Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.2 Centurion Jun. 2015
http://dx.doi.org/10.17159/2309-8309
SPINE
Primary bone tumours of the spine: Presentation, surgical treatment and outcome
M LaubscherI; M HeldII; RN DunnIII
IMBChB(UFS), Dip PEC, MMed(UCT)Ortho, FC(Orth)(SA); Consultant, Orthopaedic Surgery
IIMD, MMed(UCT)Ortho, FC(Orth)(SA); Consultant, Orthopaedic Surgery
IIIMBChB(UCT), MMed(UCT)Ortho, FC(Orth)(SA); Consultant Spine and Orthopaedic Surgeon, Professor and Head of the Department of Orthopaedics, University of Cape Town. Head: Orthopaedic Spinal Services, Groote Schuur Hospital Spine Deformity Service, Red Cross Children's Hospital. From Groote Schuur Hospital and the Department of Orthopaedics, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Primary bone tumours of the spine are a group of rare tumours that include both benign and malignant lesions. Resection is associated with a high morbidity rate.
METHODS: We retrospectively reviewed all the primary bone tumours of the spine that were surgically treated at our unit between 2005 and 2012 (haematological malignancies were excluded.
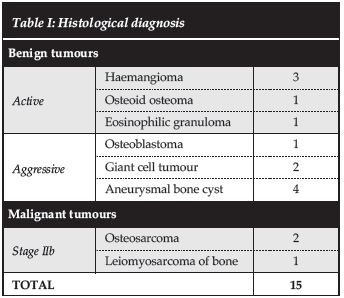
RESULTS: Fifteen cases were included that presented at a median age of 36 years (range 8 to 65 years). Pain was the most common presenting symptom. Three patients had significant neurological deficits at time of presentation and in two cases there was an improvement after surgery. The median delay in diagnosis was 7 months (range 1 to 36 months). A variety of surgical strategies was employed with the use of adjuvant radio- or chemotherapy in six cases. Twelve benign and three malignant tumours were resected. Complications (sepsis, failure of fixation and recurrence) were encountered in five cases (33%).
CONCLUSIONS: Primary bone tumours of the spine are often associated with a significant delay in diagnosis. Surgical strategy should be individualised for each case. Acceptable results can be achieved with this approach.
Key words: primary bone tumour, bone tumour, primary spine tumour, spine tumour, resection
Introduction
Primary bone tumours of the spine are a heterogynous group of conditions that includes both benign and malignant tumours, with only 6% of these tumours considered malignant.1 The spine is a frequent site of metastasis, but primary bone tumours of the spine are rare and make up only 4.2% of spinal tumours.2 Eleven per cent (11%) of primary musculoskeletal tumours occur in the spine2 with certain tumours having an affinity for the spine. Although rare, these tumours offer a considerable diagnostic dilemma and therapeutic challenge. Timely diagnosis is crucial, as immediate attention could affect overall prognosis.3
Primary bone tumours are more common in the thoracic and lumbosacral regions than in the cervical spine.4 These tumours occur according to a typical anatomical distribution within the vertebra. In general, malignant tumours occur more frequently in the anterior elements and benign tumours in the posterior elements.3-5
Primary bone tumours of the spine are rare and offer a considerable diagnostic dilemma and therapeutic challenge
The aims of treatment of these axial neoplasms include complete resection if feasible, preservation of neurological function and stabilisation of the spine.4 In the paediatric age group the growing spine is an added consideration. The quality of evidence that guides treatment is low due to the rarity of these conditions, mostly limited to case series.6-8 Resection of tumours in the spine often leaves large bony defects and is associated with a high morbidity, and complications in up to 35% of patients have been described.9 Both sepsis and mechanical failure are prevalent. Previous papers report a deep sepsis rate of greater than 5%, mechanical failure in 7% and mortality related to the surgery in 2% of cases of en bloc resections in the spine.10 Combined anterior and posterior approaches and number of levels resected are predictors of increased complications.10
The aim of our study was to review the primary bone tumours of the spine treated at our unit regarding the presentation, the surgical strategy employed and the outcome.
Materials and methods
Following Institutional Ethics approval (reference HREC 029/2013) a retrospective review was performed of all the primary bone tumours of the spine that received surgical treatment at our unit from 2005 to 2012. We excluded all haematological malignancies. We treated 15 cases during this period that were included according to these criteria.
A case note and imaging review was done where patient demographics, details of presentation, clinical information and the management strategy were analysed. All complications and mortalities were recorded.
Results
The median age at presentation was 36 years (range 8 to 65 years) with eight male and seven female patients affected. The median follow-up was 18 months (range 3 to 60 months).
The median delay in diagnosis was 7 months (range 1 to 36 months) from the time a medical opinion was first sought to a diagnosis being made. Pain was the most common presenting symptom (15 from 15 cases) and nine cases presented with pain alone. Pain was mostly axial pain in the affected region (11 of 15 cases), although three patients presented with chest pain and one with flank pain. Other presenting symptoms included neurological symptoms and odynophagia. Two patients presented with a recurrence of a benign aggressive tumour following incomplete resection at another unit.
Ten patients had no neurological deficit at time of presentation. Two patients presented with radicular symptoms and another three had significant neurological deficits at time of presentation. Of these three patients, one was graded as a Frankel A, one a Frankel C and one a Frankel D. All three cases with significant neurological deficit were in patients with benign aggressive lesions. Two of these cases had significant improvement after surgery. We had no cases of neurological deterioration following surgery.
We treated 12 benign and three malignant tumours. The histological diagnoses are summarised in Table I.
In all cases the surgery was performed by the senior author. A variety of surgical strategies was utilised. An intralesional resection or debulking of the tumour was performed in six cases and a marginal resection was performed in nine cases (see Table II) to correlate with diagnosis. This was achieved through a posterior only approach in six cases and a combined approach in nine cases. The combined approaches were performed at a single sitting in five and staged in four cases. In 14 patients a fusion was performed. A posterior only fusion was performed in four cases (one uninstrumented and three instrumented) and a combined posterior and anterior fusion was performed in ten cases. In ten cases there were significant bone defects after resecting the tumours. These were addressed with cages with bone graft in five cases and strut allografts in five cases.
Adjuvant therapy was used where indicated. Adjuvant radiotherapy alone was used in four cases, adjuvant chemotherapy in one case and a combination in another one case (Table II).
There were complications in five cases (33%). This included one case of deep sepsis with failure of fixation in the same patient. This required staged revision of instrumentation with the patient symptom free at time of last follow-up. Three cases had spread or recurrence of the tumour. Two of the recurrent cases were in malignant tumours and one in benign aggressive tumour. In the one recurrent malignant tumour a repeat attempted marginal resection was performed. The other two recurrent cases were not re-operated as resection was not possible with acceptable morbidity. We had three deaths in the series.
A variety of surgical strategies was utilised
All three patients with malignant tumours died within the follow-up period at a median of 18 months after surgery (range 3 to 59 months). Death was due to recurrence or spread of the tumours in two cases and unrelated in one case.
The patients' treatment and complications are summarised in Table II. Figures 1 to 3 show examples of cases from the series.
The aims of treatment of these axial neoplasms include complete resection if feasible, preservation of neurological function and stabilisation of the spine
Discussion
The most common presenting complaint of patients with primary tumours is pain, with roughly 60% complaining of axial pain and 25% of radicular symptoms.3 This is confirmed in our series. The presence of a neurological deficit carries a worse prognosis.11 Pain at rest or night pain is red flag symptoms that warrant further investigation. Spinal deformity is obvious when present, but occurs in less than 10% of patients. The most common cause of a painful scoliosis in adolescents is an osteoid osteoma.5
A delay in diagnosis is common and our finding is confirmed in other series.4 This is due to the presenting symptoms often being vague, pain often being the only symptom, and the initial radiographs often only showing subtle or no abnormalities leading to the symptoms not being properly investigated. Most patients report a slow, gradual onset of pain in the involved area. In benign tumours of the spine an average of 26 weeks of symptoms before presentation are reported.4 This was confirmed in our series where the average delay in presentation was 7 months.
A variety of classifications systems is used for primary bone tumours of the spine. The Enneking staging system12 was initially described for primary bone tumours of the appendicular skeleton, but is applied to tumours of the spine as well. It prognosticates as well as guides surgical resection margins and has been validated in the literature.2 The Weinstein-Boriani-Biagini surgical staging system13 is an anatomical classification based on the Enneking system that describes the number of vertebra as well as the number of sectors within a vertebra involved. Recommendations are then made for the most appropriate approach to resection of the lesion. We used the Enneking staging system. According to this system we treated 12 benign and three malignant tumours. Of the benign group five could be classified as active and seven as aggressive.
Appropriate treatment may be observational (Enneking grade 0 latent lesions) or surgical (most other lesions), depending on the level of pain, instability, neurologic compromise and the natural history of the lesion.5 The aims of surgery are complete resection of the lesion where feasible with preservation of neurological function.
In paediatric cases the growing spine is an added consideration.4 Patients should have individualised approaches and treatment plans because of the many variations of natural history, extent and level affected, local and distant spread, neurological deficit, instability, bone defect after resection and whether resection is feasible with acceptable disability.3 We used a variety of surgical strategies customised to the patient and the tumour. The specific surgical strategies are summarised in Table II.
In peripheral malignant sarcomas the most important factor affecting survival is complete resection of the tumour with a wide margin.14-15 There are however no reports prescribing surgical margins in spinal tumours. Traditional intralesional resection in a piecemeal fashion is thought to increase the likelihood of local recurrence. True wide resection would cause unacceptable morbidity as it would involve resecting the segment of spinal cord.
Total en bloc spondylectomy in a single stage from an all posterior approach was described by Tomita.14 Here wide margins are achieved except at the pedicles and occasionally the spinal canal. This approach decreases local recurrence rates.16-18 In benign aggressive lesions surgical eradication also provides the best long-term cure.6,18 We had three cases of local recurrence in our series. Two were in malignant tumours where a marginal resection was performed. The other recurrent case was a thoracic giant cell tumour encapsulating the aorta and forcing the surgeon to perform an intralesional resection.
There are no reports prescribing surgical margins in spinal tumours. Traditional intralesional resection in a piecemeal fashion is thought to increase the likelihood of local recurrence
Recent advances in chemotherapy have led to improved survival in malignant primary bone tumours, including in the spine.15 Adjuvant radiotherapy is indicated in some malignant and benign aggressive lesions.20 The use of local radiotherapy does increase the risk of major local complications, including sepsis.10 We used radio- and chemotherapy in a number of cases (see Table II) as guided by our local oncology unit.
The main limitations of this study are the retrospective character and the relatively small numbers.
We conclude that primary bone tumours of the spine are often associated with a significant delay in diagnosis. Surgical strategy and adjuvant therapy should be individualised for each case. Acceptable results with minimal complications can be achieved with this approach.
The content of the article is the sole work of the authors. No benefits of any form have been or are to be received from a commercial party related directly or indirectly to the subject of the article.
The research has been approved by the local departmental research council and ethics committee (reference HREC 029/2013).
References
1. Boriani S, Biagini R, De Iure F, et al. Primary bone tumors of the spine: a survey of the evaluation and treatment at the Istituto Ortopedico Rizzoli. Orthopedics. 1995;18(10):993-1000. [ Links ]
2. Davis JH. Anatomical classification and surgical considerations: Primary spinal tumours. An overview. South African Med J. 2011;10(3):26-30. [ Links ]
3. Sansur CA, Pouratian N, Dumont AS, Schiff D, Shaffrey CI, Shaffrey ME. Part II: spinal-cord neoplasms-primary tumours of the bony spine and adjacent soft tissues. Lancet Oncol. 2007;8(2):137-47. [ Links ]
4. Beer SJ, Menezes AH. Primary tumors of the spine in children: Natural history, management and long-term follow-up. Spine (Phila Pa 1976). 1997;22(6):649-58. [ Links ]
5. Thakur N a, Daniels AH, Schiller J, et al. Benign tumors of the spine. J Am Acad Orthop Surg. 2012;20(11):715-24. [ Links ]
6. Harrop JS, Schmidt MH, Boriani S, Shaffrey CI. Aggressive 'benign' primary spine neoplasms. Osteoblastoma, aneurysmal bone cyst and giant cell tumour. Spine (Phila Pa 1976). 2009;34(22 Suppl):S39-S47. [ Links ]
7. Fisher CG, Andersson GBJ, Weinstein JN. Spine focus issue. Summary of management recommendations in spine oncology. Spine (Phila Pa 1976). 2009;34(22 Suppl):S2-S6. [ Links ]
8. Fisher CG, Keynan O, Ondra S, Gokaslan Z. Introduction to focus issue in spine oncology: the synthesis of evidence and expert opinion for best practice recommendation. Spine (Phila Pa 1976). 2009;34(22 Suppl):S21-S25. [ Links ]
9. Choi D, Crockard A, Bunger C, et al. Review of metastatic spine tumour classification and indications for surgery: the consensus statement of the Global Spine Tumour Study Group. Eur Spine J. 2010;19(2):215-22. [ Links ]
10. Boriani S, Bandiera S, Donthineni R, et al. Morbidity of en bloc resections in the spine. Eur Spine J. 2010;19(2):231-41. [ Links ]
11. Kelley SP, Ashford RU, Rao AS, Dickson RA. Primary bone tumours of the spine: a 42-year survey from the Leeds Regional Bone Tumour Registry. Eur Spine J. 2007;16(3):405-409. [ Links ]
12. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;153:106-20. [ Links ]
13. Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine: Terminology and surgical staging. Spine (Phila Pa 1976). 1997;22(9):1036-44. [ Links ]
14. Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy: a new surgical technique for primary malignant tumors. Spine (Phila Pa 1976). 1997;22(3):324-33. [ Links ]
15. Gore L, Greffe BS, Rothenberg SS, Erickson M, Schreiber DP, Handler MH. Long-term survival after intralesional resection and multi-modal therapy of thoracic spine osteosarcoma. Med Pediatr Oncol. 2003; (6):400-402. [ Links ]
16. Boriani S, Saravanja D, Yamada Y, Varga PP, Biagini R, Fisher CG. Challenges of local recurrence and cure in low grade malignant tumors of the spine. Spine (Phila Pa 1976). 2009;34(22 Suppl):S48-S57. [ Links ]
17. Sciubba DM, Okuno SH, Dekutoski MB, Gokaslan ZL. Ewing and osteogenic sarcoma: evidence for multidisciplinary management. Spine (Phila Pa 1976). 2009;34(22 Suppl):S58-S68. [ Links ]
18. Yamazaki T, McLoughlin GS, Patel S, Rhines LD, Fourney DR. Feasibility and safety of en bloc resection for primary spine tumors: a systematic review by the Spine Oncology Study Group. Spine (Phila Pa 1976). 2009;34(22 Suppl):S31-S38. [ Links ]
19. Kim HJ, McLawhorn AS, Goldstein MJ, Boland PJ. Malignant osseous tumors of the pediatric spine. J Am Acad Orthop Surg. 2012;20:646-56. [ Links ]
20. Bremnes RM, Hauge HN, Sagsvee R. Radiotherapy in the Treatment of Symptomatic Vertebral Hemangiomas: Technical Case Report. Neurosurgery. 1996;39(5):1054-58. [ Links ]
 Correspondence:
Correspondence:
Dr Maritz Laubscher
Email: maritzl@msn.com














