Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.13 no.3 Centurion Set. 2014
HIP
The rise and fall of large bore metal-on-metal hip prostheses
Ian D Learmonth
MBChB, FRCS, FRCS(Ed), FCS(SA)Orth; Emeritus Professor, University of Bristol
ABSTRACT
Metal-on-metal was the first articular couple to be successfully used in total hip replacement. Large heads and high frictional torque resulted in a high incidence of implant loosening. This led Charnley to introduce the low friction arthroplasty where the torque was reduced by using small heads and low friction hard-on-soft bearings.
Osteoarthritis is a disease of cartilage, and resurfacing arthroplasty is therefore intuitively the logical conservative surgical solution. The early resurfacing devices with metal-on-plastic bearings were associated with catastrophic wear of the plastic. In the 1990s resurfacing was revisited, and metal-on-metal was selected to resolve the challenge of the bearing surface.
Various factors were not initially recognised as being critical for the successful outcome of these implants. These include the importance of component orientation, the significance of an adequate 'arc of cover', the prevalence of edge loading, and the impact of microseparation. In addition the biological response - pseudotumour/ALVAL etc. - was unpredicted and unexpected.
Femoral neck fractures in patients with a resurfacing arthroplasty were treated by revision to a stemmed implant with a large head. However this option was seen to have a wider application than resurfacing, was perceived as a 'high performance bearing' and addressed the problem of dislocation - one of the commonest causes of revision. These large bearings provided a dislocation 'safety net' to surgeons, many of whom consequently became less meticulous about component orientation. Liberation of metallic debris by fretting and corrosion at the taper junction between the large head and the taper of the stem - totally unforeseen by the bioengineers - emerged as a real problem in these hips.
This paper attempts to scientifically place some of these issues in perspective against the backdrop of hysteria created by legal colleagues and the media.
Keywords: hip, large metal bearings, failure.
Introduction
Metal-on-metal (MoM) was the bearing of choice in the early 1960s, using a monobloc stem with a large head. These prostheses (McKee-Farrar, Huggler, Müller etc.) were made of cobalt-chromium molybdenum alloy, and exhibited a very low wear, even up to 20 years after implantation.1 Poor component design - low head neck offset, poor prosthetic fixation, etc. - often led to early failure. However Brown et at.2 reported an 84% survivorship of the McKee-Farrar (Figure 1) at 20-year follow-up, while Jacobsson et at.3 noted that the long-term results of the McKee-Farrar were comparable to those of the Charnley low friction arthroplasty.

The high early incidence of loosening of these early large bore MoM articulations was attributed to increased shear stresses at the fixation interface consequent upon the high friction at the bearing interface. This led to Charnley introducing low friction hard-on-soft bearings - metal on ultra-high molecular weight polyethylene.
This paper attempts to scientifically place some issues in perspective against the backdrop of hysteria created by legal colleagues and the media.
In 1995 Harris noted that 'the problem is osteolysis'.4 Aseptic loosening was the commonest cause of failure of total hip replacement, and osteolysis was the commonest cause of aseptic loosening. By this time it was recognised that osteolysis was particle and particle access disease, and that micron and submicron particles of polyethylene were the main culprit. In a hard-on-soft bearing, wear is proportional to load and distance travelled. The larger the bearing, the greater the distance travelled. Early attempts at resurfacing with a polyethylene cup and a metal head in the 1970s resulted in predictably high volumetric wear of the plastic, which was associated with osteolysis and catastrophic failure.5
The recognised limitations of high density polyethylene resulted in the development of alternative bearings -highly cross-linked polyethylene, metal-on-metal and ceramic-on- metal. MoM bearings do not fracture, are self-healing, generate very low volumetric wear, and can be used for large bore couples. MoM therefore met the requirements for resurfacing, namely, the use of thin components to avoid undue resection of the femoral head and acetabulum, the use of large heads, and the use of materials with an established record in clinical practice.
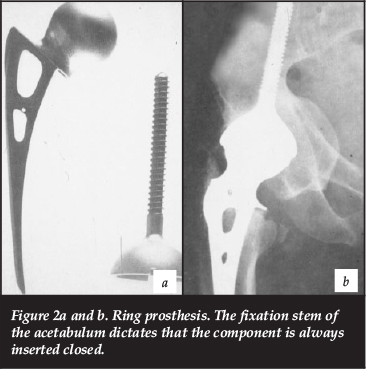
The Ring prosthesis (Figure 2), a monobloc large-bore MoM hip, had a survivorship of 95% at 15-16 years.6 Recognising the potential value of this technology, McMinn approached Corin Medical Ltd (Cirencester) whose engineers had experience of manufacturing the Ring prosthesis. This collaboration produced a MoM resurfacing device that was the forerunner of the Birmingham Hip Resurfacing (BHR).7
Resurfacing arthroplasty (RA) gained substantial traction at the turn of the century and increasing patient and surgeon demand dictated that virtually all orthopaedic companies included a resurfacing device in their portfolio.
Femoral neck fractures occur in up to 1.5% of RAs, and are the commonest cause of early failure of these devices. In these circumstances it is only necessary to revise the femoral component. All companies therefore manufactured a range of modular large diameter metal heads that would articulate with the monolithic resurfacing cups and could be applied to stemmed femoral implants.
Crownshield8 noted that large heads were associated with a decreased risk of dislocation, both because of the increased range of movement to impingement, and because of the increased jump distance - represented by the radius of the femoral head. The reduced incidence of dislocation associated with larger heads was confirmed in clinical practice.9, 10
Hip registries identified dislocation as the commonest cause of early revision and the second commonest cause of revision. Large bore MoM bearings seemed like a panacea: a 'high performance bearing' with virtually no risk of dislocation, no risk of fracture and very low wear.
So what went wrong?
Resurfacing arthroplasty
Arthritis of the hip primarily involves the articular surfaces and subchondral bone of the joint. Intuitively therefore resurfacing of the joint is the logical conservative surgical option.
Factors contributing to the failure of RA devices include poor patient selection - rheumatoid arthritis, osteoporosis, avascular necrosis, etc
It should be recognised at the outset that some resurfacing prostheses have performed remarkably well in selected patients. McMinn et at.11 reported a 99% and 98% survivorship of the BHR at 10 and 15 years respectively in male patients with osteoarthritis. Coulter et at.12 reported a 97.5% survivorship of the BHR in males at a mean follow-up of 10.4 years. The survivorship in females was only 89.1%.
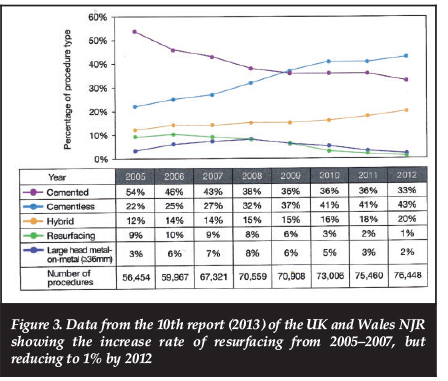
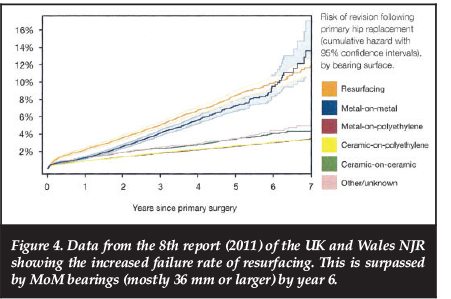
The aggressive promotion of the early success of RA resulted in an increased demand for resurfacing around 2005-2007 (Figure 3). However an unexpectedly high failure and revision rate (Figure 4) resulted in a marked decrease in resurfacing activity over the past few years (Figure 3).
Factors contributing to the failure of RA devices include poor patient selection - rheumatoid arthritis, osteoporosis, avascular necrosis, etc. - which was often associated with an increased incidence of femoral neck fracture.
Loosening of the acetabular component is one of the commonest causes of failure of large bore MoM implants. One of the main contributory factors is the significant torque generated by the high frictional resistance encountered at the articular interface of these bearings in the absence of a favourable lubrication regimen13 - for example, when rising from a sitting position, edge loading, etc. It should be noted that edge loading will itself markedly increase torque on the cup. In addition acetabular implants with a low clearance and a thin shell - designed to limit bone resection - were susceptible to deformation and equatorial binding when inserted into hard sclerotic bone. This produced enormous shear forces at the fixation interface which often culminated in loosening of the cup.
An increased generation of metallic debris is associated with an increased incidence of pathological biological responses, which often predicates the need for revision. Factors contributing to an increased generation of metallic debris include:
1. Any of the following factors that reduce the 'arc of cover' (Figure 5) and increase the wear at the articular interface:
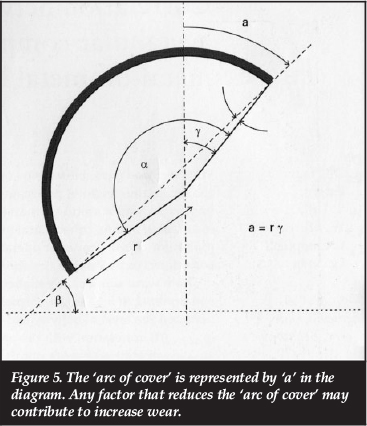
- Small acetabular components (more commonly used in females)
- Cups that are more vertically orientated
- Sub-hemispherical cups (as depicted in Figure 5)
- A Trendelenburg gait, which is associated with a functional reduction in the 'arc of cover'
- Other design features of the cup - such as the locator groove for the cup insertion device of the ASR
- Developmental dysplasia of the hip: The morphology of the acetabulum dictates that the cup is often inserted too 'open'.
2. Rim or edge loading can occur where the cup is malorientated - either too vertical or with excessive ante or retroversion. Morlock et al.14have shown that rim-loaded implants exhibited an average 21- to 27fold higher wear rate than implants without rim loading. In addition, rim-loaded implants showed a steeper mean cup inclination than their non-rimloaded counterparts (59° vs 50°).
It should be remembered that the articular relationship between the femoral head and the acetabular component is affected by the orientation of both components. The orientation of the femoral components is seldom considered in the literature - even though a markedly valgus or retroverted head will provoke edge loading.
3. Microseparation is a potent cause of increased wear. Leslie et al.15 noted that bearings tested with a cup inclination of 60° had nine-fold higher wear rates than bearings tested with a cup inclination of 45°. However, if the increased cup angle was combined with microseparation, wear rates increased by 17-fold compared to the standard.
Microseparation provokes edge loading and can occur following RA where poor bone quality or avascular bone dictates that more bone than usual is moved from the pole of the head. As resurfacing does not readily allow for the adjustment of length, microseparation may occur at the articular interface. Collagen deficiency and joint laxity - as for example encountered with Ehlers Danlos syndrome - can also result in microseparation.
Microseparation can therefore be the cause of increased metal wear even where the implants appear radiologically perfectly orientated.
An increased generation of metallic debris is associated with an increased incidence of pathological biological responses
XL-THR
The genesis of XL-THR has been described above. The concept of a high performance bearing with virtually no risk of dislocation proved very attractive to surgeons, and the use of XL-THR rapidly surpassed that of RA. However, unexpectedly the failure and revision rate of these implants exceeded those of RA.16 Garbuz et al. reported that the blood metal ion levels were approximately ten-fold higher with the XL-THR than in a matched cohort of RA. Long et al.17 reviewed 181 XL-THR at mean follow-up of 1-2 years, and noted that 15% had been revised while 14% had clinical and/or radiological signs of impending failure.
XL-THR is susceptible to the same issues at the MoM articular interface as RA. However, all total hip replacements with large MoM bearings are also susceptible to fretting and corrosion at the head/taper junction. This is associated with the liberation of metallic debris and a significant incidence of Adverse Reaction to Metallic Debris (ARMD).
There are many factors that would predispose to fretting or corrosion with failure at the taper junction. These include:
1. A contaminated taper (blood/fat etc.): It is essential with any modular head to meticulously clean and dry the taper before application of the head.
2. The head is not sufficiently firmly impacted to fully engage the taper.
3. The head is not applied axially in line with the taper. This can prevent full seating of the head, consequently provoking early micromotion with fretting and corrosion.
4. Cone angles have been reduced and trunnions have been made shorter with resultant increased localised stresses.
5. Most of these large 'endoheads' are applied onto a sleeve which is fitted to the taper. Some of these sleeves are titanium, and the titanium/titanium junction in this setting is associated with significant fretting and corrosion.
6. Larger heads are associated with an increased 'arc of cover' and reduced wear in RA. However, the larger the head in an XL-THR, the greater the head taper offset (Figure 6).18 This results in increased torque and bending moments at the taper, with a consequent increased risk of fretting and associated corrosion. High body weights and activities are associated with higher loads, which could increase the risk of fretting-induced implant failure in the clinical setting.

It was probably the unexpectedly high failure rate of these THRs with large bore MoM bearings (>36 mm) which induced Smith et al.19 to comment that 'Metal-on-metal stemmed implants give poor implant survival compared to other options and should not be implanted'.
Biological response to metal debris
It should be recognised that metal ions are released from any metal implanted in the body. These can be widely distributed throughout the body even with a metal-on-polyethylene bearing.20 Well-functioning metal-on-metal bearings have very low volumetric wear, but generate a very large number of tiny nanometre particles. MoM bearings functioning in adverse conditions are associated with increased volumetric wear, and the generation of larger particles. The uptake of particles smaller than 150 nm is mediated by the cell membrane through endocytosis and pinocytosis.21 Particles larger than 150 nm can stimulate phagocytosis by specialised cells such as macrophages.22 Particle size will therefore influence the genesis of the biological response.
Co and Cr ions may cause mutagenicity (DNA damage, aneuploidy), allergy, type four T-cell mediated hypersensitivity (aseptic lymphocyte-dominated vasculitis-associated lesion or ALVAL), toxicity (cell death) and a cyto-chemical response (chronic inflammatory/granulomatous).
The biological response to metallic debris is influenced both by the volume of debris and the morphology of the particles.
Daley et at.23 showed that wear debris damaged chromosomes in a dose-dependent manner. However, after reviewing the evidence, the MHRA (Medicines and Health Regulatory Agency - UK) concluded that there was no evidence that elevated levels of Co and Cr were associated with clinical effects. Nevertheless, given the long-term latent period to the expression of small particle disease, Learmonth and Case24 have noted that 'there is no room for complacency'.
'Pseudotumours' in association with MoM resurfacing were first reported by Pandit et at. in 200825 in three different resurfacing devices. These lesions can be cystic or solid, and can be very large, invading the periprosthetic soft tissues (Figures 7a and b). These patients typically present with pain and a local or regional swelling, but may also exhibit a neuropathy, instability, etc.
Pseudotumours' are typically characterised histologically by extensive necrosis, although there may also be heavy infiltrates of lymphocytes.
These lesions are usually dose-dependent, although they can occur in asymptomatic patients, and in patients with normal levels of metal ions.
Non-dose-dependent biological reactions to metallic debris include allergies and ALVAL (aseptic lymphocyte-dominated vasculitis-associated lesion). Allergies associated with metal implants are well documented in the literature, but are relatively rare. They may be elicited by nickel, cobalt and chromium -constituents of all RA and XL-THR bearings.
These patients often present with widespread rashes on the trunk and limbs, which quickly resolve when the implants are exchanged for titanium alloy implants combined with a ceramic/ceramic or ceramic/polyethylene articulation.
ALVAL was reported by Willert et at26 in 2005 in a series of patients with 28 mm MoM heads. The patients presented clinically with pain around the hip and signs of synovitis and an effusion. It is typically associated with low wear, and the diagnosis confirmed histologically with perivascular lymphocytic cuffs together with plasma cells and macrophages that contain metal particles. Davies et at27reported similar findings and suggested that this was some form of immunological response that could represent a novel biological mechanism that could lead to early failure of MoM devices. ALVAL appears to be an idiosyncratic delayed T-cell type four hypersensitivity reaction, which seems to occur relatively rarely.
Discussion
A metal-on-metal bearing produces very low wear, is 'self-healing' and does not fracture. So what went wrong? Randelli et at.28 have reported a 95% survivorship of 28 mm Metasul MoM bearings at 15-year follow-up. A huge number (>100 000) of these bearings have been inserted without reports of Adverse Reaction to Metallic Debris (ARMD) - except for the occasional case of ALVAL.
Histological patterns similar to ALVAL were noted in the periprosthetic tissue around a small number of McKee-Farrar prostheses.29 These were probably the well-functioning bearings. Conditions of high wear (edge loading etc.) were usually associated with high frictional torque, and the fixation of the McKee-Farrar implants was not adequate to prevent early loosening and failure. The periprosthetic soft tissues were therefore seldom presented with a significant volume of debris consisting of larger particles of metal.
The biological response to metallic debris is influenced both by the volume of debris and the morphology of the particles.
The design features of MoM resurfacing components that contributed to an increased vulnerability to wear have been alluded to above. However it should be recognised that all large bore MoM bearings are less forgiving of technical errors. In addition resurfacing arthroplasty is a technically challenging procedure. It is therefore of interest that the implant that was released with a 'no train no use' policy has the best results in the national registries!
Most resurfacing devices were extensively tested in simulators in the laboratory. However these regimens did not test true activity of daily living cycles, nor did they test performance under adverse conditions. This has been acknowledged by Fisher et al.30 and new testing protocols have been modified to address these issues. However, the orthopaedic community should by now have learnt of the danger of exporting concepts generated from simulators in the rarefied environment of the laboratory to the highly complex biological system that is the human body. It should be mandatory that there is a critical objective assessment of short- and mid-term clinical outcomes before any new implant is released to the wider patient community.
Hart et al.31 have noted that edge loading was the most important predictor of wear rate, but the majority of retrieved implants did not have excessive edge loading. Microseparation can of course provoke edge loading in well-orientated implants. Vossinakis et al.32 observed that the inclination of the sourcil was a good predictor as to whether a patient would develop supero-lateral arthritis or medial pole arthritis of the hip. This was a function of the joint kinematics and the resultant vectoral force.
A more lateral vectoral force could provoke functional edge loading, and conversely a more vertically orientated cup could be protected from edge loading by a more medially orientated vector.
The XL-THR was developed to address the problem of femoral neck fracture in RA. This allowed only the femoral component to be revised. The incidence of dislocation following conventional THR was reported as 2-3%, and dislocation was identified as the commonest cause of early revision. It appeared that the XL heads (>36 mm) addressed the problem of dislocation, and the technology was enthusiastically embraced by surgeons. The XL bearings were regarded as a 'safety net' against dislocation, and meticulous attention to component placement was neglected - and this with a device that was less forgiving of imperfect technique!
Charnley33 reported an incidence of dislocation of 0.4% using a 22.2 mm head, and felt that even this incidence could be reduced or eliminated by the use of a neck length jig. These outstanding results are attributable to a meticulous and reproducible technique. Companies should not be designing implants to address the technical inadequacies of the surgeon - the focus should be on appropriate instrumentation, technique and training.
No one anticipated the problem of micromotion and instability at the cone taper junction producing fretting and corrosion. Retrospectively I believe it is fair to say that the implications of the reduction in taper size together with the increased torque and bending moments produced by large heads should at least have been considered by our engineering colleagues. The problem has dramatically declared itself clinically, and I fear the reactive research activity is now too little and too late.
MoM bearings have been successfully used in clinical practice, but today the adverse biological reaction to metal debris and the media attention and associated 'hysteria' have resulted in their use being largely abandoned
Langton et al.31 introduced the term ARMD. It is nonspecific and encourages clinicians not to distinguish between the discrete aetiopathogenetic entities that constitute the biological reactions to metallic debris.
The biological response to metallic debris is still poorly understood. The diagnostic entities of 'pseudotumour' and ALVAL have not been clearly defined. Confusion and inconsistencies exist between clinician, radiologist and histopathologist. In some cases there may well be an overlap of diagnostic features. Some findings may be incidental and of no consequence. It has been suggested that ARMD lesions may occur in up to 50% of patients with large bore MoM bearings. Indeed an incidence of 28% at 5 years has been reported with the BHR,35 the best performing RA. Many of these 'lesions' may prove to be normal incidental findings, and more severe lesions only occur in approximately 5% of cases.
Jacobs et al.36 has noted that the biological implications of elevated metal levels in the blood and urine remain the most significant concern about MoM couples. However there is currently no established toxicity threshold for the degradation products of cobalt alloy implants.
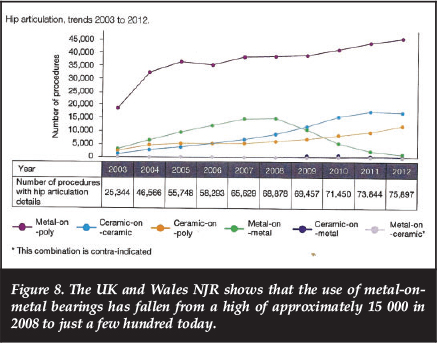
MoM bearings have been successfully used in clinical practice. Today the adverse biological reaction to metal debris, the media attention and associated 'hysteria' have resulted in their use being largely abandoned (Figure 8).
At present this is appropriate. However, we should recognise that it is not just the metal-on-metal bearing that is culpable: the manufacturing companies, our bioengineering colleagues and we, the orthopaedic community, are jointly and severally responsible.
The author is a consultant for De Puy, but no benefits of any form have been or will be received from a commercial party related directly or indirectly to the subject of the article.
References
1. Willert HG, Buchhorn GH, Gobel D, Koster G, Schnaffner S, Schenk R, Semlitsch M. Wear behaviour and histopathology of classic metal-on-metal hip endoprostheses. Clin Ortop Rel Res 1996;329 Suppl:S187-205. [ Links ]
2. Brown SR, Davies WA, DeHeer DH, Swanson AB. Long term survival of McKee Farrar total hip prostheses. Clin Orthop Rel Res 2002 Sept;402:157-63. [ Links ]
3. Jacobsson SA, Djerf K, Wahistrom O. Twenty year results of the McKee Farrar versus the Charnley prosthesis. Clin Orthop Rel Res 1996 Aug;329(Suppl):S60-80. [ Links ]
4. Harris WH. The problem is osteolysis. Clin Orthop Rel Res 1995 Feb;311:46-53. [ Links ]
5. Howie DW, Cambell D, McGee M, Cornish BL. Wagner resurfacing hip arthroplasty. The results of one hundred consecutive arthroplasties after 8-10 years. J Bone Joint Surg Am 1990 Jun;72(5):708-14. [ Links ]
6. Ring PA. Press-fit prosthesis: clinical experience. In: Osteoarthritis and the young adult hip - options for surgical management. Freeman MAR, Reynolds DA (eds). Churchill-Livingstone 1989;220-23. [ Links ]
7. McMinn D, Treacy R, Lin Kyaw, Pynsent P. Metal-on-metal surface replacement of the hip. Experience of the McMinn prosthesis. Clin Orthop Rel Res 329S, August 1996;S89-98. [ Links ]
8. Crowinshield RD, Maloney WJ, Wentz DH, Humphrey SM, Blanchard CR. Biomechanics of large femoral heads: what they do and don't do. Clin Orthop Rel Res 2004 Dec;429:102-107. [ Links ]
9. Stroh DA, Issa K, Johnson AJ, Delanois RE, Mont MA. Reduced dislocation rates and excellent functional outcomes with large diameter femoral heads. J Arthroplasty 2013 Sept;28(8):1415-20. [ Links ]
10. Jacobs JJ. Large (36 or 40mm) femoral heads decreased the rate of dislocation after revision hip arthroplasty. J Bone Joint Surg Am 2012 Nov 21;94(22):2095. [ Links ]
11. McMinn DJ, Daniel J, Ziaee H, Pradhan C. Indications and results of hip resurfacing. Int Orthop 2011 Feb;35(2):231-37. [ Links ]
12. Coulter G, Young DA, Dalziel RE, Shimmin AJ. Birmingham hip resurfacing at a mean of ten years: results from an independent centre. J Bone Joint Surg Br 2012 Mar;94(3):315-21. [ Links ]
13. Bishop NE, Hothan A, Morlock MM. High friction moments in large hard on hard hip replacement bearings in conditions of poor lubrication. J Orthop Res 2013 May;31(5):807-13. [ Links ]
14. Morlock MM, Bishop N, Zustin J, Hahn M, Ruther W, Amling M. Modes of hip failure after hip resurfacing: morphological and wear analysis of 267 retrieval specimens. J Bone Joint Surg Am 2008 Aug;90 Suppl 13:89-95. [ Links ]
15. Leslie IJ, Williams S, Isaac G, Ingham E, Fisher J. High cup angle and microseparation increases the wear of hip surface replacements. Clin Orthop Rel Res 2009;467(9):2259-65. [ Links ]
16. Garbuz DS, Tanzer M, Greidanus NV, Masri BA, Duncan CP. The John Charnley Award: metal-on-metal hip resurfacing versus large diameter head metal-on-metal total hip replacement: a randomized clinical trial. Clin Orthop Rel Res 2010 Feb;468(2):318-2 [ Links ]
17. Long WT, Dastane M, Harris MJ, Wan Z, Dorr LD. Failure of the Durom Metasul acetabular component. Clin Ortop Rel Res 2010 Feb;468(2):400-405. [ Links ]
18. Langton DJ, Sidaginamale R, Lord JK, Nargol AVF, Joyce JT. Taper junction failure in large diameter metal-on-metal bearings. Bone and Joint Research April 2012;1(4):56-63. [ Links ]
19. Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW. Failure rates of stemmed metal-on-metal replacements; analysis of data from the National Joint Registry of England and Wales. Lancet 2012 Mar 31;379(9822):1199-204. [ Links ]
20. Langkamer VJ, Case CP, Heap P, Taylor A, Collins C, Pearse M, Solomon L. Systemic distribution of wear debris after hip replacement. A cause for concern? J Bone Joint Surg Br 1992 Nov;74(6):831-79. [ Links ]
21. Shukla R, Bansal V, Chandhary M, Basu A, Bhonde RR, Sastry M. Biocompatibility of gold nanoparticles and their endocytic fate inside the cellular compartment: a microscopic overview. Langmuir 2005 Nov 8:21(23):10644-54. [ Links ]
22. Trindade MC, Lind M, Sun D, Schurman DJ, Goodman SB, Smith RL. In vitro reaction to orthopaedic biomaterials by macrophages and lymphocytes isolated from patients undergoing revision surgery. Biomaterials 2001 Feb;22(3):253-59. [ Links ]
23. Daley B, Doherty AT, Fairman B, Case CP. Wear debris from hip or knee replacements causing chromosomal damage in human cells in tissue culture. J Bone Joint Surg Br 2004 May;86(4):598-606. [ Links ]
24. Learmonth ID, Case CP. Metallic debris from orthopaedic implants. Lancet 2007 Feb;369(9561):542-44. [ Links ]
25. Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CLM, Ostlere S, Thanasou N, Gill HS, Murray DW. Pseudotumors associated with metal-on-metal hip resurfacing. J Bone Joint Surg (Br) 2008;90-B(7):847-45. [ Links ]
26. Willert H-G, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, Lohman CH. Metal-on-metal bearings and hyper-sensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg 2005;67-A(1):28-36. [ Links ]
27. Davies P, Willert H-G, Campbell PA, Learmonth ID. Case PC. An unusual perivascular lymphocytic infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg 2005 Jan;87(1):18-27. [ Links ]
28. Randelli F, Banci L, D'Anna A, Visentin O, Randelli G. Cementless metal-on-metal total hip arthroplasties at 13 years. J Arthroplasty 2012 Feb;27(2):186-92. [ Links ]
29. Willert H-G, Buchhorn G, Fayyazi A, Lohman C. Histopathological changes around metal/metal joints indicate delayed type hypersensitivity. Preliminary results in 14 cases. Osteologie 2000;9:2-16. [ Links ]
30. Leslie I, Williams S, Isaac G, Hatto P, Ingham E, Fisher J. Wear of surface engineered metal-on-metal bearings for hip prostheses under adverse conditions with the head loading on the rim of the cup. Proc Inst Mech Eng 2013 Apr;2247(4):345-49. [ Links ]
31. Hart AJ, Muirhead-Allwood S, Porter M, Mathies A, Maggiore P, Underwood R, Cann P, Cobb J, Skinner JA. Which factors determine the wear rate of large-diameter metal-on-metal hip replacements? Multivariate analysis of 276 components. J Bone Joint Surg Am 2013 Apr 17;95(8):678-85. [ Links ]
32. Vossinakis LC, Karnezis LA, Parry K, Learmonth ID. Radiographic associations for 'primary' hip osteoarthrosis: a retrospective cohort study of 47 patients. Acta Orthop Scand 2001 Dec;72(6):600-608. [ Links ]
33. Charnley J. In: Low Friction Arthroplasty of the Hip. Springer Verlag 1979 Chapter 19 Post-operative dislocation:314-19. [ Links ]
34. Langton DJ, Jameson S, Joyce T, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large diameter total hip replacement: A consequence of excessive wear. J Bone Joint Surg Br 2010 Jan;92(1):38-46. [ Links ]
35. Bisschop R, Boomsma MF, Van Raay JJ, Tiebosch AT, Maas M, Gerritsma CL. High prevalence of pseudotumor in patients with a Birmingham Hip Resurfacing prosthesis: a prospective cohort study of 129 patients. J Bone Joint Surg Am 2013 Sep;95(17):1554-60. [ Links ]
36. Jacobs JJ, Skipor AK, Campbell PA, Hallab NJ, Urban RM, Amstutz HC. Can metal levels be used to monitor metal-on-metal hip arthroplasties? J Arthroplasty 2004 Dec;19(8Suppl):59-65. [ Links ]
 Correspondence:
Correspondence:
Prof Ian Learmonth
21 Grove Village
37 Stuart Road
7700 Rondebosch
Cape Town
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.














