Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.14 n.1 Centurion Feb./Mar. 2015
TRAUMA
Tibial non-union treated with the TL-Hex: A case report
N FerreiraI; F BirkholtzII; LC MaraisI
IMMed(Orth); Tumour, Sepsis Reconstruction Unit, Department of Orthopaedic Surgery, Grey's Hospital, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IIMMed(Orth); Private Practice, Walk-A-Mile Centre, Pretoria
ABSTRACT
Tibial non-unions are difficult to treat, even for the experienced orthopaedic trauma surgeon. Despite being relatively common problems, controversy exists regarding their ideal management. We report a case of a stiff oligotrophic tibial non-union successfully treated with the new TL-Hex (Orthofix, Verona, Italy) circular external fixator. Closed gradual distraction was effective to correct all deformities and stimulate bone formation without the need for a tibial osteotomy or bone graft.
Key words: tibia, non-union, oligotrophic, hexapod, TL-Hex
Background
The tibia in the most commonly injured long bone.1 Due to its anatomical site and subcutaneous location the tibia is often exposed to high-energy trauma, and it is prone to a number of complications including non-union formation.1-4 Along with the severity of injury, many other factors have been implicated in non-union development, including systemic compromise of the host and iatrogenic factors relating to the management of the initial injury.3,5-10
Once established, non-unions are difficult to treat.5,7,11 For the patient, non-unions harbour significant morbidity in terms of financial and emotional compromise.9,12-14 For the healthcare system and treating physician, non-unions demand increased resources, expensive treatment strategies and a meticulous understanding of the underlying disease process.14,15 The optimal management strategy promotes rapid consolidation of the non-union while simultaneously allowing functional rehabilitation of the affected limb.
We report a case of a stiff oligotrophic non-union of the distal tibia that was successfully treated with monofocal distraction with the new TL-Hex (Orthofix, Verona, Italy) circular external fixator.
Case report
A 26-year-old woman was referred to our limb reconstruction unit after failed conservative management of a closed distal third tibia fracture. The fracture was sustained after a fall, six months prior to our consultation. Her initial management consisted of a patella-tendon bearing plaster cast and regular follow-up at her base hospital. At presentation to our unit a stiff tibial non-union with a partially correctable deformity was evident.
Non-unions demand increased resources, expensive treatment strategies and a meticulous understanding of the underlying disease process
Local and systemic staging confirmed the diagnosis of metabolic syndrome X. She was a type 1 diabetic, hypertensive and hypothyroid on treatment. A bone density scan done at the base hospital revealed the patient to be osteopaenic. Radiographs confirmed an oligotrophic non-union of an oblique distal third right tibia fracture with an 11° varus, 9° recurvatum and 22 mm shortening deformity (Figure 1). Full knee and ankle motion was possible and no vascular or neurological compromise was present. No other abnormalities were identified.

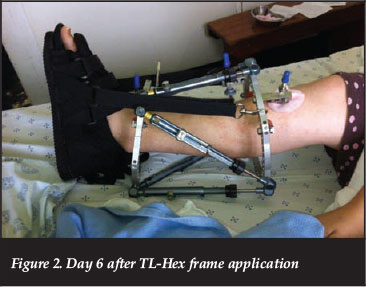
Surgical management consisted of a fibula osteotomy followed by application of a TL-Hex circular external fixator. Proximal and distal fixation consisted of two hydroxyapatite-coated half pins and one 1.8 mm tensioned transverse wire secured to a single ring for each bone segment (Figure 2). The non-union site was left undisturbed and in the deformed position. No bone graft was added.
After a latency period of seven days, gradual correction was achieved over 23 days at a distraction rate of 1 mm per day. During the correction and the consolidation phase functional rehabilitation was encouraged with the assistance of a physiotherapist. Full weight bearing was allowed from the first post-operative day. Pin tract care followed our standard protocol and included twice daily cleaning with an alcoholic solution of chlorhexidine.16,17
No complications were encountered during the treatment period, and no pin site infections developed. After 22 weeks, radiographic evaluation confirmed solid union with exuberant callus formation. Union was confirmed by the lack of tenderness at the non-union site and the ability to weight bear on a fully dynamised external fixator without pain. After clinical and radiographic confirmation of union, the external fixator was removed (Figure 3). Radiographic follow-up confirmed a solid union with no displacement of deformity, ten months after fixator removal.

Discussion
Circular external fixators are increasingly being used for orthopaedic trauma and post-traumatic reconstruction.18-20 These fixators exhibit a unique ability to eliminate bending and translational shear while maintaining a degree of axial micromotion.19,21-25 This three-dimensional stability translates into a biomechanical environment that is conducive to bone healing and regenerate formation and is often exploited for limb salvage and reconstruction.18, 24, 26-28
The hexapod fixator has been a recent modification of the traditional Ilizarov-type fine wire circular external fixator.29-30 It consists of two rings connected with six oblique struts in an octahedral configuration. Complex mathematical algorithms calculate strut length adjustments in order to manipulate the orientations of the two rings to each other.31-32 By attaching each of these rings to a bone segment, their position and orientation can be altered, thereby facilitating the reduction of complex multiplanar deformities.
Partial fibula resection is an important step in the management of tibial non-unions:33 Not only does the fibula osteotomy increase compressive forces across the ununited tibia, correction of tibial deformities relies on a mobile fibula.33-37 For both these reasons a partial fibula resection was performed in our patient as it allowed correction of the tibial deformity and force transmission across the tibial non-union site.
The Orthofix TL-Hex is the latest hexapod circular external fixator that is commercially available. The first case was performed in South Africa on 12 November 2012 and since then its use has steadily increased in South Africa, Great Britain, France and Italy. The key design features of the TL-Hex include struts with both acute and gradual excursions that increase their working lengths (Figure 4), struts that attach via stable ball joints on the outside of rings to open more fixation holes in the rings (Figure 5), and the adjustment of struts through a user-friendly click mechanism that prevents accidental adjustments.


In stiff non-unions, the ability of the hexapod circular external fixator to provide controlled gradual distraction allows not only the correction of existing deformities, but also the stimulation of new bone formation. This 'tension-stress effect' was initially described by Ilizarov and is the biological basis of distraction histogenesis used in limb lengthening and bone transport.38-40 It is thus possible, in low biologically active scenarios, to stimulate natural bone healing without the addition of bone graft or orthobiologics. This was demonstrated in our case, where an oligotrophic non-union healed with exuberant callus formation through gradual distraction without the addition of bone graft.
Conclusion
Circular external fixators are extremely useful in the management of tibial non-unions. Hexapod fixators in particular provide additional management options where non-unions are associated with deformities that are not acutely correctable.
The TL-Hex fixator is the latest hexapod circular external fixator that is commercially available, and this case is the first report of its use in clinical practice. Its use allowed gradual reduction of a stiff non-union while also facilitating functional rehabilitation and eventual union in an acceptable position.
Consent
Written consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The content of this article is the sole work of the author. No benefits of any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1. Fong K, Truong V, Foote CJ, Petrisor B, Williams D, Ristevski B, et al. Predictors of nonunion and reoperation in patients with fractures of the tibia: an observational study. BMC Musculoskelet Disord. 2013;14:103. PubMed PMID: 23517574. Pubmed Central PMCID: 3614478. [ Links ]
2. Akhtar A, Shami A, Sarfraz M. Functional outcome of tibial nonunion treatment by Ilizarov fixator. Ann Pak Inst Med Sci. 2012;8(3):188-91. [ Links ]
3. Bhandari M, Schemitsch E. Clinical advances in the treatment of fracture nonunion: the response to mechanical stimulation. Curr Opin Orthop. 2000;11:372-77. [ Links ]
4. Wu CC, Chen WJ. A revised protocol for more clearly classifying a nonunion. J Orthop Surg. 2000;8(1):45-52. PubMed PMID: 12468875. [ Links ]
5. Dimitriou R, Kanakaris N, Soucacos PN, Giannoudis PV. Genetic predisposition to non-union: evidence today. Injury. 2013;44 Suppl 1:S50-53. PubMed PMID: 23351872. [ Links ]
6. Douglas L, Benson D, Seligson D. The incidence of nonunion after nailing of distal tibial and femoral fractures. Curr Orthop Pract. 2010;21(1):49-53. [ Links ]
7. Harwood P, Newman J, Michael ALR. An update on fracture healing and non-union. Orthop Trauma. 2010;24(1):9-23. [ Links ]
8. Jones CB, Mayo KA. Nonunion treatment: iliac crest bone graft techniques. J Orthop Trauma. 2005;19(10 Suppl):S11-3. PubMed PMID: 16479216. [ Links ]
9. Perumal V, Roberts C. (ii) Factors contributing to non-union of fractures. Curr Orthop. 2007;21(4):258-61. [ Links ]
10. Sun D, Yuan D, Zhang X. A new hypothesis on the mechanism of atrophic non-union. Medical Hypotheses. 2011;77(1):69-70. [ Links ]
11. Abumunaser LA, Al-Sayyad MJ. Evaluation of the calori et Al nonunion scoring system in a retrospective case series. Orthopedics. 2011;34(5):359. PubMed PMID: 21598896. [ Links ]
12. Buijze GA, Richardson S, Jupiter JB. Successful reconstruction for complex malunions and nonunions of the tibia and femur. J Bone Joint Surg [Am]. 2011;93(5):485-92. PubMed PMID: 21368081.
13. Kanellopoulos AD, Soucacos PN. Management of nonunion with distraction osteogenesis. Injury. 2006;37 Suppl 1:S51-5. PubMed PMID: 16574120. [ Links ]
14. Antonova E, Kim Le T, Burge R, Mershon J. Tibia shaft fracture - costly burden of nonunions.pdf. BMC Musculoskeletal Disord. 2013;14:42. [ Links ]
15. Tzioupis C, Giannoudis PV. Prevalence of long-bone non-unions. Injury. 2007;38 Suppl 2:S3-9. PubMed PMID: 17920415. [ Links ]
16. Ferreira N, Marais LC. Prevention and management of external fixator pin track sepsis. Strat Traum Limb Recon. 2012;7(2):67-72. PubMed PMID: 22729940. Pubmed Central PMCID: 3535127. [ Links ]
17. Ferreira N, Marais LC. Pin tract sepsis: Incidence with the use of circular fixators in a limb reconstruction unit. SA Orthop J 2012;11(1):10-18. [ Links ]
18. Fragomen AT, Rozbruch SR. The mechanics of external fixation. HSS journal: the musculoskeletal journal of Hospital for Special Surgery. 2007;3(1):13-29. PubMed PMID: 18751766. Pubmed Central PMCID: 2504087. [ Links ]
19. Mullins MM, Davidson AW, Goodier D, Barry M. The biomechanics of wire fixation in the Ilizarov system. Injury. 2003;34(2):155-7. PubMed PMID: 12565025. [ Links ]
20. Moss DP, Tejwani NC. Biomechanics of external fixation: a review of the literature. Bulletin of the NYU hospital for joint diseases. 2007;65(4):294-99. PubMed PMID: 18081548. [ Links ]
21. Paley D, editor. Biomechanics of the Ilizarov external fixator. 1991. [ Links ]
22. Paley D, Fleming B, Catagni M, Kristiansen T, Pope M. Mechanical evaluation of external fixators used in limb lengthening. Clin Orthop Relat Res. 1990;250:50-57. PubMed PMID: 2293944. [ Links ]
23. Yamagishi M, Yoshimura Y. The biomechanics of fracture healing. J Bone Joint Surg [Am]. 1955;37-A(5):1035-68. PubMed PMID: 13263349.
24. Bronson DG, Samchukov ML, Birch JG, Browne RH, Ashman RB. Stability of external circular fixation: a multi-variable biomechanical analysis. Clin Biomech. 1998;13(6):441-48. PubMed PMID: 11415819. [ Links ]
25. Hasenboehler E, Smith WR, Laudicina L, Philips GC, Stahel PF, Morgan SJ. Fatigue behavior of Ilizarov frame versus tibial interlocking nail in a comminuted tibial fracture model: a biomechanical study. J Orthop Surg Res. 2006;1:16. PubMed PMID: 17156471. Pubmed Central PMCID: 1702341. [ Links ]
26. Watson MA, Mathias KJ, Maffulli N. External ring fixators: an overview. Proceedings of the Institution of Mechanical Engineers Part H. J Eng Med. 2000;214(5):459-70. PubMed PMID: 11109853. [ Links ]
27. Hak DJ, Toker S, Yi C, Toreson J. The influence of fracture fixation biomechanics on fracture healing. Orthopedics. 2010;33(10):752-55. PubMed PMID: 20954622. [ Links ]
28. Mitousoudis A, Magnissalis E, Kourkoulis S. A biomechanical analysis of the Ilizarov external fixator. EPJ Web of Conferences. 2010;6 DOI: http://dx.doi.org/10.1051/epjconf/20100621002 [ Links ]
29. Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 2005;29(2):125-29. PubMed PMID: 15703937. Pubmed Central PMCID: 3474509. [ Links ]
30. Taylor J. Correction of general deformity with the Taylor Spatial Frame. http://www.jcharlestaylor.com 2002. [ Links ]
31. Gao XS, Lei D, Liao Q, Zhang GF. Generalized Stewart-Gough platforms and their direct kinematics. IEEE Transaction. 2005;21(2):141-51. [ Links ]
32. Husty ML. An algorithm for solving the direct kinematics of general Stewart-Gough platforms. Mech Mach Theory. 1996;31(4):365-79. [ Links ]
33. Rozbruch SR, Fragomen AT, Ilizarov S. Correction of tibial deformity wth use of the Ilizarov-Taylor spatial frame. J Bone Joint Surg [Am]. 2006;88-A Suppl 4:156-74.
34. Fernandez-Palazzi F. Fibular resection in delayed union of tibial fractures. Acta Orthop Scand. 1969;40:105-18. [ Links ]
35. Rankin EA, Metz CW. Management of delayed union in early weight bearing treatment of fractures tibia. J Trauma. 1970;10:751-59. [ Links ]
36. Jorgensen TE. The influence of the intact fibula on the compression of a tibial fracture or pseudoarthrosis. Acta Orthop Scand. 1974;45(1):119-29. PubMed PMID: 4451045. [ Links ]
37. Dujardyn D, Lammens J. Treatment of delayed union or non-union of the tibial shaft with partial fibulectomy and an Ilizarov frame. Acta Orhtop Belg. 2007;73:630-34. [ Links ]
38. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263-85. PubMed PMID: 2912628. [ Links ]
39. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249-81. PubMed PMID: 2910611. [ Links ]
40. Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8-26. PubMed PMID: 2403497. [ Links ]
 Correspondence:
Correspondence:
Dr N Ferreira Tumour
Sepsis and Reconstruction Unit Department of Orthopaedic Surgery Grey's Hospital Nelson R Mandela School of Medicine
UKZN Pietermaritzburg, South Africa
Tel: +27 33 897 3000
Email: Nando.Ferreira@kznhealth.gov.za














