Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.14 no.1 Centurion Fev./Mar. 2015
TUMOUR
Synovial chondromatosis: A review of the literature and report of two cases
ST RangoakoI; EJ RaubenheimerII; K MafeelaneIII
IMBChB; Department of Orthopaedic Surgery, Faculty of Health Sciences, Medunsa Campus, University of Limpopo
IIMChD, PhD, DSc; Metabolic Bone Disease Laboratory, Faculty of Health Sciences, Medunsa Campus, University of Limpopo
IIIMBChB, FCSA(Orth); Department of Orthopaedic Surgery, Faculty of Health Sciences, Medunsa Campus, University of Limpopo
ABSTRACT
Synovial chondromatosis is a rare benign condition which develops in the synovial tissue of a joint, bursa or tenosynovial sheath. It is characterised by formation of cartilaginous nodules which may enlarge and grow into larger masses. Although radiological imaging contributes to a differential diagnosis, a final diagnosis can only be established with histological examination. Meticulous examination of the lesions is essential in ruling out sarcomatous change. We present a review of the literature and report two cases of synovial chondromatosis of the knee joints diagnosed over a ten-year period in the orthopaedic unit of a tertiary hospital serving mainly an urban- and peri-urban population sample.
Key words: synovium, chondromatosis, knee joint
Introduction and review of the literature
Synovial chondromatosis is a pathological condition in which mesenchymal cell rests in the synovial membrane form one or more cartilage nodules.1,2 Although the pathogenesis remains speculative, various theories have been proposed. Most authors favour the concept of the cartilage masses representing benign neoplastic growths. This is supported by their unrestricted growth potential and tendency to become large,3,4 undergo chondrosarcomatous change,5-8 and recur if incompletely excised.5,9,10 An infective cause for the stimulus to form cartilage in the synovial membrane is discounted by negative cultures obtained from synovial fluid samples.1
Although a significant proportion of patients report trauma as a possible association, the majority give no history of injury of the affected joint.1 An appealing explanation for the presence of cartilaginous masses in the synovium relates to the acknowledged phagocytic capacity of the synovial membrane.10 Fragments of cartilage (and bone) resulting from wearing down of articular surfaces in an osteoarthritic joint may be absorbed by the synovial lining and proliferate in the synovial membrane.1,11 In order for this theory to be plausible, the majority of cases should be reported in elderly patients, which is not the case.
Synovial chondromatosis affects patients over a wide age range reportedly between 17 to 64 years with a peak during middle age,1,5 with degenerative joint disease only present in few.5 The condition is mono-articular and the most common joints involved are the knee followed by the hips.5,12 Several case reports describe lesions involving the temporomandibular joint,2,13-15 joints of the hands,3,10,16 ankle, upper extremity,17,18 hip8 and vertebrae.19 Synovial chondromatosis is more common in males.1,5 Pain and limitation of movement are the most frequently reported presenting symptoms, usually of many years' duration.1,2,7 Large lesions result in pseudo-fusion of the involved joint.3 Intra-articular loose bodies are more frequent in patients with small lesions and may cause locking of the joint. Giant loose intra-articular bodies are rare.4
The typical early radiological appearance is stippled calcification in and around an affected joint. Computed tomography (CT) is the technique of choice for defining the state of the bony surfaces of the articular joint but is inferior to magnetic resonance imaging (MRI) for the identification of non-calcified intra-articular bodies15 and all other structural soft tissue changes.15 Conventional radiographs frequently reveal the typical 'ring-and-arc' appearance following mineralisation of the chondroid mass.12 Erosion of bony facets is frequently seen in synovial chondromatosis.12 Chondrosarcomas develop in up to five per cent of patients with synovial chondromatosis.5,7,20 The histological features of a low grade chondrosarcomas are often ambiguous, and careful clinicopathological correlation is required.21 Biopsy should be performed in cases where malignant transformation is suspected. Microscopic examination should therefore always be supplemented by clinical features indicative of sarcomatous change, which include a clinical history of multiple recurrences,5 sudden enlargement of a lesion6 and radiological findings of endosteal scalloping7 and bone marrow infiltration.12 No MRI features are reported which could be helpful in distinguishing cases with sarcomatous change from synovial chondromatosis alone.20 However MRI is useful in differentiating chondrosarcoma and other bone tumours from synovial chondromatosis and should be viewed as the imaging tool of choice if there is doubt about the diagnosis. Missing a primary malignant bone tumour and performing an intralesional resection leads to extensive tumour contamination with subsequent amputation and poor long-term prognosis. Despite radical surgery, metastatic dissemination has been reported in 29% of cases of synovial chondromatosis with secondary sarcomatous change.8 Other conditions which should be considered in the clinical differential diagnosis of synovial chondromatosis includes pigmented villonodular synovitis, synovial haemangioma, lipoma arborescens21 and all the causes for intra-articular loose bodies such as osteochondral fractures as well as chondrosarcoma and parosteal osteosarcoma.1
The typical early radiological appearance is stippled calcification in and around an affected joint
The principles of treatment of synovial chondromatosis include removal of the tumour(s) using arthrotomy with or without partial synovectomy for large lesions1-3 or arthroscopic removal for small to medium-sized bodies attached to the synovium.18,22 Complete synovectomy is impractical in the knee joint and synovectomy of the hip joint requires dislocation. The latter is not justifiable due to the danger of avascular necrosis of the femoral head secondary to joint dislocation with subsequent fracture. Cases with intra-articular disease have a higher tendency for recurrent growths.16
The purpose of this paper is to report two cases of synovial chondromatosis diagnosed in an orthopaedic unit in a tertiary hospital which serves mainly a rural and peri-urban patient sample of the northern regions of South Africa.
Case 1
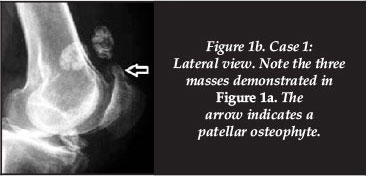
A 60-year-old male employed as a machine operator in a factory was referred to our hospital following a four-year history of severe pain in the left knee, swelling and difficulty in walking due to frequent locking of the joint. Minimal relief was experienced after the use of NSAIDs and analgesics. He consulted traditional healers with no improvement in the condition. His family history was negative and he suffered no associated morbidities. Clinically he presented with significant swelling of the knee and the loose bodies were not palpable. Pre-operative radiographs showed three radiopaque bodies around the knee joint and a patellar osteophyte (Figure 1a and b). Arthroscopic surgery and partial synovectomy of the hypertrophied synovium was performed and two anterior parapatellar tendon portals were used for removal of the three loose bodies.
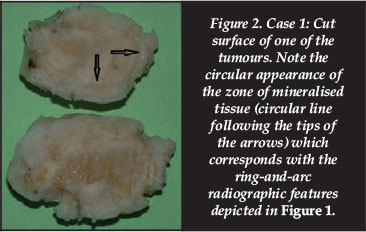
The masses had a smooth surface and white appearance and measured between 2 and 3 cm in diameter. On the cut surface the circular band of mineralised tissue was clearly visible (Figure 2). Due to the presence of mineralised tissue in the specimen, it was demineralised for microscopic processing and sectioning. Microscopically the specimen showed formation of hyaline cartilage in the centre covered by a layer of mineralised bone and fibrous tissue towards the outside. The features were compatible with those of synovial chondromatosis (Figure 3).

Case 2
A 43-year-old unemployed male was referred from a district hospital following a two-year history of progressive pain of the left knee, intermittent swelling, restricted joint movement and frequent locking of the joint. His daily activities were affected due to severe pain and limitation of movement. He reported previous left knee injury during a football game when he was 17 years of age. His family history was negative for bone and joint diseases. Physical examination revealed a mildly swollen tender knee with positive patellofemoral crepitus.
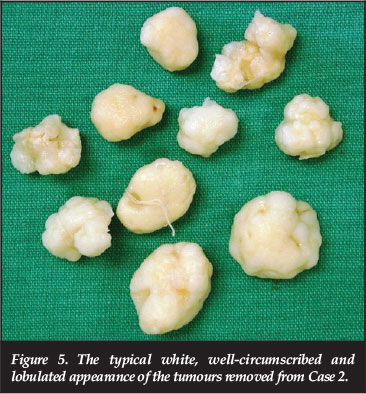
He could fully extend his knee and flex it from 0-85 degrees. Two firm masses were palpable on the anterolateral aspect of the knee. Conventional radiographs showed multiple radiopaque loose bodies associated with the knee joint (Figure 4). Arthroscopy using two anterior parapatellar tendon portals was performed. Ten white, oval, chondritic loose bodies, measuring between 1.9 χ 1.4 cm and 1.1 χ 1 cm in diameter were removed (Figure 5). During the procedure a velvety red appearing and hypertrophied synovium was identified and a partial synovectomy was performed. Microscopic examination showed features resembling those of the lesions in Case 1 and confirmed the diagnosis of synovial chondromatosis. Post-operative radiographs showed no residual bodies. Although the patient experienced slight discomfort and mild swelling after prolonged activity, full function of the joint was restored.

Discussion
Over a period of ten years only two cases of synovial chondromatosis were recorded in our orthopaedic unit, which serves as a referral centre for patients from clinics in the northern and north-western sections of South Africa. This infrequency underscores the rarity of the disease. In both patients the knee joints were affected, supporting the preference for the involvement of the large joints of the lower extremity. Pain and reduced mobility due to locking of the joint were the main complaints of both our patients. Case 2 gave a history of trauma to the joint 24 years before clinical manifestations. Whether this bears any reference to the development of the lesion remains speculative. In the first case, no association with trauma to the knee joint could be recalled by the patient. The ages of both cases fall within the range reported for the disease and both patients are males, supporting the male predominance reported in the literature.1,5 The lesions removed from Case 1 will fall in a category described as 'very large'3 in the literature. The larger lesions tend to mineralise and this facilitates a radiological diagnosis on plain films. The typical ring-and-arc radiological feature12 resulting from the zone of bone formation between the outer fibrous capsule and the core of hyaline cartilage was demonstrated histologically in both our cases, suspending the need for the employment of additional imaging techniques. The histological assessment of the lesions removed is important in ruling out a primary malignant bone tumour, which has disastrous consequences if missed. Our study is the only one in the English literature which demonstrates the macroscopic and microscopic appearances of the ring-and-arc radiological feature resulting from the process of mineralised bone formation within the chondritic bodies in synovial chondromatosis.
Both our cases were treated with arthroscopic surgery and partial synovectomy as the technique offered the advantage of better visualisation, less peri-operative morbidity and the prevention of secondary joint changes such as arthrofibrosis which is more common in open joint surgery. The post-operative follow-up of our patients is short and we can subsequently not comment on the long-term success of the treatment employed.
References
1. Jeffreys TE. Synovial chondromatosis. J Bone Joint Surg 1967;49B:530-34. [ Links ]
2. Reed LS, Foster MD, Hudson JW. Synovial chondromatosis of the temporomandibular joint: a case report and literature review. Cranio 2013;31:309-13. [ Links ]
3. Maramatsu K, Hashimoto T, Tominaga Y, Taguchi T. Large synovial osteochondromas arising from the interphalangeal joint of the thumb: a case report and review of the literature. Anticancer Res 2014;34:1057-62. [ Links ]
4. Sourlas I, Brilakis E, Mavrogenis A, Stravropoulos N, Korres D. Giant intra-articular osteochondromata of the knee. Hippokratia 2013;17:281-83. [ Links ]
5. Davis RI, Hamilton A, Biggart JD. Primary synovial chondro-matosis: a clinicopathologic review and assessment of malignant potential. Hum Pathol 1998;29:683-88. [ Links ]
6. Hallam P, Ashwood N, Cobb J, Fazal A, Heatley W. Malignant transformation of synovial chondromatosis of the knee? Knee 2001;8:239-42. [ Links ]
7. Yao MS, Chang CM, Chen CL, Chan WP. Synovial chondrosarcoma arising from synovial chondromatosis of the knee. JBR-BTR 2012;95:360-62. [ Links ]
8. Campanacci DA, Matera D, Franchi A, Capanna R. Synovial chondrosarcoma of the hip: report of two cases and literature review. Chir Organi Mov 2008;92:139-44. [ Links ]
9. Church JS, Breidahl WH, Janes GC. Recurrent synovial chondro-matosis of the knee after radical synovectomy and arthrodesis. J Bone Joint Surg Br 2006;88:673-75. [ Links ]
10. Loonen MP, Schuurman AH. Recurrent synovial chondro-matosis of the wrist: case report and literature review. Acta Orthop Belg 2005;71:230-35. [ Links ]
11. Murphy FP, Dahlin DC, Sullivan CR. Articular synovial chondromatosis. J Bone Joint Surg 1962;44-A:7. [ Links ]
12. Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics 2007;27:1465-88. [ Links ]
13. Peyrot H, Motoriol PF, Beziat JL, Barthelemy I. Synovial chondromatosis of the temporomandibular joint: CT and MRI findings. Diagn Interv Imaging 2014, Feb 20: (e publication ahead of print). [ Links ]
14. Shah SB, Ramonojam S, Gadre PK, Gadre KS. Synovial chondro-matosis of the temporomandibular joint: journey through 25 decades and a case report. J Oral Maxillofac Surg 2011;69:2795-814. [ Links ]
15. Testaverde L, Perrone A, Caporali L, Ermini A, et al. CT and MR findings in synovial chondromatosis of the temporomandibular joint: our experience and review of the literature. Eur J Radiol 2011;78:414-18. [ Links ]
16. Roulot E, Le Vliet D. Primary synovial osteochondromatosis of the hand wrist. Report of a series of 21 cases and literature review. Rev Rhun Engl Ed 1999;66:256-66. [ Links ]
17. Santiago T, Mariano C. Primary synovial chondromatosis of the ankle joint presenting as a monoarthritis. BMJ Case Rep 2013; Dec 10: pii: bcr2013202186. [ Links ]
18. Griesser MJ, Harris JD, Likes RL, Jones GL. Synovial chondro-matosis of the elbow causing mechanical block to a range of motion: a case report and review of the literature. Am J Orthop 2011;40:253-56. [ Links ]
19. Gallia GL, Weiss N, Cambell JN, McCarthy EF, Tufaro AP, Gokaslan ZL. Vertebral synovial chondromatosis. Report of two cases and review of the literature. J Neurosurg Spine 2004;1:211-18. [ Links ]
20. Wittkop B, Davies AM, Mangham DC. Primary synovial chondromatosis and synovial chondrosarcoma: a pictorial review. Eur Radiol 2002;12:2112-19. [ Links ]
21. Adelani MA, Wupperman RM, Holt GE. Benign synovial disorders. J Am Acad Orthop Surg 2008;16:268-75. [ Links ]
22. Krebs VE. The role of hip arthroscopy in the treatment of synovial disorders and loose bodies. Clin Orthop Relat Res 2003;406:48-59. [ Links ]
 Correspondence:
Correspondence:
Prof E J Raubenheimer
Room FDN 110 Medunsa Campus, University of Limpopo
0204, South Africa
Tel: +27 12 521 4838
Email: Erich.raubenheimer@ul.ac.za