Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.13 n.2 Centurion Apr./Aug. 2014
FOOT AND ANKLE
Metatarsophalangeal joint instability of the lesser toes: review and surgical technique
James R. Jastifer; Michael J. Coughlin
MD; St Alphonsus Coughlin Foot and Ankle Clinic, Boise, Idaho, USA
ABSTRACT
Metatarsalgia of the lesser toes is commonly caused by metatarsophalangeal (MTP) joint instability. The clinical presentation varies but often includes pain on the plantar aspect of the forefoot that often progresses to the development of coronal and transverse plane malalignment. In some cases, frank MTP joint dislocation can develop. Operative treatment has historically included indirect surgical realignment utilising soft tissue release, soft tissue reefing, tendon transfer, and periarticular osteotomies. An improved understanding of plantar plate tears has recently led to the development of a clinical staging and anatomic grading system that helps guide treatment. A dorsal surgical approach, With the exposure augmented utilising a Weil osteotomy, allows the surgeon to directly access and repaid the plantar plate. Early clinical results suggest that direct plantar plate repair may be a significant advancement in the reconstruction and realignment of lesser MTP joint instability.
Key words: lesser toe instability, crossover toe, plantar plate, MTP instability, forefoot
Introduction
Metatarsalgia is a commonly encountered problem in clinical practice and can have a number of causes (Table I).1-3 First described by Coughlin in 1987,4 the term 'second crossover toe´ was introduced to characterise the clinical deformity. The pathology of the crossover toe, however, does not always include crossing over the hallux. In the early stages of disease it may manifest as a subtle deviation of the toe. Although the second toe was first described and is most commonly involved, deformity in the other lesser toes is also common.1,5-9 Nonetheless, the eponym second crossover toe has been widely accepted and repeatedly used when referring to this pathologic entity. The cause of MTP joint instability is multifactorial, and may have an acute or insidious onset. Newly developed clinical staging and surgical grading systems help to define the magnitude and pattern of plantar plate tears, and assist the clinician in the treatment of MTP joint instability9-12

Importance of the plantar plate
The plantar plate is a stout structure that originates on the metatarsal head just proximal to the metatarsal articular surface and inserts onto the plantar base of the proximal phalanx.2,13,14 Its function is to primarily resist tensile loads in the sagittal plane as well as to provide cushioning to the MTP joint during weight bearing.3,7 Careful dissection of the second MTP joint has shown that the plantar plate is the major stabilising structure of the lesser toe due to its central location and multiple attachments.3,15,16 Instability of the MTP joint, on the other hand, has been linked to the integrity of the plantar plate.1,10,17-20 It has been thought that attenuation and tearing of the plantar plate and collateral ligaments may eventually lead to sagittal and transverse plane instability of the MTP joint.21,22 Pathology in the plantar plate observed in cases of second MTP joint instability has been noted near its insertion at the base of the proximal phalanx.2,10,13,15,17,18,23,24
During normal gait, the MTP joint hyperextends during the terminal stance phase of gait. The plantar plate provides passive resistance, along with the intrinsic musculature (lumbricals and interossei) which provide active resistance, to this dorsiflexion force which propels the body forward. With plantar plate deterioration, the proximal phalanx subluxes dorsally. Additionally, the interossei are displaced dorsal to the axis of rotation of the MTP joint and thus lose their capacity to plantarflex the MTP joint. The lumbrical, located medially, is tethered by the deep metatarsal ligament and becomes a medial deforming force which adds an adduction force vector to the toe causing medial deviation.10,11,14,25 The collateral ligaments are likely to contribute to both transverse and sagittal plane malalignment of the digit.10,26
Based on cadaveric and surgical findings, as well as the reports of other authors,9-11,18,26,27 we believe that plantar plate insufficiency is the primary pathologic finding that leads to this MTP joint instability.
Demographics
MTP joint instability has been associated with a long second metatarsal, acute trauma, chronic inflammation, hallux valgus, hallux varus, pes planus, hallux rigidus, interdigital neuromas, and hammertoe deformities, but the cause may also be insidious and idiopathic.5-7,16,18,19,22,28 These pathologic processes likely alter the loading characteristics of the lesser toes and therefore contribute to instability patterns. While MTP joint instability is frequently seen in older sedentary women, it has been reported in younger male athletes as well.1,16 While an acute disruption of the plantar plate can lead to instability of the lesser MTP joint,19,29,30 more often an insidious and idiopathic onset of symptoms is seen likely resulting from attritional changes which lead to an eventual plantar plate tear.9 A high incidence of lesser MTP joint instability in older females has led some to suggest that the long-term use of high-fashion footwear may lead to chronic hyperextension forces of the MTP joint and eventual plantar plate insufficiency.5,7,9 Although originally described as a deformity of the second MTP joint,4 Nery et at.9 observed in a large series of 55 plantar plate tears (28 patients) that two-thirds of patients had second toe involvement, while a third of patients had third or fourth toe involvement.
We believe that plantar plate insufficiency is the primary pathologic finding that leads to this MTP joint instability
History and physical exam
Determining the primary cause of metatarsalgia can be difficult.31 The most common physical examination finding in patients presenting with plantar plate tears is focal tenderness on the plantar aspect of the forefoot at the base of the second toe. This tenderness may be isolated to the plantar base of the proximal phalanx, where transverse plantar plate tears typically occur. Initially, the swelling associated with the tears may be seen without associated deformity. With time, sagittal and coronal plane deviation develops with continued attenuation of the plantar plate and collateral ligaments. The development of a gap between adjacent toes or medial deviation of a toe is a frequent finding.1,5,10,21 A hyperextension deformity is seen in later stages, and as the deformity progresses the pathologic toe may cross over or under the adjacent digits.16 Chronic pain and malalignment often lead to the development of an associated hammertoe deformity at the proximal interphalangeal joint.3,5
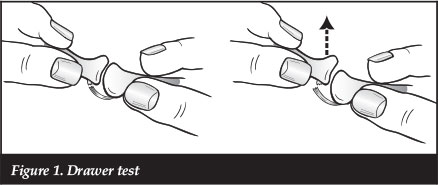
Other clinical findings that may be associated with MTP joint instability include digital swelling, swelling on the plantar aspect of the MTP joint, neuritic symptoms, and MTP joint malalignment.7,9-11,23 The most specific finding is a positive drawer test (80.6% sensitivity, 99.8% specific ).32
Klein et at.32 studied the pre-operative clinical findings and compared them to intra-operative findings. Several key findings were highly sensitive for detecting plantar plate tears including gradual onset of pain (93%), previous first ray surgery (100%, despite an incidence of 18%), pain at the second metatarsal head (98% sensitive), and oedema at the second metatarsal head (95.8% sensitive). Acute onset of pain and toe deformity was rare but telling (7% incidence, 100% specificity).
Some patients may describe radiating pain or numbness into the toes, and this should raise the awareness of a possible adjacent neuroma.33 Coughlin et at.,8 reported the concomitant presence of an interdigital neuroma in patients with lesser MTP joint instability in nearly 20% of the cases. Compression of the transverse metatarsal arch in the presence of joint instability typically does not illicit a 'Mulder click' or numbness and pain radiating into the toes, which can be typical in the presence of an interdigital neuroma.16,33,34 Even so, differentiating a symptomatic interdigital neuroma from an unstable lesser MTP joint can be difficult, especially in the early stages. The use of sequential injections in adjacent MTP joints and intermetatarsal spaces may help lead to an accurate diagnosis.5,16,35
The drawer test is a pathognomonic finding associated with MTP joint instability.9,16,32,36 This test is performed by grasping the proximal phalanx of the involved digit and applying a vertical stress in a dorsal direction. This manoeuvre may reproduce the patient's pain and often the examiner will feel the MTP joint sublux or dislocate (Figure 1). The plantar flexion strength of the digit may be decreased, and this can be quantified by using the 'paper pull-out test'.18 A strip of paper (1 cm x 6 cm) is placed under the affected toe tip. While the patient plantar flexes the affected digit and grasps the paper, the examiner pulls the paper strip out from beneath the toe (Figures 2a and b). A positive test is seen when there is no digital purchase present, and the paper strip is pulled out intact without tearing. These clinical exam findings can be correlated to provide a reliable means for diagnosing plantar plate tears.
Sung et al.37 found a high degree of clinical accuracy in the pre-operative physical exam when later compared to the findings of both advanced imaging and surgery. Evaluation of the magnitude of deformity, and the associated instability on drawer testing allows the clinician to pre-operatively stage the condition on a 0-3 scale (Table II). Staging is a useful tool in predicting the degree of surgical correction necessary at the time of operative intervention.
Imaging studies
Standard anteroposterior and lateral weightbearing radiographs should be used to assess joint congruity, angular deformity, and intra-articular arthritic changes of the foot.16 Common findings include a disruption in the metatarsal parabola of the symptomatic foot, increase in the 1-2 inter-metatarsal angle, medial deviation of the second toe and splaying of the digits.38
Additional imaging modalities should also be considered in evaluating MTP joint pathology. Arthrography of the MTP joints has been used to determine the presence of plantar plate tears, but this is limited in defining the size or pattern of the tear.14,27,39 Yao et al.40 first described the utility of MRI for evaluating a plantar plate tear.
Nery et al.9 and Sung et al.37 reported MRI to be specific and reliable in determining the presence and extent of plantar plate pathology. Ultrasound should be considered but may be limited by the experience of the technologist. While ultrasound and MRI are both appropriate imaging modalities for plantar plate tears, ultrasound is more sensitive than MRI (91.5% versus 73.9%) while MRI is more specific (100% versus 25%).37,41,42 An experienced musculoskeletal radiologist is helpful in assessing the presence and magnitude of tears on MRI. We have found that a 3 tesla MRI can provide excellent visualisation, and we no longer use arthrography to assist in making a diagnosis (Figure 3).
Classification
Several grading schemes for describing second MTP joint instability have been described,14,25,27,43 but only recently has the plantar plate involvement in lesser MTP joint instability been thoroughly evaluated and classified.9-12,20,23,27,44,45
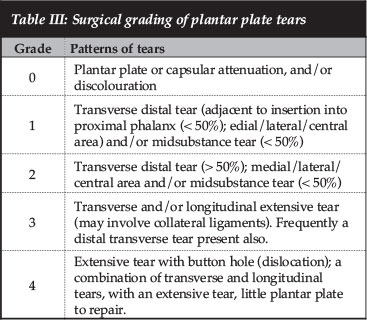
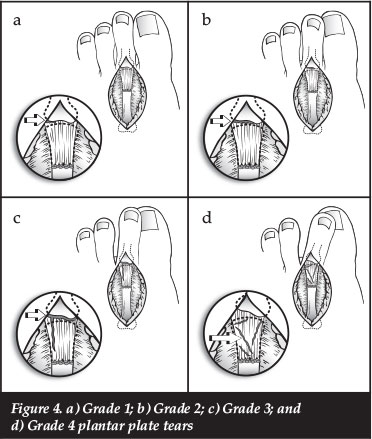
We use two staging systems to guide the treatment of plantar plate dysfunction. First, we use a comprehensive clinical staging system based on physical exam findings which incorporates many of the principles of previous rating systems (Table II).7,9,14,25,27,43 Second, an anatomic grading system been developed based on dissection of cadaveric specimens with plantar plate tears (Table III). These systems address plantar plate dysfunction and are helpful in quantifying the magnitude of the deformity and the pre-operative planning for surgical repair of the specific type of tear. Nery et al.9 reported on a series of 55 plantar plates evaluated arthroscopically prior to open repair, and found that a Grade 3 tear was most common and accounted for almost half of all tears. They used the same grading system described in this article to evaluate these patients (Figures 4a-d).
Conservative treatment
Early detection of plantar plate tears is difficult. Because of the insidious onset of the pain and deformity, delay in the evaluation and treatment is quite common. Frequently, patients become concerned only after progression of the deformity and the presence of a fixed hammertoe.5 The initiation of conservative measures may reduce painful metatarsalgia, but rarely will this alter the progression of symptoms or malalignment.31 There are several conservative treatment options (Figures 5a-d). An alteration in footwear with a reduced heel height and roomy toe box may reduce pressure on the symptomatic digit. A graphite footplate may help diminish stress on the MTP joint in the terminal stance phase of gait.10,35 The footplate can be accompanied by a soft insole with a metatarsal pad placed proximal to the symptomatic metatarsal head to reduce plantar discomfort by redistributing pressure.6,10 A symptomatic hammertoe deformity may be padded with a silicon toe sleeve to reduce pain. Taping the affected toe in the early stages may increase sagittal plane stability, with the goal of position control of the toe while scarring or healing of the tissue occurs. Taping is unsuccessful in cases of complete capsular disruption when the toe is moderately subluxed or dislocated.5

Early detection of plantar plate tears is difficult
Frequently, patients become concerned only after progression of the deformity and the presence of a fixed hammertoe
Coughlin reported on a small series of patients with crossover deformity and found that taping of the digit slowed progression of the deformity but the patients continued to experience joint pain.1,4 Due to the composition of the plantar plate, which is largely type 1 collagen, it is reasonable to expect that a complete tear is unlikely to heal spontaneously with time.20,24,27 Long-term taping can occasionally cause ulceration of the toe or chronic oedema.6
While conservative measures may temporarily relieve the pain of an unstable lesser MTP joint, they will not permanently correct the deformity.4-6 Some clinicians use non-steroidal anti-inflammatory drugs (NSAIDs) to manage discomfort but these should be used with caution, especially in older patient populations. Selective corticosteroid injections may be diagnostic and therapeutic, as described above, but must be used with caution.10,35 Injections can potentially mask symptoms, allowing further capsular and plantar plate degeneration with subsequent joint subluxation or dislocation.6,10 Thus, with increasing pain and deformity associated with capsular instability and plantar plate tears, surgical intervention should be considered.
Surgical technique
The thought process for treating plantar plate tears has progressed through several iterations. Until recently, surgical treatment of lesser toe MTP instability was done indirectly. Some of the treatments included simple synovectomy, soft tissue capsular or tendon release, tendon transfers, and bony decompression.7,14,16,22,43,45,46 Direct plantar plate repair has been reported through a plantar approach;18,27 however, we directly repair the plantar plate through a dorsal approach (Figures 6a and b).2,9,44
While conservative measures may temporarily relieve the pain of an unstable lesser MTP joint, they will not permanently correct the deformity
An approximately 3 cm long dorsal longitudinal incision is made in the adjacent web space of the affected toe. The incision is deepened in the interval between the extensor tendons. The dorsal MTP joint capsule is incised and the medial and lateral collateral ligaments are released at their insertion onto the proximal phalanx. The metatarsal capsular attachments with the associated medial and lateral vascular supply to the metatarsal head are preserved. A Weil metatarsal osteotomy is performed parallel to the plantar aspect of the foot, and the metatarsal head is translated proximally 8 to 10 mm. It is fixed temporarily in a proximal position with a vertical Kirschner wire. The remaining 2-3 mm of the dorsal metaphyseal flare is removed to improve visualisation of the plantar plate. A second vertical Kirschner wire is placed centrally in the proximal phalanx metaphysis. A joint distractor is positioned over the two Kirschner wires and used to open the joint and directly inspect the plantar plate for pathology. The tear type guides the suturing technique.
A distal transverse tear, grade 1 or 2, is repaired with a mechanical suture passer ('Mini-scorpion' © Arthrex, Inc. Naples, FL) by placing one or two horizontal mattress sutures. A longitudinal grade 3 tear is often repaired using a hand-held manual suture passer (suture lasso © Arthrex, Inc. Naples, FL). Following suture placement in the plantar plate, two vertical holes are drilled in the base of the proximal phalanx. The sutures are then passed through the phalangeal drill holes, the Weil osteotomy is fixed into final position, and the sutures are tied over a dorsal bone bridge. If a transverse plane deformity remains, a capsular reefing suture is placed on the convex side of the deformity to achieve further realignment. The drawer test is routinely negative following surgical repair. After a standard closure, a gauze and tape compression dressing is applied. Strengthening, stretching, and range of motion exercises are commenced at 10-14 days post-operatively, and protected weight bearing in a postoperative shoe is continued for 6 weeks after surgery. For those returning to athletic activity, the patients are allowed to commence exercising with full forefoot weight bearing at the sixth post-operative week. A graphite insole with a soft prefab orthotic covering this stiff insole is placed in the athletic shoe to prevent excessive dorsiflexion. This is used for an additional 12 weeks, and is continued in athletes participating in contact sports. Taping of the involved digit is frequently advocated to protect the toe from further injury.
Surgical outcomes
A literature review on the operative treatment of lesser toe MTP joint instability demonstrates that historically an indirect repair of the MTP joint has been performed. This is largely due to the fact that the pathology of plantar plate tear was not well defined, the surgical exposure was difficult, and few surgical instruments were available to achieve repair in such a confined space. The most frequently reported surgical techniques included MTP joint synovectomy,21 capsular soft tissue release with reefing,1,4,6,16,29,43,46 extensor and flexor tendon transfers,1,4,8,14,16,18,25,43,46 phalangeal and metatarsal osteotomies,7,14,25 and even digit amputation.47 Distal metatarsal osteotomies to decompress and realign the involved joint showed unimpressive results.6,7,14,25 None of these surgical techniques addresses the principle cause of MTP joint instability, the plantar plate. The plantar plate, in conjunction with the medial and lateral collateral ligaments-is the key stabilising structure of the MTP joint.4,7-9,11,26,48
Operative techniques have evolved to achieve direct repair of plantar plate tears.9,10,18,24,27,44 In a cadaveric study, Ford et al.45 compared different surgical procedures including primary plantar plate repair- a flexor tendon transfer (FTT), and a combined tendon transfer and plantar plate repair- and concluded that a primary plantar plate repair was a viable alternative to FFT in stabilising the lesser MTP joint. It is intuitive to repair a plantar plate tear through a plantar incision- which has been reported to achieve satisfactory results.18,27 With the plantar approach however, it is difficult to expose adjacent joints and it may also put the patient at risk for a painful plantar scar. Cooper and Coughlin,2 in a cadaveric study- showed that adequate exposure of a lesser MTP joint could be achieved utilising a dorsal approach and a Weil osteotomy. Others9-12-44 have reported satisfactory pain relief and good results of plantar plate repairs done through a dorsal approach using a Weil osteotomy. In a prospective study of a direct plantar plate repair using a dorsal approach-Coughlin et al. and Nery5,9 reported on 22 patients (40 MTP joints) and noted excellent pain relief with improved digital strength and realignment at an average follow-up of 1.5 years.
Since the original description of crossover second toe deformity in 1987,4 there has been an evolution in the evaluation and treatment of lesser toe MTP joint instability. Staging of the deformity based on the clinical examination- and grading of the tear based on surgical findings-helps define the magnitude of the deformity and the severity of the plantar plate tear. After exhausting non-operative treatment- we now treat plantar plate tears with direct surgical repair and advancement with the technique described above. This involves visualisation of the plantar plate through a dorsal approach and primary repair of the tear with non-absorbable suture. We advise any surgeon considering the adoption of this new technique to gain experience in the laboratory setting as it can be technically difficult. Excellent early results have been reported with this surgical technique.
References
1. Coughlin MJ. Second metatarsophalangeal joint instability in the athlete. Foot Ankle, 1993;14(6):309-19. [ Links ]
2. Cooper MT- Coughlin MJ. Sequential dissection for exposure of the second metatarsophalangeal joint. Foot Ankle Int, 2011;32(3):294-99. [ Links ]
3. DuVries HL. Dislocation of the toe. JAMA, 1956;160:728. [ Links ]
4. Coughlin MJ. Crossover second toe deformity. Foot Ankle, 1987;8(1):29-39. [ Links ]
5. Coughlin MJ. When to suspect crossover second toe deformity. J Musculoskeletal Medicine, 1987: p. 39-48. [ Links ]
6. Coughlin MJ. Subluxation and dislocation of the second metatarsophalangeal joint. Orthop Clin North Am, 1989;20(4):535-51. [ Links ]
7. Coughlin MJ. Lesser toe deformities- in Surgery of the Foot and Ankle, MJ Coughlin- CL Mann- CL Saltzman- Editors. 2007-Mosby Elsevier Inc.: Philadelphia- PA. p. 363-464. [ Links ]
8. Coughlin MJ, et al. Concurrent interdigital neuroma and MTP joint instability: long-term results of treatment. Foot Ankle Int, 2002;23(11):1018-25. [ Links ]
9. Nery C- et al. Lesser metatarsophalangeal joint instability: prospective evaluation and repair of plantar plate and capsular insufficiency. Foot Ankle Int, 2012;33(4):301-11. [ Links ]
10. Coughlin MJ- Baumfeld DS- Nery C. Second MTP joint instability: grading of the deformity and description of surgical repair of capsular insufficiency. Phys Sportsmed, 2011;39(3):132-41. [ Links ]
11. Coughlin MJ, et al. Metatarsophalangeal joint pathology in crossover second toe deformity: a cadaveric study. Foot Ankle Int, 2012;33(2):133-40. [ Links ]
12. Weil L, Jr, et al. Anatomic plantar plate repair using the Weil metatarsal osteotomy approach. Foot Ankle Spec, 2011;4(3):145-50. [ Links ]
13. Gregg J, et al. Histologic anatomy of the lesser metatarsophalangeal joint plantar plate. Surg Radiol Anat, 2007;29(2):141-47. [ Links ]
14. Mendicino RW, et al. Predislocation syndrome: a review and retrospective analysis of eight patients. J Foot Ankle Surg, 2001;40(4):214-24. [ Links ]
15. Bhatia D, et al. Anatomical restraints to dislocation of the second metatarsophalangeal joint and assessment of a repair technique. J Bone Joint Surg Am, 1994;76(9):1371-75. [ Links ]
16. Kaz AJ, Coughlin MJ. Crossover second toe: demographics, etiology, and radiographic assessment. Foot Ankle Int, 2007;28(12):1223-37. [ Links ]
17. Borne J, et al. [Plantar plate and second ray syndrome: Normal and pathological US imaging features and proposed US classification]. J Radiol, 2010;91(5 Pt 1):543-48. [ Links ]
18. Bouche RT, Heit EJ. Combined plantar plate and hammertoe repair with flexor digitorum longus tendon transfer for chronic, severe sagittal plane instability of the lesser metatarsopha-langeal joints: preliminary observations. J Foot Ankle Surg, 2008;47(2):125-37. [ Links ]
19. Brunet JA, Tubin S. Traumatic dislocations of the lesser toes. Foot Ankle Int, 1997;18(7):406-11. [ Links ]
20. Deland JT, et al. Anatomy of the plantar plate and its attachments in the lesser metatarsal phalangeal joint. Foot Ankle Int, 1995;16(8):480-86. [ Links ]
21. Mann RA, Mizel MS. Monarticular nontraumatic synovitis of the metatarsophalangeal joint: a new diagnosis? Foot & Ankle, 1985;6(1):18-21. [ Links ]
22. Mann RA, Coughlin MJ. The rheumatoid foot: review of literature and method of treatment. Orthop Rev, 1979;8:105-112. [ Links ]
23. Deland JT, Sung IH. The medial crosssover toe: a cadaveric dissection. Foot Ankle Int, 2000;21(5):375-78. [ Links ]
24. Johnston RB, 3rd, Smith J, Daniels T. The plantar plate of the lesser toes: an anatomical study in human cadavers. Foot Ankle Int, 1994;15(5):276-82. [ Links ]
25. Yu GV, et al. Predislocation syndrome. Progressive subluxation/dislocation of the lesser metatarsophalangeal joint. J Am Podiatr Med Assoc, 2002;92(4):182-99. [ Links ]
26. Barg A, et al. Role of collateral ligaments in metatarsophalangeal stability: a cadaver study. Foot Ankle Int, 2012;33(10):877-82. [ Links ]
27. Powless SH, Elze ME. Metatarsophalangeal joint capsule tears: an analysis by arthrography, a new classification system and surgical management. J Foot Ankle Surg, 2001;40(6):374-89. [ Links ]
28. Morton DJ. Metatarsus atavicus:the identification of a distinctive type of foot disorder. Journal Bone Joint Surgery,1927;9:531-44. [ Links ]
29. Murphy JL. Isolated dorsal dislocation of the second metatar-sophalangeal joint. Foot Ankle, 1980;1(1):30-32. [ Links ]
30. Rao JP, Banzon MT. Irreducible dislocation of the metatar-sophalangeal joints of the foot. Clin Orthop Relat Res,1979;145:224-26. [ Links ]
31. Coughlin MJ. Common causes of pain in the forefoot in adults. J Bone Joint Surg Br, 2000;82(6):781-90. [ Links ]
32. Klein EE, et al. Clinical examination of plantar plate abnormality: a diagnostic perspective. Foot Ankle Int, 2013;34(6):800-804. [ Links ]
33. Coughlin MJ, Pinsonneault T. Operative treatment of inter-digital neuroma. A long-term follow-up study. The Journal of Bone and Joint Surgery (Am), 2001;83-A(9):1321-28. [ Links ]
34. Mulder JD. The causative mechanism in morton's metatarsalgia. The Journal of Bone and Joint Surgery (Br), 1951;33-B(1):94-95. [ Links ]
35. Trepman E, Yeo SJ. Nonoperative treatment of metatarsopha-langeal joint synovitis. Foot Ankle Int, 1995;16(12):771-77. [ Links ]
36. Thompson FM, Hamilton WG. Problems of the second metatar- sophalangeal joint. Orthopedics, 1987;10(1):83-89. [ Links ]
37. Sung W, et al. Diagnosis of plantar plate injury by magnetic resonance imaging with reference to intraoperative findings. J Foot Ankle Surg, 2012;51(5):570-74. [ Links ]
38. Klein EE, et al. The underlying osseous deformity in plantar plate tears: a radiographic analysis. Foot Ankle Spec, 2013;6(2):108-18. [ Links ]
39. Blitz NM, Ford LA, Christensen JC. Second metatarsopha-langeal joint arthrography: a cadaveric correlation study. J Foot Ankle Surg, 2004;43(4):231-40. [ Links ]
40. Yao L, et al. Magnetic resonance imaging of plantar plate rupture. Foot Ankle Int, 1996;17(1):33-36. [ Links ]
41. Klein EE, et al. Musculoskeletal ultrasound for preoperative imaging of the plantar plate: a prospective analysis. Foot Ankle Spec, 2013;6(3):196-200. [ Links ]
42. Klein EE, et al. Magnetic resonance imaging versus musculoskeletal ultrasound for identification and localization of plantar plate tears. Foot Ankle Spec, 2012;5(6):359-65. [ Links ]
43. Haddad SL, et al. Results of flexor-to-extensor and extensor brevis tendon transfer for correction of the crossover second toe deformity. Foot Ankle Int, 1999;20(12):781-88. [ Links ]
44. Gregg J, et al. Plantar plate repair and Weil osteotomy for metatarsophalangeal joint instability. Foot Ankle Surg, 2007;13(3):116-21. [ Links ]
45. Ford LA, Collins KB, Christensen JC. Stabilization of the subluxed second metatarsophalangeal joint: flexor tendon transfer versus primary repair of the plantar plate. J Foot Ankle Surg, 1998;37(3):217-22. [ Links ]
46. Myerson MS, Jung HG. The role of toe flexor-to-extensor transfer in correcting metatarsophalangeal joint instability of the second toe. Foot Ankle Int, 2005;26(9):675-79. [ Links ]
47. Gallentine JW, DeOrio JK. Removal of the second toe for severe hammertoe deformity in elderly patients. Foot Ankle Int, 2005;26(5):353-58. [ Links ]
48. Sarrafian SK, Topouzian LK. Anatomy and physiology of the extensor apparatus of the toes. J Bone Joint Surg Am, 1969;51(4):669-79. [ Links ]
 Correspondence:
Correspondence:
James R. Jastifer MD
Saint Alphonsus Coughlin Foot & Ankle Clinic
1075 North Curtis Road Suite 300, Boise
ID 83706
Tel: (616)-481-8151
Email: jastifermd@gmail.com
No benefits were received for the publication of this manuscript.
This paper is our original unpublished work and it has not been submitted to any other journal for reviews.
(All figures and tables reproduced with permission from Michael J. Coughlin MD)
This article is also available online on the SAOA website (www.saoa.org.za) and the SciELO website (www.scielo.org.za). Follow the directions on the Contents page of this journal to access it.
















