Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.13 no.3 Centurion sep. 2014
SHOULDER AND ELBOW
Early and medium-term complications of the modified Latarjet procedure
J-P du PlessisI; A LambrechtsII; D McGuireIII; SJL RocheIV; BC VrettosV
IFCS(SA)Orth, MMed(Orth)UCT; Consultant Orthopaedic Surgeon, New Somerset Hospital, Cape Town
IIMMed(Orth)Pret; Consultant Orthopaedic Surgeon Constantiaberg Hospital, Cape Town
IIIFCS(SA)Orth, MMed(Orth)UCT; Consultant Orthopaedic Surgeon Groote Schuur Hospital, Cape Town
IVFCS(SA)Orth; Consultant Orthopaedic Surgeon, Dept of Orthopaedic Surgery, University of Cape Town, Groote Schuur Hospital, Cape Town
VFCRS(Eng), FCS(SA)Orth, MMed(Orth)UCT; Consultant Orthopaedic Surgeon, Life Orthopaedic Hospital, Vincent Pallotti, Cape Town; From the Princess Alice Orthopaedic Unit, Groote Schuur Hospital, Cape Town
ABSTRACT
PURPOSE: We aimed to assess the short- and medium-term complications of patients who had undergone a modified Latarjet procedure.
METHOD: We retrospectively reviewed the notes and X-rays of all patients identified by surgical log books and/or operation codes for instability. A telephonic follow-up was used to obtain an Oxford Shoulder Score (OSS) and information regarding complications. Patients who had a soft tissue stabilisation procedure were excluded.
RESULTS: The data for 96 shoulders in 93 patients were available for follow-up. Thirty-four complications were noted in 30 patients. These included seven nerve injuries, all of which had resolved at final clinical follow-up; five screw-related complications; five early recurrent dislocations and three early recurrent subluxations, and 14 other minor complications. There was a total re-operation rate of 8%. Patients who developed complications had a median post-op OSS at last follow-up of 21, while those without complications had a median score of 13. A high-risk group of patients was identified. Epileptics, substance abusers and chronic dislocations were statistically more likely to have a poor outcome when they developed complications when compared with patients without these risk factors who developed complications (OSS 35 vs 14, P<0.002). Patients who did not develop a complication had a median OSS of 13.
CONCLUSION: Epileptic patients, substance abusers and chronic dislocations were more likely to develop severe complications following a modified Latarjet. Once a complication occurred their outcomes were significantly worse.
Keywords: Latarjet, complications, anterior instability.
Introduction
There has been a recent increase in the popularity of using the modified Latarjet procedure to treat traumatic shoulder dislocations. This follows the increased recognition of failures of soft tissue reconstructions performed for the unstable shoulder. The published redislocation rates for arthroscopic soft tissue stabilisation procedures is between 5 and 30%.1,2 These high failure rates of the Bankart repair have been shown to be a particular problem in young patients playing contact sports and those with bony deficiencies.3 Dr G Walch, whose procedure of choice is not a Bankart repair but the modified Latarjet, has published results of over 2 000 Latarjet procedures with a 1% failure rate, 98% excellent or good results and 83% of patients returning to pre-injury level of sport.4 He states that complications of this procedure are almost always due to a technical error and therefore can be avoided. It has been proposed that if this is the case then why are we doing any other surgical procedure for the unstable shoulder? But are Dr Walch's results reproducible?
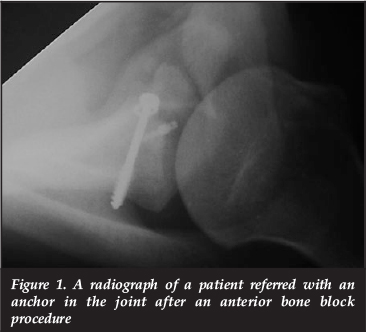
A number of complications of Latarjet procedures were picked up in patients who were referred to the state hospital practice of one of the senior authors (Figures 1 and 2). This prompted a review of the procedures that had been done in the state and private practices of the two senior authors.

The purpose of the study was to review the short- and medium-term complications of the Latarjet procedures performed in our unit; to review the management of these complications and their outcomes; and to identify possible predictive factors which would guide our clinical decision-making.
Method
Clinical notes of all patients with surgically treated instability between 2002 and 2010 were requested for review. These patients were treated at the shoulder unit of a large state hospital by one of the senior authors. The data bases of the senior authors' private practices were searched for procedure codes for instability surgery (0578). From this group all patients who had undergone a Latarjet procedure were included.
Clinical data and available imaging were reviewed and the patients were contacted for a telephonic interview which included an Oxford Shoulder Score (OSS).
The patients' clinical data and Oxford shoulder scores were compared between the groups of patients with complications and those without. The Wilcoxon rank sum test was used to test statistical significance between the two groups. Clinical data collected included past medical history (specifically a history of seizures, alcohol and drug abuse), age of first dislocation, number of dislocations prior to surgery, delay from first dislocation to surgery, estimated size of bone loss (glenoid and Hill-Sachs lesion) and fixation technique of the coracoid graft.
There has been a recent increase in the popularity of using the modified Latarjet procedure to treat traumatic shoulder dislocations
Results
In the state hospital, 192 patients were flagged as having had a surgical procedure for possible shoulder instability; 108 folders were recovered. Eighty of these folders were cases of shoulder instability and 38 of these patients had had a Latarjet procedure. In the private hospital, 58 patients were identified as having had a Latarjet procedure. This gave a total of 96 procedures in 93 patients.
Fifty-three patients (55%) were contactable telephonically for the interview and another 19 (20%) were discharged pain-free without complications or instability. This left an inadequate follow-up in 25% of our patient population. The average clinical follow-up was 7.3 months and the average telephonic follow-up was 30.5 months post-surgery.
Complications
There were 34 recorded complications in 30 patients giving an incidence of 31.25% in an unselected group of all the patients.
Neurological injury
There were seven cases of neurological injury (7.3%). They included three axillary nerve injuries, one musculocutaneous nerve, one median nerve, one suprascapular nerve injury and one patient with superficial sensory alteration of the forearm. All neurological symptoms had resolved at final clinical follow-up.
The axillary nerve injuries recovered at 3, 6 and 7 months and the musculocutaneous nerve recovered at 6 weeks. The median nerve injury was thought to be related to an inter-scalene block and had resolved by 6 weeks. The suprascapular nerve injury was clinically suspected (but not confirmed) as the patient had infraspinatus weakness (4/5) which had resolved at 6 months. The patient with sensory alteration had resolution of symptoms by 7 months.
Two of the patients with axillary nerve injuries and the patient with the musculocutaneous nerve injury had chronic shoulder dislocations.
Screw-related complications
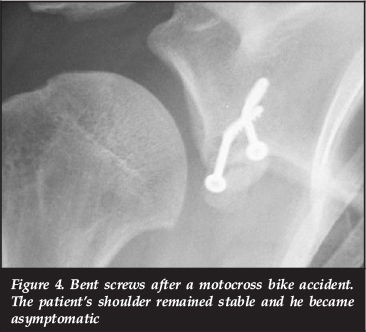
There were five screw-related complications. Three were as a result of irritation from prominent screws; two anteriorly and one posteriorly. There were two patients with bent screws. One was as a result of a motocross bike accident 6 months after surgery and one following a seizure one day after the procedure (Figures 3 and 4). The patient who had the bike accident had no recurrent instability and no further surgery was required. The patient who had the seizure had the graft revised. He has remained stable since his revision.

Three of five screw-related complications were as a result of irritation from prominent screws
Recurrent instability
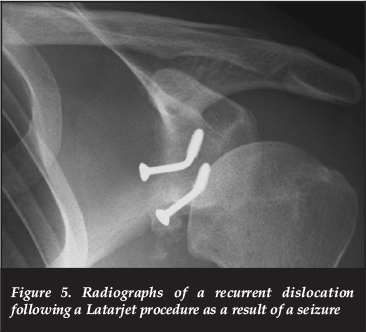
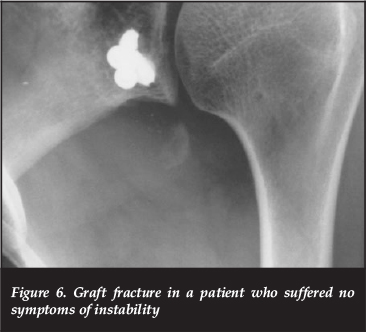
The length of follow-up was not adequate to gauge an overall re-dislocation rate but five patients had recurrent dislocations in the early post-operative period. Two of these were as a result of graft fracture, and one of these was caused by a drug withdrawal seizure. The graft was large enough to be revised. It was turned on its side and re-fixed to the glenoid. The other case was revised to an Eden-Hybinette procedure. There was also one case in which the graft fractured with no further instability 3 years after the procedure. In this case the screws were removed with resolution of symptoms and no further instability (Figures 5 and 6).
One recurrent dislocation was related to graft non-union. The patient redislocated 7 months after his Latarjet and had a revision to an Eden-Hybinette procedure.
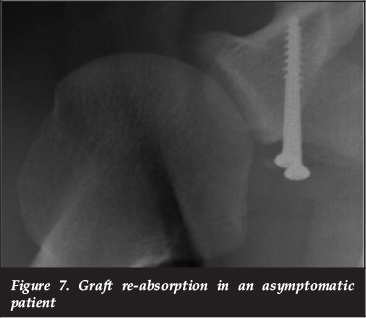
Two of the recurrent dislocations were related to graft resorption; one of these patients had revision to an Eden-Hybinette procedure and the other declined further surgery. There was also one case of graft re-absorption in which no instability resulted (Figure 7). This patient was asymptomatic and had no further surgery.
Three patients had recurrent subluxations. One of these patients had a chronic dislocation prior to surgery and declined the arthrodesis which was offered to him. The other two were epileptic patients who had recurrent seizures and are currently awaiting seizure control prior to arthrodesis for arthritis associated with the subluxations.
There were also two patients who reported subjective shoulder instability which was not reproducible on clinical examination. They are being managed conservatively.
Other complications
There was one case of superficial wound infection which resolved with antibiotic treatment alone. One patient complained of subjective non-anatomic neurology; he unfortunately defaulted follow-up and further investigations which had been organised. There were four patients who had severe shoulder stiffness; all of these patients had Latarjet procedures done for chronic shoulder dislocations and are being managed conservatively.
Other complications included: one patient with bicipital tendonitis which resolved after a steroid injection; one frozen shoulder which was improving at last follow-up; one case in which a lucency was noted around the screws (the patient remained asymptomatic and was managed expectantly); and one case of avascular necrosis and humeral head collapse. The avascular necrosis occurred in a patient who also had a Latarjet for a chronic dislocation. This patient had problems with alcohol abuse and declined further surgery.
Re-operation rate
There was a re-operation rate of 8.3% (eight patients): three had removal of screws (two for prominent anterior screws and one for posterior screw irritation); three had Eden-Hybinette procedures (for recurrent dislocations after the Latarjet procedure); one had a graft revision (for graft fracture following a seizure); and one had an arthrodesis (for persistent subluxation after a chronic dislocation). There were, however, another six patients who were either waiting for or had declined further surgery. This gave a potential re-operation rate of 14.6%.
Past medical history
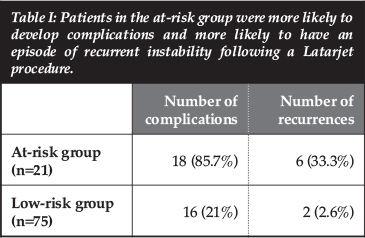
Within the group of patients with chronic dislocations, epilepsy or with a history of substance abuse, there were 18 complications in 15 patients (Table I). We termed this group the high-risk group. There were 16 complications in the rest of the patients in the complication group. This is not a significant difference but six of the eight dislocations or subluxations occurred in this high-risk group (p=0.002).
Oxford Shoulder Score (OSS)
Fifty-three patients were contactable for telephonic OSS (Table II). Twenty of these patients had a recorded complication and 33 had no complications. In the group of patients who had no complications the median OSS was 13 (interquartile range 12-15). In those with complications the median OSS was 21 (interquartile range 13-41). Within the complication group however the group of patients previously defined as high risk had a median OSS of 35 (interquartile range 21-42) and those in the low risk group had a median OSS of 14 (interquartile range 12-20). This was found to be statistically significant using the Wilcoxon rank sum test (p=0.03).
Age of first dislocation
The median age of first dislocation in the patients who had complications was 28.5 years (interquartile range 20-47). In the patients with no complications the median age was 20.5 years (interquartile range 18-26). This was found to be a statistically significant difference with a p-value of 0.02 (Wilcoxon rank sum).
Fixation technique
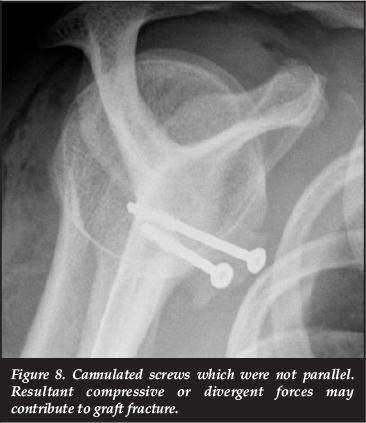
All three patients with broken grafts were fixed using cannulated screws without the use of a jig (Figure 8).
Factors with no influence on complications
The number of dislocations prior to the Latarjet procedure, the delay from the first dislocation to the Latarjet procedure and the estimated size of the bone defect were not found to influence the complications. The sizes of the bony defects were estimated during arthroscopy of the shoulder prior to the Latarjet.
Discussion
The Latarjet procedure has been shown in the literature to be a successful procedure to stabilise the shoulder particularly in the young patients playing contact sport with bone deficiency.3-6 Recent publications have highlighted high complication rates for the modified Latarjet procedure. Shah et al. reported a complication rate of 25%.7 They also felt that they were underestimating the rate of complications with this figure. Walch et al. have the best reported results for the modified Latarjet procedure.5 They do not specifically report an overall complication rate in their study but do mention that there was a 2.4% incidence of graft fracture and a 2.4% rate of graft non-union.
Complications, when they occur, significantly impact on the outcome of the Latarjet procedure
Although some studies have reported relatively high recurrence rates for arthroscopic soft tissue stabilisation procedures (15-30%),2,8 the incidence of other complications is low. A recent Canadian study reported infection in only 0.04% (two of 4 802 patients) and stiffness requiring manipulation under anaesthetic in 0.15%.9
Complications, when they occur, significantly impact on the outcome of the Latarjet procedure (OSS 13 vs OSS 21). This has been confirmed in the literature recently by Shah et al.7 They found good or excellent outcomes in 42% of patients who developed complications and 91% who did not (using the Rowe Score).They were also able to link the rate of complications with three factors: age, Workmen's Compensation claims, and the use of 4.5 mm cannulated screws.7
We could not link the same factors statistically with an increase in complications in our study group. The patients in our study identified as high risk (epileptics, substance abusers and patients with chronic shoulder dislocations) had particularly poor outcomes when they developed complications when compared to those patients without these conditions who developed complications (OSS 14 vs 35).
Poor outcomes after the Latarjet procedure have also been documented in epileptics by Walch et al.10 They documented unacceptably high recurrence rates of 43% in this patient group. All recurrences occurred at the time of a seizure. They recommended that 'The Latarjet procedure should be reserved for the well-controlled patient with epilepsy who has recurrent anterior dislocation of the shoulder during activities of daily living'.10 Where seizure control is not possible and surgery is required, an Eden-Hybinette procedure may be a better choice for primary stabilisation of these patients. Hutchinson et al. reported no dislocations in a group of 13 epileptic patients treated with an anterior glenoid bone block.11 Their follow-up was limited to 2.7 years. Other studies with longer follow-up have however reported dislocations following anterior glenoid bone block procedures.10, 12 Medical control of the seizures prior to surgery whenever possible is required.
The assessment of recurrence rates of instability following a Latarjet procedure requires follow-up of at least 5 years.13 Our follow-up was not adequate to estimate a total rate of recurrence but did give an indication of early recurrence. In our study group, six of the eight patients with early recurrence fell into the high-risk group. Four were seizure related. Burkart et al.14 reported four recurrences in the early post-op period; one related to seizures and three to significant trauma (excessive alcohol was involved in one of these cases). The majority of early recurrences seem to be related to significant recurrent trauma or seizures. Shah et al. found early recurrences related to graft non-union or resorption in three of four recurrences and only one was related to trauma.7 Other studies have not been able to link coracoid graft osteolysis and fibrous union with recurrent dislocation despite high levels of graft lysis (59.5%).3,15
There was a significant incidence of neurological injury following this procedure (7.3%) but all of these nerve injuries resolved. This is a similar rate to the 8.2% noted by Ho et al.16 for open anterior shoulder stabilisation procedures. Shah et al. found a neurological complication rate of 10%.7 They found primarily sensory deficits of the radial and musculocutaneous nerves and that these injuries did not significantly impact on long-term outcomes.7
All three incidences of graft fractures were in patients initially fixed with cannulated screws without the use of a guiding device or jig. We thought that the thin guide wires may have had an increased propensity to diverge or converge when inserted as compared to the initial placement of a 2.5 mm drill bit. This would then result in divergent or convergent forces across the graft when the screws were tightened and might have led to the fractures. The cannulated screws were also 4 mm screws (as opposed to the 3.5 mm cancellous screws which were otherwise used) which also may have impacted on the graft weakness. Graft fracture was not experienced when a guiding device for the same 4 mm cannulated screws was used. Shah et al. also warned against the use of 4 or 4.5 mm cannulated screws but for a different reason.7 They found a high incidence of instability related to the use of cannulated screws but attributed it to graft non-union. They postulated that the fixation to the glenoid was not as secure because the cannulated screws were partially threaded and had short thread length.
There was one case of superficial infection in our group of patients. Infection rates are not reported in many other papers on the subject. Shah et al. report a 6% infection rate.7
These were infections which required further surgery. Allain et al. reported three infections in 95 patients.17 Walch et al.4 and De Beer et al.18 reported peri-operative infection as being extremely rare.
Patients undergoing this procedure, who fall into the high-risk group, should be warned of the potential high re-operation rate, 8.3% in our study. This would be much higher if all patients either waiting for or declining further surgery were included (14.6%). Hovelius et al. reported a 4% re-operation rate in his study on long-term follow-up of Latarjet patients13 and Allain et al. a 4.2% re-operation rate.17 Hovelius et al.13 reported removal of screws in five patients, and in the paper by Lafosse et al,19 four patients required screw removal, but reasons for their removal were not given in either case. Other authors have also reported on the need for screw removal due to posterior pain.18 Three patients in our study developed symptoms related to prominent screws. Two of these patients had anterior irritation and one had posterior symptoms. The screws were removed and they became asymptomatic. Three other patients had revisions to Eden-Hybinette procedures. These were as a result of recurrent dislocations after the Latarjet. One patient had the graft revised after it fractured in the early post-op period as a result of a seizure. One other patient had an arthrodesis after a failed Latarjet for a chronic shoulder dislocation.
The age of first dislocation was found to be higher in the patients who developed complications following the Latarjet. Most of the patients with chronic dislocations were older at the time of their first dislocation and this group had a higher complication rate. This probably skews the data for this variable.
Conclusions
Short length of follow-up and limited telephonic follow-up are limitations of this study. Despite this we feel there is important information that can be gained from this research:
- Patients who develop complications following a Latarjet have poor clinical outcomes.
- Those with epilepsy, substance abuse and chronic dislocations have an increased risk of recurrent instability and worse outcomes when they develop a complication. An alternative procedure may be better in these cases.
- Neurological injuries, when they occur, seem to recover.
- Cannulated screws may result in an increased fracture rate when used without a guide or jig.
- Importantly those patients who did not have a complication did very well.
This study has been approved by the research ethics committee of the University of Cape Town.
No commercial benefits have been or are to be received from a commercial party related directly or indirectly to the subject of the article. Funding was received in the form of an institutional grant for a shoulder and elbow fellowship at the University of Cape Town from Johnson&Johnson and SA Biomedical.
References
1. Garofalo R, Mocci A, Moretti B, Callari E, Di Giacomo G, Theumann N, Cikes A, Mouhsine E. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy 2005;21:1283-89 [ Links ]
2. Koss S, Richmond JC, Woodward JS Jr. Two- to five-year follow-up of arthroscopic Bankart reconstruction using a suture anchor technique. Am J Sports Med. 1997;25:809-12. [ Links ]
3. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [ Links ]
4. Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg 2011;20:S61-S69 [ Links ]
5. Walch G, Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg 2000;1:256-61. [ Links ]
6. Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg [Br] 2007;89:1470-77 [ Links ]
7. Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JP. Short-Term Complications of the Latarjet Procedure. J Bone Joint Surg [Am]. 2012;94:495-501. [ Links ]
8. Boileau P, Villalba M, Hery, JY Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthro-scopic Bankart repair. J Bone Joint Surg [Am] 2006;88:1755-63. [ Links ]
9. Wasserstein D, Dwyer T, Veillette C, Gandhi R, Chahal J, Mahomed N, Ogilvie-Harris D. Predictors of dislocation and revision after shoulder stabilization in Ontario, Canada, from 2003to 2008. Am J Sports Med 2013;41:2034-40. [ Links ]
10. Raiss P, Lin A, Mizuno N, Melis B, Walch G. Results of the Latarjet procedure for recurrent anterior dislocation of the shoulder in patients with epilepsy. J Bone Joint Surg [Br] 2012;94:1260-64. [ Links ]
11. Hutchinson JW, Neumann L, Wallace WA. Bone buttress operation for recurrent anterior shoulder dislocation in epilepsy. J Bone Joint Surg [Br] 1995;77:928-32. [ Links ]
12. Buhler M, Gerber C. Shoulder instability related to epileptic seizures. J Shoulder Elbow Surg 2002;11:339-44. [ Links ]
13. Hovelius L, Sandstrom B, Olofsson A, Svensson O, Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012;21:647-60. [ Links ]
14. Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007;23:1033-41. [ Links ]
15. Di Giacomo G, Costantini A, De Gasperis N, De Vita A, Lin BKH, Francone M, Rojas Beccaglia MA, Mastantuono M. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: a computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg 2011;20:989-95. [ Links ]
16. Ho E, Cofield RH, Balm MR, Hattrup SJ, Rowland CM. Neurologic complications of surgery for anterior shoulder instability. J Shoulder Elbow Surg. 1999;8:266-70. [ Links ]
17. Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg [Am] 1998;80:841-52. [ Links ]
18. De Beer JF, Roberts C. Glenoid bone defects - Open Latarjet with congruent arc modification. Orthop Clin N Am} 2010;41:407-15. [ Links ]
19. Lafosse L, Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg 2010;19:2-12. [ Links ]
 Correspondence:
Correspondence:
Dr J-P du Plessis
PO Box 897
7450 Howard Place
Cape Town, South Africa
Tel: 021 506 5580
Fax: 021 506 5581
Email: jp@shoulderelbow.co.za
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.














