Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.13 no.2 Centurion abr./ago. 2014
TUMOUR AND INFECTION
Telangiectatic osteosarcoma of the radius: A missed diagnosis case report
Dr T MsithiniI; Prof M LukheleII; Dr Z LindaIII
IMBChB; Registrar, Division of Orthopaedics, University of Witwatersrand
IIMBChB, MMed(Orth), FCS(Orth); Clinical Head of Orthopaedics: Charlotte Maxeke Johannesburg Academic Hospital, University of Witwatersrand
IIIMBChB, FCS(Orth); Head of Tumour and Sepsis Unit, Charlotte Maxeke Academic Hospital, University of Witwatersrand
ABSTRACT
Telangiectatic osteosarcoma is a rare variant of osteosarcoma accounting for 3%-11% of all primary osteosarcomas.1 It has well described distinctive radio-pathological features. Radiographically, these tumours appear as purely lytic destructive lesions located in the metaphyses of long bones. On gross clinical examination, it presents as a soft and cystic mass. Histologically findings are that of aneurysmally dilated spaces lined by osteoid-producing atypical stromal cells. This is a report on a patient with an atypical telangiectatic osteosarcoma which was missed by the primary treating medical team.
Key words: pathologic fracture, telangiectatic osteosarcoma, awareness
Introduction
We present a case of an adolescent female withiectatic osteosarcoma (TOS) of the radius and review the clinical, radiological and pathological features. On reviewing the literature no similar case involving the radius was found.
Case history
A 15-year-old schoolgirl presented to a local hospital with a fracture of the left forearm after a trivial fall. The medical staff made a diagnosis of midshaft radius fracture and the pathological nature of the fracture was overlooked (Figures 1 and 2). They went ahead and performed open reduction and internal fixation (Figure 3). There were no notes on the intra-operative findings on the nature of surrounding soft tissue and quality of bone. Three months later, she presented with swelling and pain of the left forearm. Radiographic examination revealed an extensive lytic destructive lesion of radius. It was at that stage that the patient was referred to our centre.


Physical examination revealed a massively distended forearm with associated epitrochlear and axillary adenopathy (Figure 4). There was no neurovascular deficit or elbow/ wrist involvement clinically. The rest of the physical assessment was unremarkable.

Plain radiographs confirmed an extensively destructive lesion of the radius, with massive soft tissue swelling, soft tissue spicules and failure of fixation (Figure 5).

Laboratory investigations were unremarkable with a slightly raised erythrocyte sedimentation rate (ESR) 15 mm/hr. The haemoglobin level was 12 and liver function test were normal with alkaline phosphatase 101.
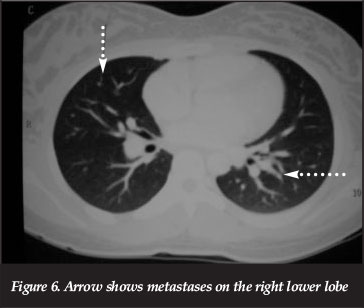
Computerised tomography scan (volumetric CT) of the chest, showed evidence of metastasis to the lungs (Figure 6).
Scintigraphy (Technetium 99m diphosphate scan) revealed an increase uptake in all three phases on left forearm and ribs (Figure 7).
Magnetic resonance imaging had severe artefact as a result of the plate and screws but confirmed the extensive soft tissue involvement. At this stage it was clear that we were dealing with a malignant tumour with metastasis. She was taken to theatre for an open biopsy of the lesion. Intra-operatively, the tumour was found to be pale yellow in colour and highly vascularised with areas of necrosis.
The histopathology was reported by the pathologist to show blood-filled pseudo-cystic spaces surrounded by tumour cells with osteoid deposition and formation of cartilage by malignant cells.
The pathologist made a diagnosis of telangiectatic osteosarcoma with foci of chondroblastic cells. The patient was referred to the paediatric oncology department for neoadjuvant chemotherapy with the plan of performing an amputation. Unfortunately she demised during the chemotherapy courses.
Plain radiographs confirmed an extensively destructive lesion of the radius
Discussion
Telangiectatic osteosarcoma (TOS) was first described by Paget (1854). Gaylord considered these tumours to be malignant aneurysms of bone (1903). Ewing was the first to consider and describe TOS as a variant of osteogenic osteosarcoma.2 TOS is primarily a tumour of long tubular bones with the metaphysis as a site of origin. The incidence varies in different studies from 3%-10%1 There is male predominance with a ratio of 2:1 (males:females) and median age of 17.5 years (15-20 years).
Clinical presentation resembles conventional osteosarcoma, presenting with local pain, soft tissue mass or both. Pathological fractures are an occasional presentation, but have been reported in study as 29% at initial diagnosis or during the course of the disease, compared to 12% for conventional osteosarcoma.3
The risk factors for pathological fractures include large dimensions, diaphyseal location, and progressive loss of bony matrix, osteolytic radiographic pattern, telangiectatic type and prior biopsy.
The metaphyseal region of long bones is the most common location at presentation with the following distribution pattern: distal femur (41.6%), proximal tibia (16.9%), proximal humerus (9.2%), proximal femur (7.7%), mid femur (6.2%), mid humerus (4.6%), mid tibia (3.1%) pelvis (3.1%), fibula (1.5%), skull (1.5%) and ribs(1.5%).4 Extra-osseous TOS has been described in soft tissues.
The aggressive, expansile and osteolytic nature of this tumour is the radiographic hallmark. The dilemma associated with radiological diagnosis of TOS is due to the fact that it is almost indistinguishable from an aneurysmal bone tumour. A combined modality approach with use of strict pathological and radiological criteria is crucial.4
There is a high rate of pathological fracture in patients with TOS.5 Our patient is atypical as our literature search revealed no similar case of TOS being described as occurring in the diaphysis of the radius. The permeative lytic lesions seen in the first X-rays are also atypical unless the TOS was in its early stages. The histological pattern is also atypical in the sense that cartilage formation has not been described in TOS. An argument can be made that the cartilage and osteoid formation is a result of the open reduction and internal fixation of the fracture of the radius. The aggressive nature of the progression of the lesion and its vascularity does simulate TOS.
The lesson to be learned from the initial assessment by the primary doctors is that pathological fractures should always be kept high on the list of possibilities. For a young patient to sustain a fracture of the radius significant force is required. It is therefore important to always take a history of the mechanism of injury. If the force involved turns out to be minor, further history on pre-fracture symptoms must be solicited. In this particular patient a fracture of the radius without an associated fracture of the ulna or disruption of the distal radio-ulna joint should have raised an alarm. This case emphasises the need for continuous professional education on musculoskeletal pathology for primary care providers including community medical officers given that not enough time is allocated to orthopaedics during undergraduate training. At the same time it supports encouraging medical officers at district and provincial hospitals to register and take the Higher Diploma in Orthopaedics already provided by the Colleges of Medicine of South Africa.
Conclusion
It very important to identify pathological fractures at the outset, and then to investigate and manage them appropriately. Clinicians should have a high index of suspicion in atypical mechanisms of injury and relook at the fracture pattern to exclude a pathological fracture.
References
1. Sangle A, Layfield J. Telangiectatic osteosarcoma. Arch Pathol Lab Med. 2012;136:572-76. [ Links ]
2. Yeon-Lim Suh, Je G. Telangiectatic osteosarcoma. Journal of Korean Medical Science 1989;4(2):97-101. [ Links ]
3. Mutsuno T, Unni KK, McLeod RA, Dahlin DC. Telangiectatic osteogenic sarcoma. Cancer 1976;38(6):2538-47. [ Links ]
4. Huvos AG, Rosen G, Bretsky SS, Butler A. Telangiectatic osteogenic sarcoma a clinicopathologic study of 124 patients. Cancer 1982;49(8):1679-89. [ Links ]
5. Weiss A, Khoury J, Hoffer F, WU J, Heck R, Quintana J, Poe D, Rao B, Daw N. Telangiectatic osteosarcoma: The St. Jude Children's Research Hospital's Experience. Cancer 2007;109:1627-37. [ Links ]
 Correspondence:
Correspondence:
Prof M Lukhele
Division of Orthopaedics
Charlotte Maxeke Johannesburg Academic Hospital
University of Witwatersrand
Tel: +27117172038
Email: mkhululi.lukhele@wits.ac.za
The content of this article is the sole work of the authors. The primary author has received a research grant from the South African Orthopaedic Association for research relating to chronic osteomyelitis.
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.














