Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.13 n.3 Centurion Sep. 2014
SPINE
Effect of additional ultrasound therapy to analgesics in treatment of acute low back pain: A randomised control trial conducted at the Aga Khan University Hospital, Nairobi (AKUH, N)
S MohammedaliI; SK MutisoII; P OrokoI; B OmbachiI; H SaidiI
IMBChB, MMed(Surg); Department of Surgery, Aga Khan University Hospital, Nairobi, Kenya
IIBSc MBChB; Medical Officer at the Tigoni Hospital, Limuru, Kenya; Department of Human Anatomy, University of Nairobi, Kenya
IMBChB, MMed(Surg), FRCS(Ed), FRCS(Tr&Orth); Department of Surgery, Aga Khan University Hospital, Nairobi, Kenya
IMBChB, MMed, AO Spine Fellow; Department of Surgery, Aga Khan University Hospital, Nairobi, Kenya
IBSc, MBChB, MMed(Surg), FCS(ECSA), FACS; Department of Surgery, Aga Khan University Hospital, Nairobi, Kenya
ABSTRACT
BACKGROUND: Acute low back pain (LBP) is a common condition that is encountered by many physicians with varied treatments instituted in its management. Ultrasound physiotherapy is a common modality used in its management, although its effectiveness and its role in management of acute LBP is not well known.
METHODS: A randomised controlled trial was conducted to compare the effect of the addition of ultrasound therapy to a defined analgesia protocol in patients presenting with acute LBP at the Aga Khan University Hospital, Nairobi. The main outcomes were reduction in disability and pain which were evaluated using the mean change in Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) score for pain, respectively. Patients were followed up for a minimum of four weeks with assessment using the ODI and VAS at weekly clinic visits.
RESULTS: Seventy-four patients were included in the study. Thirty-six patients were allocated to the analgesia with additional ultrasound group and 38 to the analgesia alone group. The Minimal Clinically Important Difference (MCID) of 10% points at four weeks after initiation of treatment was achieved in the ultrasound group but not in the analgesia only group. This difference was not statistically significant though, 10.35% vs 8.44%; p=0.36. There was no difference in the mean change in the ODI score between the two groups at any of the four follow-up visits after initiation of treatment. Mean difference in change of ODI (95% confidence interval) was -3.2(-7.0 to 0.6) after the first week, 2.96(-1.3 to 7.2) after the second and 1.90(-2.3 to 6.1) after the third week, p=0.36, 0.17 and 0.096 respectively. There was also no difference detected in the mean change of VAS score between the two groups at the first and fourth visit. Mean difference in VAS between the first and fourth weeks was 0.2 with a 95% confidence of -0.85 to 1.2 (p=0.72).
CONCLUSION: The addition of ultrasound therapy to the treatment of acute LBP improved patient outcomes as assessed by an MCID of a disability index, but which was not statistically significant. No outcome difference was noted in the two groups using the VAS pain score.
Keywords: acute low back pain, analgesia, ultrasound therapy.
Introduction
Low back pain (LBP) is a common condition worldwide with associated significant disability and economic implications.1,2 The lifetime prevalence of LBP is over 70% in industrialised countries with peak prevalence occurring between ages 35 and 55 years.3 It is the second most common reason for absence from work in adults aged <55 years, with work-related LBP estimated to cause 818 000 disability-adjusted life years lost annually.4,5 In African countries, a lifetime prevalence of 62% among adults has been reported and this was associated with significant disability, loss of productivity and working man hours.6
Most patients with LBP have no serious pathologic aetiology, with most having their LBP attributed to an unidentified cause, either due to mechanical strain or related to work/posture.7-9 The natural history of acute LBP is resolution of symptoms in the majority of patients by the fourth week of onset with 90% returning to work within three months.10-12
With minimal intervention such as analgesia and minimising activity to tolerable levels only, most patients improve in the first few weeks.13,14 Analgesic therapy alone without additional treatment has been shown to be effective in terms of pain control and reduction of disability.15 The use of paracetamol, ibuprofen and mefenamic acid has been recommended, with opiates and muscle relaxants being disapproved due to their sedative effects, drug dependence and lack of additional benefit.12-16-17 Interventions such as physiotherapy, bed rest and back exercises that are frequently used in clinical practice, have no strong evidence to support their routine use.12,14 Moreover, massage and transcutaneous electrical nerve stimulation (TENS) therapy are not recommended as modalities of therapy because of a lack of proven clinical benefit.12 Ultrasound waves are often used as an adjunct to medical therapy for their thermal effect.18,19 However, although its use is expensive to the patient there is no proven clear benefit in the management of acute LBP.20,22 There is no published randomised trial to assess this. The present study aimed to assess the effectiveness of ultrasound in addition to analgesia as compared to analgesia alone as interventions to reduce the morbidity of LBP with regard to pain control and disability.
Methods
Trial design
The study was a randomised, controlled trial of patients with acute LBP comparing an intervention group, who received the standard analgesia protocol and ultrasound therapy, with a control group, who received only the standard analgesia protocol (Figure 1).
Participants
Patients presenting with acute LBP, as defined in the inclusion and exclusion criteria, aged 18-60 years. The patients were all seen at the Aga Khan University Hospital, Nairobi (AKUH, N), Kenya.
The inclusion criteria constituted: Patients aged 18-60 years with acute onset LBP. An acute episode of pain was defined as pain that lasts for more than 24 hours but less than six weeks. Moreover, the pain had to be in an area bounded superiorly by T12 and inferiorly by the buttock crease.
The exclusion criteria constituted the following:
- Patients with indicators of serious pathology from history and examination findings, also referred to as 'red flags'.12 Patients with red flags were further investigated with imaging and referred for further management.
- Patients who were vomiting - we wished to administer the analgesic prescription by the oral route.
- Patients who were already on other forms of analgesia, e.g. opioids and muscle relaxants.
- Patients with contraindications to ultrasound treatment such as skin allergies, dermatitis or a skin haematoma, and those already on other forms of physiotherapy.
Interventions
Study protocol
A study guideline and unbiased randomisation was adhered to. This guideline was circulated and a copy for reference was available at all study recruitment sites. Informed consent was obtained by the treating physician after discussing the study with patients. Training was held for the doctors and physiotherapists who were involved in patient recruitment and to maximise protocol adherence. The ODI was given to the patients and was reported by patient self-response on study entry and at intervals of 1, 2 and 3 weeks after initiation of therapy. Following an initial visit, they were provided with a mobile phone contact for reporting non-improvement of their pain and instructions for escalation of pain management were given as per the protocol.
Treatment protocol
Control arm: Patients were commenced on 1 g of paracetamol by mouth stat, then 1 g 6 hourly for seven days. All patients were managed as outpatients unless they had severe pain, i.e. ODI score of 50% or more or a VAS score of more than 8/10; were not ambulatory due to pain; requested to be managed as an inpatient; fulfilled the three criteria above and could afford the admission fee or opted to go to another hospital.
Intervention arm: Patients were commenced on 1 g of paracetamol by mouth stat, then 6 hourly for seven days. Concurrent physiotherapy (ultrasound only) was commenced with the first session starting the same day of recruitment unless they presented after midnight, in which case it was commenced on the earliest available session. Pulsed ultrasound therapy was administered with a total of three sessions in a week for two weeks (a total of six sessions). All patients were managed as outpatients unless they met the criteria stated above.
With minimal intervention such as analgesia and minimising activity to tolerable levels only, most patients improve in the first few weeks
Follow-up: In both arms, patients managed on an in/ outpatient basis were reviewed at intervals of 1, 2, and 3 weeks with the ODI administered at every contact. If at subsequent review the reported pain was persistent or had increased, the treating physician was to add a non-steroidal anti-inflammatory drug, i.e. Ibuprofen 400 mg twice daily for seven days.17,21,23 All patients had access to a central help line number for enquiries or to report any problems during their management. Direct questioning about medication compliance was used to confirm patient compliance with the protocol.
Outcome
Oswestry Disability Index (ODI)
Outcomes were measured using a patient-administered questionnaire, the Oswestry Disability Index (ODI). The ODI is a validated and widely used tool for assessing disability from back pain. It is a ten-question, self-administered questionnaire that is convenient to use. It has been translated for use into various languages around the world, and has been shown to be indicative of the respondent's disability from LBP. We used the English version to assess disability from acute back pain in this study.23,24 The Minimal Clinically Important Difference (MCID) for the ODI in the present study was taken to be 10 percentage points.23
Sample size determination
Malimvaara and colleagues14 showed that at three weeks, the mean ODI index for patients who were randomised to exercise as compared to no treatment, was significantly different (mean difference=6.6) to that for patients on bed rest (mean difference=3.9). In the same study at 12 weeks, the mean ODI index was about 6 for all treatments. In a meta-analysis of acute LBP treatment, Machado and colleagues compared the analgesic effects of treatments for non-specific LBP using a 100-point scale and reported that analgesics had a moderately significant treatment effect (10-20 points) when compared to placebo, unlike exercise, radiotherapy, traction, physiotherapy or prolotherapy, which showed a minor treatment benefit (<10 points).24 The estimated pooled standard deviation (SD) of the ODI for the bed rest-control and exercise-control comparisons was 10.5 and 11.71 at three weeks, and 9.44 and 10.07 at 12 weeks, respectively.
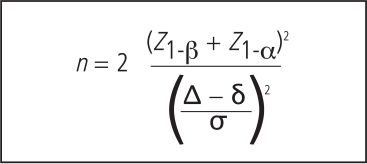
Using a level of significance of 5% and 80% power, the study needed 37 patients in each study arm assuming a clinically meaningful difference (δ) in the ODI index of 10, an observed difference (Δ) between the control and treatment arm of 3.5 and a standard deviation of 10.
The formula for calculating the sample size in the control and treatment group for a comparative study is given by:
Adjusting for 10% loss to follow-up then a total of 82 patients were to be recruited in the study.
Randomisation
The recruited patients were randomised by the choosing of sealed envelopes with written prescription for paracetamol alone (38 patients) and paracetamol with the ultrasound therapy regimen (36 patients). The envelopes were opened at the Accident and Emergency Department and pharmacy, and the doctor/pharmacist administered the prescription drug and directed the patient to the Physiotherapy Department depending on the treatment allocation. Recruited patients were randomised with each arm having the ODI administered, and treatment commenced immediately according to protocol.
Statistical methods
Each recruited patient's ODI was recorded in their file and retrieved after three weeks for analysis. The mean change in ODI and VAS score was calculated using the SPSS-version 17(SPSS Inc., Chicago, Illinois) and STATA-10 software for analysing the trends and assessing statistical difference between the groups.
Comparisons among the treatment groups was done using Wests for normally distributed continuous variables such as age of patients and mean change in scores, while the Mann-Whitney non-parametric test was used for non-normally distributed continuous outcomes, for example, the individual ODI scores of each patient.
Linear mixed-effect models were used for multivariate analysis to determine factors that may be associated with the rate of change of the ODI index over time.
The Oswestry Disability Index (ODI) is a validated and widely used tool for assessing disability from back pain
Ethical considerations
Ethical approval was obtained from the AKUH, N research committee ethics board. All information was confidential and used for the sole purpose of the study. In all participants, the following guidelines were observed: All patients received the current standard of care with regard to pain management, i.e. pain control according to the prior stated protocol. If for any reason their pain was not controlled according to the protocol, they were given opioid analgesia and excluded from the study with an 'intention to treat' analysis being performed. All adverse events were reported and recorded. Patients who reported severe adverse events related to the treatment or non-improvement in back pain were excluded, with the protocol being discontinued, reassessed and referred to the Orthopaedic clinic for further treatment.
Informed consent was obtained from all participants by the treating physician at the first contact. The patient was at liberty to withdraw from the study at any time he/she wished.
Results
A total of 108 patients were screened of which 14 patients declined participation and 94 patients were recruited. Of the recruited patients, 20 were excluded for the following reasons: ten patients had already been started on alternative analgesic agents that differed from our analgesic protocol and had used muscle relaxants; five had chronic back pain; and five patients had started other forms of physiotherapy.
Patient demographics
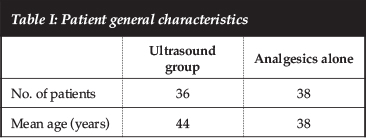
Seventy-four patients met the eligibility criteria and were randomised to receive analgesia with ultrasound (ultrasound group n=36), or analgesics alone (no-ultrasound group n=38). There were 39 (52.7%) male patients and 35 (47.3%) female patients. The participants had a mean age of 44 years in the ultrasound group and 38 years in the no-ultrasound group (Table I).
Primary outcome
Change in ODI score
The median ODI score was higher on the first visit in the ultrasound group but the rate and trend of ODI score change at any point over the four visits was not different from the final visit ODI score (Figure 2 and Table II). The score was 3 in the ultrasound group and 1 in the no-ultrasound group (P=0.23).
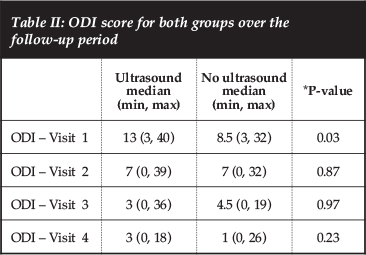
There was no difference in the mean change of the ODI score between the first and fourth, first and third and first and second visits. That is, none of the groups were improving faster on follow-up with regard to the change in ODI score over subsequent visits (Table III).
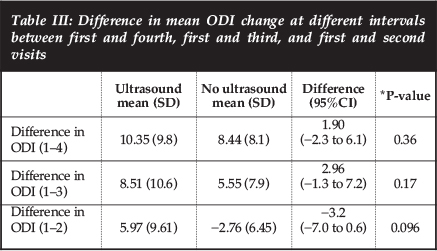
It is also important to note that the MCID (Minimal Clinically Important Difference) of 10 percentage points at four weeks after initiation of treatment was achieved in the ultrasound group but not in the analgesia-only group. This difference was however not statistically significant: 10.35% vs 8.44%; P=0.36 (Table III).
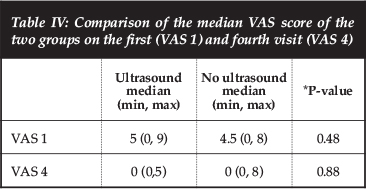
Change in Visual Analog Score (VAS)
Both groups had similar pain scores in terms of the VAS at the initial and final visits. There was no difference between the groups at the first and fourth visit; P=0.48 and P=0.8 respectively (Table IV). Also, no difference was detected in the mean change of the VAS over the first and fourth visits between the two groups (P=0.73).
Two of the 74 patients (one from each group) had persistent pain at the end of four weeks and went on to have a magnetic resonance imaging (MRI) assessment of the lumbo-sacral spine and orthopaedic referral. One patient had inter-vertebral disc extrusion of L4/5 that necessitated lumbar discectomy. The other had mild disc dehydration and disc bulge at L3/4 and L4/5 and is currently on follow-up for the same.
Discussion
LBP is of high prevalence worldwide with significant varied disability and economic implications.1,3 However, the efficacy of ultrasound therapy in addition to analgesia in its treatment is not well known. Consequently, the present study set out to determine the effect of additional ultrasound therapy to analgesia in the management of LBP.
At presentation, patients who were randomised to receive ultrasound had a higher ODI score but went on to improve in a similar manner as the no-ultrasound group by the fourth visit. Two of the 74 patients (one from each group) had persistent pain at the end of four weeks and went on to have an MRI assessment of the lumbo-sacral spine and orthopaedic referral. None of the patients had plain radiographs performed. This was in keeping with recommendations from other published literature as this practice has not been shown to add any value in the diagnosis or management of patients with acute LBP.25,26
Most of the patients improved by the fourth week of treatment in both arms, as expected in the natural course of acute LBP.3,27
For analysis, the individual median ODI score was used as the measure of central tendency as opposed to the means because the data was distributed in a non-parametric fashion, whereas the changes in the scores over time were normally distributed; therefore the difference in the mean change of the ODI score was analysed for significance. No statistically significant difference was observed to provide benefit with the addition of ultrasound in terms of ODI or VAS score change. One must take note that the MICD at 90% confidence is 10 percentage points. That means at least a 10% change is required to be clinically meaningful and a change of less than this may be attributable to an error in the measurement.23 In our study the MICD for the ODI at four weeks after initiation of treatment was achieved in the ultrasound group but not in the analgesia only group. This difference, however, was not statistically significant. This creates grounds for further investigating the clinical effectiveness of analgesia alone in the treatment of LBP when evaluated with the ODI.
Acute LBP can result from a variety of sites also known as 'pain generators' such as the facet joint, fascia, sacroiliac joint and inter-vertebral disc.28,29 The episodes of acute pain are usually self-limiting but cause significant absenteeism from work, affect productivity and loss of man hours.30 The rationale for additional therapeutic modalities for back pain should be guided by evidence of improvement in this disability. The most commonly used dosage of ultrasound was employed in this study.20 Ultrasound waves used at this frequency achieve tissue penetration transdermally and are postulated to confer analgesic effect by improving the elasticity of collagencontaining tissues.21 Apart from the 'thermal theory' of the mechanism of action of ultrasound,20,21 it is also thought that ultrasound promotes healing by increasing blood supply, hence increasing oxygen delivery, nutrients and white blood cells at the site of application.31,32 Almost immediately after injury to tissues, mast cells release histamine into the bloodstream, causing localised arteriolar vasodilatation and a consequential increase in blood flow.33,34
Dyson and Hasson and colleagues suggest that, if damaged tissues are exposed to ultrasound during the inflammatory phase of the healing process, blood flow may further increase. Whether this is attributable to a rise in temperature or to the release of histamine via non-thermal mechanisms remains unclear.35,36
We can therefore conclude that the use of additional ultrasound treatment resulted in a clinical difference in the disability index but did not statistically reduce pain or disability as compared to analgesia alone. Most of our patients had back pain that was adequately managed with analgesic therapy alone although this was not clinically detectable as per the ODI. We therefore recommend the use of paracetamol alone as first line therapy and adding an NSAID for those whose pain persists, with appropriate follow-up for gastritis when indicated. Since the use of additional physiotherapy in the form of single modalities or multimodal therapy is quite common, a study to address the effects of other therapies with a standard analgesic protocol and/or ultrasound therapy is indicated.
We can conclude that the use of additional ultrasound treatment resulted in a clinical difference in the disability index but did not statistically reduce pain or disability as compared to analgesia alone
Also, as the evidence for use of combination analgesics with muscle relaxants is weak and there are no clear guidelines for their use, future research is needed to investigate their usefulness in reducing pain and disability in this patient population.
Limitations
The present study had a couple of limitations: First, absence from work or loss of man hours were not recorded because of the concern for validity due to recall basis as this data could only be collected after the fourth visit on completion of therapy. Secondly, due to limited funds available our desire to have a sham therapy arm, i.e. allocation of patients to receive analgesics with the ultrasound probe being applied on the back but no delivery of the waves could not be executed.
References
1. Mounce K. Back pain. Rheumatology (Oxford). 2002;41:1-5. [ Links ]
2. Maetzel A, Li L. The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Practice & Research Clinical Rheumatology, Jan 2002;16(1):23-30. [ Links ]
3. Andersson GBJ. The epidemiology of spinal disorders. In: Frymoyer JW, ed. The adult spine: principles and practice. 2nd ed. New York: Raven Press, 1997;93-141. [ Links ]
4. Hadler NM. Workers with disabling back pain. N Engl J Med 1997;337:341-43. [ Links ]
5. Punette M, et al. Estimating the global burden of low back pain attributable to combined occupational exposures. Am J of Ind Med 2005;48:459-69. [ Links ]
6. Louw QA, et al. The prevalence of low back pain in Africa. BMC Musculoskeletal Disord. 2007;8:105. [ Links ]
7. Croft PR, Papageorgiou AC, Ferry S, et al. Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine 1995;20(24):2731-37. [ Links ]
8. Katz JN, et al. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. Bone Joint Surg Am. 2006;88 Suppl 2:21-24. [ Links ]
9. Macfarlane GJ, Thomas E, Papageorgiou AC, Croft PR, Jayson MI, Silman AJ. Employment and physical work activities as predictors of future low back pain. Spine 1997;22(10):1143-45. [ Links ]
10. Croft PR, et al. Outcome of low back pain in general practice: a prospective study. BMJ 1998;316:1356-57. [ Links ]
11. Roland M, et al. Spine (Phila Pa 1976). 1983;8(2):145-50. [ Links ]
12. van Tulder M, et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15 (Suppl. 2):S169-S191. [ Links ]
13. Andersson GB, Svensson HO, Oden A. The intensity of work recovery in low back pain. Spine 1983;8:880-84. [ Links ]
14. Malimvaara A, et al. The treatment of acute low back pain -Bed rest, exercise or ordinary activity? N Engl J Med 1995;332:351-55. [ Links ]
15. Koes BW, Scholten RJPM, Mens JMA, Bouter LM. Efficacy of non-steroidal anti-inflammatory drugs for low back pain: a systematic review of randomised clinical trials. Ann Rheum Dis 1997;56:214-23. [ Links ]
16. Van Tulder M, et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15 (Suppl. 2):S169-S191; recommendation T5. [ Links ]
17. Roelofs PD, Deyo RA, Koes BW, Scholten RJ, van Tulder MW. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database of Systematic Reviews 2008; Issue 1. Art. No.:CD000396. [ Links ]
18. Philadelphia Panel. Philadelphia Panel evidence-based clinical practice guidelines on selected interventions for low back pain. PhysTher 2001;81(10):1641-74. [ Links ]
19. Maher CG, et al. Effective physical treatment for chronic low back pain. Orthop Clin N Am 2004;35:57-64. [ Links ]
20. Coakley, S. Biophysical effects of ultrasound at therapeutic intensities. Physiotherapy 1978;64(4):169. [ Links ]
21. Dyson, M. Sucking Stimulation of tissue repair by ultrasound. Physiotherapy 1978:64(4):105. [ Links ]
22. University of Manchester. Backache beaten by good vibrations? Science Daily, 3 November 2006. http://www.sciencedaily.com. [Last accessed 10th January 2010]. [ Links ]
23. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000;25(22):2940-52. [ Links ]
24. The Italian version of the Oswestry Disability Index. Spine (Phila Pa 1976). 2009;34(19):2090-95. [ Links ]
25. van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine (Phila Pa 1976). 1997;22(4):427-34. [ Links ]
26. van den Bosch MAAJ, Hollingworth W, Kinmonth AL, Dixon AK. Evidence against the use of lumbar spineradiography for low back pain. Clinical Radiology 2004;59:69-76. [ Links ]
27. Pengel LHM, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis BMJ 2003;327:323-25. [ Links ]
28. Carragee EJ, Barcohana B, Alamin T, van den Haak E. Prospective controlled study of the development of lower back pain in previously asymptomatic subjects undergoing experimental discography. Spine 2004;29(10):1112-17. [ Links ]
29. Rives PA, Douglass AB. Evaluation and treatment of low back pain in family practice. J Am Board Fam Pract 2004;17:S23-31. [ Links ]
30. National Institute of Neurological Disorders and Stroke (NINDS). Low Back Pain Fact Sheet. Bethesda, MD: National Institute of Neurological Disorders and Stroke; 2003. [ Links ]
31. Baker RJ, Bell GW. The effect of therapeutic modalities on blood flow in the human calf. J Orthopaedic and Sports Physical Therapy 1991;13:23-27. [ Links ]
32. Houghton PE. Effects of therapeutic modalities on wound healing: A conservative approach to the management of chronic wounds. Physical Therapy Reviews 1999;4:167-82. [ Links ]
33. Maxwell L. Therapeutic US: Its effects on the cellular and molecular mechanisms of inflammation and repair. Physiotherapy 1992;78:421-26. [ Links ]
34. Sherwood L. Human physiology: From cells to systems 4th ed. New York: Brooks/Cole Publishing, 2001. [ Links ]
35. Dyson M. Mechanisms involved in therapeutic US. Physiotherapy 1987;73:116-20. [ Links ]
36. Hasson S, Mundorf R, Barnes W, Williams J, Fujii M. Effect of pulsed US versus placebo on muscle soreness perception and muscular performance. Scand J Rehabilitation Medicine 1990;22:199-205. [ Links ])
 Correspondence:
Correspondence:
Dr S Mohammedali
Department of Surgery
Aga Khan University Hospital
Nairobi, Kenya
PO Box 030270-00100
Nairobi, Kenya
Tel: +254711092115
Fax: +254203743935
Email: shamshuza@yahoo.com
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.














