Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.13 no.3 Centurion Set. 2014
TUMOUR AND INFECTION
Intraneural lipoma of the common peroneal nerve: A case report and review of the literature
P RyanI; M ter HaarII; A RocherIII; I GogaIV
IMBChB(UCT), HDip(Orth), MMed(Orth), FCOrth(SA); Orthopaedic Surgeon; Department of Orthopaedic Surgery, Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-Natal
IIMBChB, FCOrth(SA); Orthopaedic Surgeon; Department of Orthopaedic Surgery, Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-Natal
IIIMBChB, FCOrth(SA); Orthopaedic Surgeon; Department of Orthopaedic Surgery, Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-Natal
IVMD, RFCS(Edinburgh), FCS(Orth)(SA); Professor and Head of Arthroplasty and Reconstruction Unit; Department of Orthopaedic Surgery, Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-Natal
ABSTRACT
Intraneural lipomas are rare hamartomas, encompassed within the spectrum of fatty lesions associated with peripheral nerves. More commonly associated with nerves of the upper limb, there are few reports of intraneural lipomas associated with nerves of the lower limb. In these cases they are usually found around the foot and ankle, or more proximally in the upper thigh or hip.
We report a case of an intraneural lipoma associated with the common peroneal nerve: the presenting features, diagnosis and subsequent management. We give a concise review of fatty lesions associated with peripheral nerves, and in particular, intraneural lipomas.
Keywords: lipoma, intraneural lipoma, common peroneal, compression neuropathy, fibrolipoma.
Introduction
Benign fatty lesions of peripheral nerves are uncommon, and when they occur, typically affect the nerves of the upper limb. There are only a handful of reports describing cases in the lower limb, and these are mostly confined to distal branches of the superficial peroneal nerve at the foot and ankle.
Due to its rare occurrence, we report a case of an intra-neural lipoma associated with the common peroneal nerve (CPN), presenting as a compression neuropathy.
Case report
A 25-year-old female patient presented with a 12-month history of progressive pain in the lateral aspect of her right leg. She had associated numbness over the fourth toe running proximally up to the fibula head for five months.
There were no associated constitutional symptoms, and she was otherwise well.
Clinical examination demonstrated full, painless movement of her lumbar spine and hip. Straight leg raise test was negative, and there was no gross lower limb malalignment. Local examination of the knee revealed no skin abnormalities. A vague swelling around the lateral aspect of the knee was noted, extending 5 cm below the level of the fibular head. It was tender over the area of the fibular head and slightly more distally. Local percussion along the common peroneal nerve reproduced her neurological symptoms.
There was some paraesthesia in an area extending from the fibula head down to the fourth toe. There was very mild weakness with power graded 4+ in the right tibialis anterior and extensor hallucis longus muscles. Neurological examination of the upper limbs and the left lower limb revealed no abnormality.
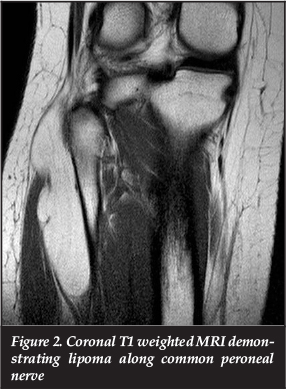
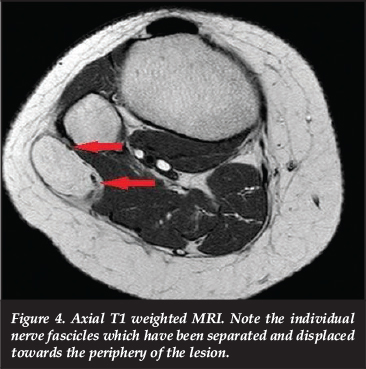
Plain radiographs of the affected limb (Figure 1) revealed a slight increase in the local soft tissue shadow with no underlying bony abnormality. Magnetic resonance imaging (MRI) (Figures 2 to 4) revealed a benign-appearing tumour, most likely a lipoma, with iso-intensity to normal fat on T1 and fat-suppressed sequences. The lesion originated at the level of the knee joint, and followed the common peroneal nerve distally, around the neck of the fibula and into the antero-lateral calf. In view of the progressive nature of her symptoms, and the radiological appearance of an evolving compressive neuropathy, the patient was offered operative intervention.


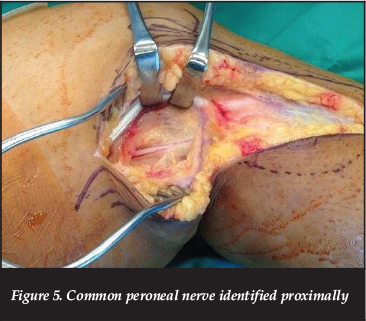
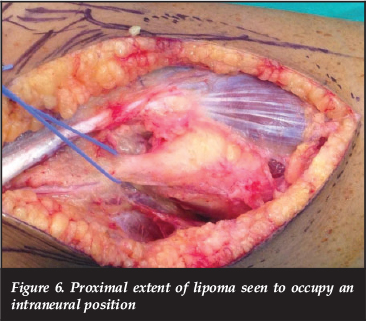
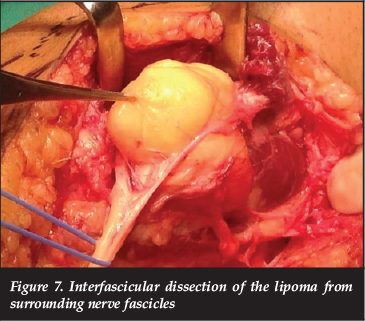
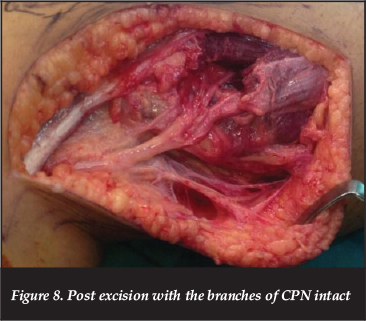
At surgery, a curvilinear incision was utilised, beginning 7 cm above the knee joint line on the lateral side, and extending to the antero-lateral aspect at the upper-calf level. The common peroneal nerve was identified proximally under the hamstring tendon (Figure 5), and followed distally. The proximal extent of the lesion was identified intraneurally (Figure 6), and an interfascicular dissection of the tumour from the nerve was continued distally (Figure 7) to below the level of the fibular neck, with care taken not to injure branches of the CPN (Figure 8). The excised tumour measured 11 cm x 6 cm x 3 cm, and macroscopically resembled lipomatous tissue, with a homogenous yellow colour, firm consistency and lobulation (Figure 9).

Histological evaluation showed features consistent with a benign fatty lesion with well-encapsulated mature adipose tissue. There were no associated chondroid elements, and a histological diagnosis of a benign lipoma was made.
The patient had an uneventful post-operative course. There was no neurological complication, and at nine-week follow-up, the patient had regained full strength in the antero-lateral calf musculature, and normal sensation had returned to the antero-lateral calf and toe.
Discussion
While adipose tissue is a normal constituent of epineural and perineural tissue, lipomatous lesions associated with peripheral nerves are rare. They may be classified according to their location: intraneural versus extraneural; their pathological activity: infiltrating (lipomatous) or not (lipoma); and by their histological contents: whether they contain fibrous or chondroid elements.
Lipomatous lesions associated with peripheral nerves are rare
Lipomatosis refers to an infiltration of fatty tissue intimately involved with a nerve. It may be associated with a local increase in mesenchymal growth, or focal gigantism. In these cases the term 'macrodystrophia lipomatosa' may be used. In extreme cases it may be more generalised and associated with syndromes such as Proteus and Klippel-Trenaunay.1-3 Surgical excision of the lipomatous tissue inevitably involves damage to, or excision of the associated nerve, and surgical debulking of distal hypertrophied tissues may be required.
In contrast, lipomas have a much more benign clinical course. They are hamartomas arising from the normal epineural fat tissue, and may be intraneural or extra-neural. They are focal, well demarcated and tend to displace rather than invade or surround nerve fascicles,3 as seen in this case. They are not associated with local bone and tissue overgrowth.
Historically the terminology for these lesions has had little conformity. Terms included intraneural lipoma, neural fibrolipoma, lipofibromatous hamartoma, perineural lipoma, macrodystrophia lipomatosa, lipomatosis of nerve, fibrolipomatous hamartoma, and fatty infiltration of nerve.
Recently, in an attempt to clarify the nomenclature, Spinner et at.3 divided the lesions into two groups:
- Group 1 included the basic lesions of lipomas and lipomatosis as separate entities, which could occupy either an intraneural or extraneural position.
- Group 2 contained combined lesions. These combined lesions could be:
- A single basic lesion (e.g. lipoma or lipomatosis) in both an intraneural and extraneural position.
- Both basic lesions in a single position, e.g. intraneural lipoma with associated intraneural lipomatosis
- Combined lesions in differing positions.
The authors further emphasised the concept that these adipose lesions form a broad yet interrelated spectrum of pathology.
Intraneural lipomas most commonly affect the nerves of the upper limb. The median nerve4-9 is the most frequent, but they have been described in the ulnar,8, 10 radial,11 musculocutaneous,8 and axillary nerves,8 as well as in the brachial plexus.8, 12
In the lower limb, the majority arise from small branches of the common peroneal nerve around the ankle and foot,13, 14 and others arise more proximally from the sciatic nerve.8, 15, 16
There are few reports of intraneural lipomas affecting the CPN. One paper describes an intraneural chondroid lipoma of the CPN17 which had similar clinical and MRI features, but varying histological characteristics, and a single other case in the Italian literature describes a giant lipoma of the sciatico-popliteal nerve.18
Severe pain should be a warning sign, as intraneural lipomas are typically painless, or cause only minor discomfort
Three papers report on cases of compression of the CPN by extraneural lipomas,19-21 i.e. the origin of the fat cells was not of neural tissue.
Diagnosis of intraneural lipoma may be suspected on clinical grounds. Sabapathy et at.14 highlight the features of mass consistency, association with a cord-like structure, free medial to lateral mobility with little longitudinal mobility, and no association with tendon movement as key clinical features. They do, however, suggest further imaging by MRI scan should the diagnosis be less clear, or on the suspicion of possible malignancy. Severe pain should be a warning sign, as intraneural lipomas are typically painless, or cause only minor discomfort.6, 10, 13 Typical MRI findings include tissue with signal characteristics identical to subcutaneous fat: bright signal on T1 and dark signal on fat-suppressed images.
Two reports19,20 highlight the usefulness of ultrasound imaging over MRI scanning in the diagnosis of compression neuropathies of superficial nerves by lipomas. However, despite this and other advantages such as cost and availability, operator dependence still remains a concern.
In most instances, surgical management yields excellent results, and recurrence or malignant change are rare.13 Preservation of distal neurologic function may be achieved with careful dissection of neural structures. This may, however, not be necessary in cases where the involvement is that of a distal sensory nerve alone, where sacrifice of the nerve and en-bloc resection is an acceptable option.14
In our case, the position of the lipoma within the CPN resulted in the splaying of the numerous nerve divisions over the mass. This required meticulous dissection aided by magnification. Fortunately, there was no neurological complication; however, pre-operative patient counselling regarding potential neurological fallout cannot be overemphasised.
Summary
Intraneural lipomas are rare lesions, but should be considered in the differential diagnosis of patients presenting with compressive neurological symptoms. Clinical suspicion aided by relevant investigations make diagnosis relatively straightforward. Surgical excision with care taken of neurological structures gives excellent results.
The content of the article is the sole work of the authors. No benefits of any form have been or are to be received from a commercial party related directly or indirectly to the subject of the article. The patient gave consent for the use of clinical records and radiographic materials.
References
1. Meirer R, Huemer GM, Shafighi M, Kamelger FS, Hussl H, Piza-Katzer H. Sciatic nerve enlargement in the Klippel-Trenaunay-Weber syndrome. Br J Plast Surg 2005;58(4):565-68. [ Links ]
2. Biesecker LG. The multifaceted challenges of Proteus syndrome. JAMA 2001;285(17):2240-43. [ Links ]
3. Spinner RJ, Scheithauer BW, Amrami KK, Wenger DE, Hebert-Blouin MN. Adipose lesions of nerve: the need for a modified classification. J Neurosurg 2012;116(2):418-31. [ Links ]
4. Abu Jamra FN, Rebeiz JJ. Lipofibroma of the median nerve. J Hand Surg Am 1979;4(2):160-63. [ Links ]
5. Morley GH. Intraneural lipoma of the median nerve in the carpal tunnel. Report of a Case. J Bone Joint Surg Br 1964;46:734-35. [ Links ]
6. Rusko RA, Larsen RD. Intraneural lipoma of the median nerve-case report and literature review. J Hand Surg Am 1981;6(4):388-91. [ Links ]
7. Watson-Jones R. Encapsulated lipoma of the median nerve at the wrist. J Bone Joint Surg Br 1964;46:736. [ Links ]
8. Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 146 peripheral non-neural sheath nerve tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg 2005;102(2):256-66. [ Links ]
9. Carvi y Nievas MN, Archavlis E, Unkel B. Delayed outcome from surgically treated patients with benign nerve associated tumors of the extremities larger than 5 cm. Neurol Res 2010;32(6):563-71. [ Links ]
10. Balakrishnan C, Saini MS, Demercurio J. Intraneural lipoma of the ulnar nerve: A case report and review of literature. Can J Plast Surg 2006;14(1):49-50. [ Links ]
11. Balakrishnan C, Bachusz RC, Balakrishnan A, Elliot D, Careaga D. Intraneural lipoma of the radial nerve presenting as Wartenberg syndrome: A case report and review of literature. Can J Plast Surg 2009;17(4):e39-41. [ Links ]
12. Chatillon CE, Guiot MC, Jacques L. Lipomatous, vascular, and chondromatous benign tumors of the peripheral nerves: representative cases and review of the literature. Neurosurg Focus 2007;22(6):E18. [ Links ]
13. Terrence Jose Jerome J. Superficial peroneal nerve lipoma. Rom J Morphol Embryol 2009;50(1):137-39. [ Links ]
14. Sabapathy SR, Langer V, Bhatnagar A. Intraneural lipoma associated with a branch of the superficial peroneal nerve. J Foot Ankle Surg 2008;47(6):576-8. [ Links ]
15. Chiao HC, Marks KE, Bauer TW, Pflanze W. Intraneural lipoma of the sciatic nerve. Clin Orthop Relat Res 1987(221):267-71. [ Links ]
16. Godquin B, Brunelli M, Basso M. [Giant lipoma of the sciatic nerve (author's transl)]. Chirurgie 1978;104(3):221-24. [ Links ]
17. Park SE, Lee JU, Ji JH. Intraneural chondroid lipoma on the common peroneal nerve. Knee Surg Sports Traumatol Arthrosc 2011;19(5):832-34. [ Links ]
18. Crescente D, Cucco D. [Giant lipoma of the external sciatico-popliteal nerve]. Chir Organi Mov 1981;67(3):357-60. [ Links ]
19. Hsu YC, Shih YY, Gao HW, Huang GS. Subcutaneous lipoma compressing the common peroneal nerve and causing palsy: sonographic diagnosis. J Clin Ultrasound 2010;38(2):97-99. [ Links ]
20. Vasudevan JM, Freedman MK, Beredjiklian PK, Deluca PF, Nazarian LN. Common peroneal entrapment neuropathy secondary to a popliteal lipoma: ultrasound superior to magnetic resonance imaging for diagnosis. PM R 2011;3(3):274-79. [ Links ]
21. Seki N, Okada K, Miyakoshi N, Shimada Y, Nishida J, Itoi E. Common peroneal nerve palsy caused by parosteal lipoma of the fibula. J Orthop Sci 2006;11(1):88-91. [ Links ]
 Correspondence:
Correspondence:
Dr P Ryan
Arthroplasty Unit
Department of Orthopaedic Surgery
Inkosi Albert Luthuli Central Hospital
Private Bag X03
Mayville, KZN, 4058
Tel: +27 (31) 240 2160
Email: paullisa.ryan@gmail.com
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.














