Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.13 n.4 Centurion Dec. 2014
Expert Opinion on Published Articles
Reviewer: Dr N Ferreira
Tumour, Sepsis and Reconstruction Unit, Department of Orthopaedic Surgery, University of KwaZulu-Natal Grey's. Hospital Pietermaritzburg, Tel: +27 033 897 3299. Nando.Ferreira@kznhealth.gov.za
What are the functional outcomes of endoprosthetic reconstructions after tumor resection?
NM Bernthal, M Greenberg, K Heberer, JJ Eckart Clin Orthop Relat Res 2014;DOI 10.1007/s11999-014-3655-1
The diagnosis of a primary bone sarcoma has historically meant extremely poor survival, and surgical procedures limited to amputations. With advances in medical and surgical treatment of these cancers, patient survival has improved tremendously. This increased life expectancy has resulted in a higher demand for limb salvage. It should however still be emphasised that the primary aim in tumour surgery is to save a life, secondarily to save a limb and lastly to restore function beyond routine daily living activities.
Where limb salvage can be performed without jeopardising patient survival, it is imperative to discuss expected outcomes with patients and their families.

Objective data regarding implant longevity and functional results can assist the orthopaedic oncological surgeon in generating reasonable expectations of life after limb salvage and provide the patient with a realistic look into the future.
Bernthal et al. invited 69 eligible patients to participate in a study evaluating the functional outcome of endoprosthetic reconstructions after tumour resections. The authors aimed to answer three questions: 1) What is the efficiency of gait? 2) What is the knee strength compared to the contralateral side? And 3) How active are patients at home and in the community?
Twenty-four patients (seven proximal femur, nine distal femur and eight proximal tibia replacements) at a mean of 13.2 years (2.5-28.2) from endoprosthetic reconstruction responded to the invitations. All respondents underwent evaluation in a gait laboratory to ascertain O2 cost of walking and walking speed. Isokinetic strength testing of knee extension and flexion was measured and all patients were asked to wear a StepWatch Activity Monitor to measure their total number of strides per day. The results were compared with a control group of eight healthy individuals.
There was no statistical difference for median 02 cost during gait between any of the groups (proximal femur, distal femur and proximal tibia replacements) and controls. Median walking speed between the groups and control also showed no statistical significant difference. All reconstructions showed decreased strength in knee extension and flexion compared to the contralateral side with the proximal tibial reconstruction group showing the greatest deficit. There was no statistical significant difference in the number of steps taken at home or in the community among the different reconstruction groups.
The current study reports excellent functional results over long follow-up times
Objective functional outcomes after tumour resection and endoprosthesis reconstruction are necessary to generate reasonable expectations for surgeons and patients undergoing limb salvage. The current study reports excellent functional results over long follow-up times. It is however important to note that only about a third of the eligible patients responded to the invitation for functional evaluation. This obviously has the potential for a significant observational bias, as patients with poorer outcomes might not be willing to participate in the physical activities required for the evaluation. I would caution against generating expectations of functional outcomes reported in this paper with all patients about to undergo tumour resection and megaprosthesis reconstruction.
This study does, however, propose good objective measures to evaluate functional outcomes after tumour resection and endoprosthetic reconstruction. These measures can potentially be used to objectively evaluate different surgical reconstruction techniques and implant designs in future.
Reviewer: Dr LC Marais
Tumour, Sepsis and Reconstruction Unit
Department of Orthopaedic Surgery
University of KwaZulu-Natal
Grey's Hospital Pietermaritzburg
Tel: (033) 897 3424
Leonard.Marais@kznhealth.gov.za
'Warning signs' of primary immunodeficiency among patients with periprosthetic joint infection
Claudio Diaz-Ledezma, Jennifer Baker, Javad Parvizi
J Appl Biomater Funct Mater 2014;12(2):65-69.
DOI: 10.5301/jabfm.5000207
Periprosthetic joint infection (PJI) is a devastating complication following hip and knee arthroplasty. The role of the host in the development of PJI is well recognised and several scoring systems have been devised in an attempt to identify high-risk patients. These scoring systems have, however, focused on factors known to be associated with secondary immunodeficiency. In this article the authors investigate the potential role of primary immunodeficiency (PID) in the development of PJI.
Primary immunodeficiency encompasses a wide spectrum of genetic disorders which result in a reduction in the competency of a patient's immune response, placing them at risk of multiple infections. More than 180 such disorders have been identified and it is estimated that 1 in 1 200 people in the United States may be afflicted with PID. These disorders have been classified into eight broad categories consisting of combined immunodeficiencies, antibody deficiencies, immune dysregulation, phagocyte abnormalities, innate immunity dysfunction, autoinflammatory disorders and complement deficiencies. One of the more common disorders presenting in adulthood is common variable immunodeficiency (CVID), which is characterised by varying degrees of hypogammaglobulinaemia.

Clinically these disorders may be difficult to detect, and researchers have developed a list of ten 'warning signs' which may point towards the possible presence of a PID. These warning signs consist of the following:
1. Two or more new ear infections within one year
2. Two or more new sinus infections within one year, in the absence of allergy
3. One pneumonia per year for more than one year
4. Chronic diarrhoea with weight loss
5. Recurrent viral infections (colds, herpes, warts, condyloma)
6. Recurrent need for intravenous antibiotics to clear infections
7. Recurrent, deep abscesses of the skin or internal organs
8. Persistent thrush or fungal infections on skin or elsewhere
9. Infection with normally harmless tuberculosis-like bacteria
10. A family history of primary immunodeficiency
In the study by Diaz-Ledezma et al., 14% of the 185 patients with PJI included in the study had one or more of these 'warning signs'. Only a small number of cases, though, had no additional comorbidities (which could have caused a secondary immunodeficiency). The potential prevalence of PID was therefore estimated to be in the region of 1.6%. The limitations of this study were, however, acknowledged by the authors. Only patients with more than 15 medical consults at the institution's facilities, prior to the diagnosis of PJI, were included in the study. This means that 587 patients on their PJI database were excluded and the sample size was considerably reduced. The second limitation is the retrospective nature of the analysis. The prevalence can only be inferred, as routine testing for PID was not performed. The final shortcoming relates to the ten 'warning signs' themselves. These have been criticised in several other publications because of their lack in accuracy.
While the article under scrutiny does not necessarily provide the answers, it raises important questions. What percentage of patients with implant-related infections has an underlying primary immunodeficiency? A well-designed prospective study will be required to answer this question. Common variable immunodeficiency, for example, can be treated through immunoglobulin replacement therapy. Should we, therefore, be screening patients for the presence of a PID prior to elective arthroplasty? The authors of this study concluded that administration of these 'warning sign' questions to patients with multiple infections may lead to identification of a primary immunodeficiency status which may in turn influence the outcome of elective arthroplasty. In my limited experience, the management of patients with PID has been particularly challenging and requires a multidisciplinary approach. It may, therefore, be advisable to screen patients with an unexplainable infection for the presence of an underlying immunodeficiency.
Reviewer: Dr P Greyling
Department of Orthopaedic Surgery
Steve Biko Academic Hospital
Tel: 012 354 2851
Management after failed treatment of ankle fracture
John A Scolaro, David P Zamorano
Current Orthopaedic Practice 2014;25(3):221-26
Failed treatment of ankle fractures can result in ankle instability and joint surface incongruity. Biomechanical studies have shown that lateral talar shift of more than 1 mm causes a loss of over 40% of the tibiotalar contact area. This leads to pain, loss of function and early post-traumatic degenerative changes.
The aim of treatment should be to identify the reason for failure, and anatomically reduce and restore the tibiotalar joint with stable fixation.
The ideal time for reconstruction is not known; the literature supports a few months to years.
Evaluation should include a complete clinical and radiological evaluation. The radiological investigation includes X-rays (three views), anteroposterior, mortis (200 internal rotation) and a lateral view. A CT scan can be helpful to evaluate the syndesmosis, fracture reduction, bony fragments, debris and articular surface.
Lateral malleolus
Restore fibular length and rotation. Visualisation of the distal tibiofibular joint is essential to ensure correct reduction of the lateral malleolus within the incisura of the distal tibia.
Transverse, step and oblique fibular osteotomies have been described to restore length and rotation. If the osteotomy exceeds 3 mm, autologous bone graft should be used.
Medial malleolus
Osteotomy or debridement of non-healing bone surfaces.
The anterior medial edge of the tibial plafond should be exposed to ensure chondral reduction of the medial malleolus. Fixation can be done with screws, tension band construct or a plate fixation. Fragment excision can be performed if the fragment removal does not result in ankle instability. The deltoid ligament can be advanced and secured to bone with anchors or bone tunnels.
Posterior malleolus
Isolated malunion or non-union of the posterior malleolus is rare. If posterolateral subluxation of the talus occurs, a corrective osteotomy and revision fixation should be done.
Syndesmosis
Revision fixation should be performed with an open technique. Visualise the distal tibiofibular joint and debride the incisura.
Conclusion
Ankle fractures are commonly treated orthopaedic injuries; the goal should be to achieve a well-aligned stable ankle joint.
This article summarises the treatment options for the failed treatment of ankle fractures, and is a good read for all registrars.
The aim of treatment should be to identify the reason for failure, and anatomically reduce and restore the tibiotalar joint with stable fixation

Reviewer: Dr FF Birkholtz
Unitas Hospital
Lifestyle Management Park Suite 8C
Lyttleton
012 644-2641
Prevention and management of external fixator pin track sepsis
N Ferreira, LC Marais
Strategies in Trauma and Limb Reconstruction 2012;7:67-72
The effect of HIV infection on the incidence and severity of circular external fixator pin track sepsis: a retrospective comparative study of 229 patients
N Ferreira, LC Marais
Strategies in Trauma and Limb Reconstruction 2014;9:111-15
External fixation is increasingly used for the treatment of complex trauma, trauma sequelae and congenital conditions. The weak point of any external fixator is the pin-bone interface, as this is where the fixation of the external fixator to the bone takes place. Compromise of this interface through pin track infection can lead to catastrophic failure of the external fixator device.
In these two excellent articles from two prominent local limb reconstruction surgeons, they first discuss a scientific approach to pin track care, followed by a critical look at HIV as a risk factor for pin track sepsis.
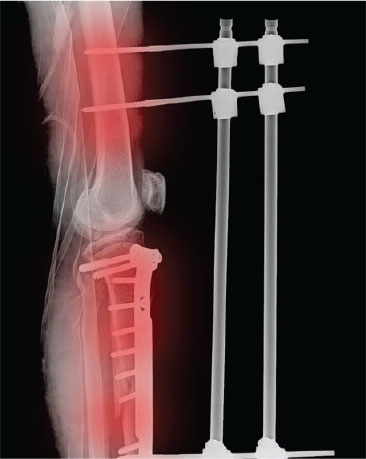
In the first article, the principles of proper pin track care are systematically and clearly discussed with good reference to the available literature. An important message is that pin track care commences during the intra-operative phase, as proper pin and wire insertion are essential in preventing later pin track problems.
The authors then guide the reader through a scientific postoperative pin track protocol through the early and late postoperative periods. They also discuss the management of pin track problems after frame removal. Treatment of established pin track sepsis is also discussed in some detail.
This article is a seminal work in the field of external fixator surgery and makes essential reading for anyone who uses external fixation, even occasionally.
The second article explores whether HIV should be seen as a significant risk factor for pin track infection. This article represents the biggest single study where pin track sepsis rates were evaluated and compared between HIV positive and negative patients. It also seems to be the only one focusing on circular external fixation.
A meticulous retrospective analysis of a single centre's results was performed and all the patients were treated with a strict pin care protocol. It was shown clearly that HIV positivity and indeed CD4 count showed no correlation to the presence or severity of pin track sepsis.
This means that the dogma that circular fixation is not appropriate for HIV-positive patients is refuted. In this regard, this paper will become one of the benchmark papers in the field of external fixation.
These two papers, read together, illustrate the importance of meticulous pin track care, which can give excellent results despite factors like immunocompromise. Acceptably low infection rates can be achieved, thereby making external fixation a more attractive option in the treatment of complex orthopaedic pathology.














