudzki JR, Adler RS, Warren RF, Kadrmas WR, Verma N, et al. Contrast-enhanced ultrasound characterization of the vascularity of the rotator cuff tendon: age- and activity-related changes in the intact asymptomatic rotator cuff. J Shoulder Elbow Surg. 2008;.7(1 Suppl):96S- 100S. [ Links ]
23. Kumagai J, Sarkar K, Uhthoff H. The collagen types in the attachment zone of rotator cuff tendons in the elderly: an immunohistochemical study. J Rheumatol, 1994;21:2096-100. [ Links ]
24. Lake S, Miller K, Elliott D, Soslowsky L. Effect of fiber distribution and realignment on the nonlinear and inhomogeneous mechanical properties of human supraspinatus tendon under longitudinal tensile Loading. J Orthop Res. 2009;27:1596-602. [ Links ]
25. Paul RG, Bailey AJ. Glycation of collagen: the basis of its central role in the late complications of ageing and diabetes. Int J Biochem Cell Biol. 1996;28:1297-310. [ Links ]
 Correspondence:
Correspondence:
Dr OO Ayoola
Department of Radiology Obafemi Awolowo University
Ile-Ife, Osun state 230001
Nigeria
E-mail: oluyoola@gmail.com














