Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.13 no.1 Centurion Jan./Mar. 2014
EXPERT OPINION ON PUBLISHED ARTICLES
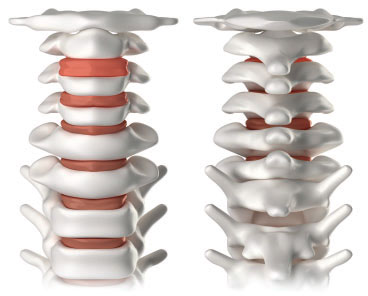
Early morbidity of multilevel anterior cervical discectomy and fusion with plating for spondylosis: Does the number of levels influence early complications? A single surgeon's experience in 519 consecutive patients
Reviewer: Dr SJ Mabusha
Spinal Unit Department of Orthopaedic Surgery University of KwaZulu-Natal King Dinuzulu Hospital Tel: 031 240 4393
Dennis E Bullard, Jillian S Valentine
Evidence-Based Spine-Care Journal, April 2013;4(1):13-17
Cervical spondylosis is nearly a ubiquitous process that develops as patients age. Cervical neck pain can present with radiculopathy, myelopathy and/or myeloradicu-lopathy. The prognosis is often good for patients with radiculopathy and the need for surgery might be obviated. In the majority of patients who present with axial neck pain, symptoms will be benign and self-limited, usually resolving in six to eight weeks. Urgent red-flag diagnoses, such as infection, trauma and tumours must be ruled out.
The study by Bullard et al enrolled a huge number of cases and all surgeries were performed by a single surgeon using a uniform technique. Their main study objective was to evaluate within clinical practice evidence-based results of short-term morbidity with a multi-level anterior cervical discectomy and fusion with plating. The discectomy was always performed using the surgical microscope. Standard constructs were employed: structural allografts or cages filled with biologic material with anterior plating.
Early morbidity was measured by peri-operative complications: length of hospital stay, pain assessments, hardware failure and return to work status was evaluated for 1-, 2-, 3-, and 4-level ACDFP during the first three months after surgery. The 90-day review period is used as a hallmark for assessment of surgically related complications, healing and reoperations. Early functional recovery is assessed by 24 months, and long-term quality of life and health utilisation studies are determined by 5 years and more.
The author recommends strict patient selection criteria. Patients were excluded for traumatic injuries, chronic steroid use, chronic dialysis, and rheumatoid arthritis. The following types of comorbidities were documented: smoking, hypertension, obesity and diabetes mellitus. Spine surgeons should put high premiums on other comorbidities such as sleep apnoea, COPD, pre-operative steroid use, osteoporosis, use of steroids and NSAIDs. These factors may greatly affect the patient's outcome.
Results
The most common complication across all four ACDFP levels was swallowing/speech dysfunction, followed by uncontrolled pain, then haematoma and reoperation (n=2). There were no reported infections, hospital readmissions, or instances of hardware failure.
The author's summary and conclusions:
1. Multilevel ACDFP can be performed with minimal initial morbidity in a group of generally healthy patients.
2. To their knowledge, their patient database is the largest group reported on in the literature.
3. Transient increase in dysfunction in 3- and 4-level ACDFP, but none of the increases were statistically significant other than for hospital stay for 3- and 4-level ACDFP and return to work for 4-level ACDFP.
I am impressed by this paper. It reveals the fact that multilevel corpectomies with their inherent complications can be avoided. There is minimal blood loss and short operation time with multilevel discectomies. Vertebral artery and recurrent laryngeal nerve injuries are less common. The approach is done through the Smith-Robinson approach. This study is an excellent start with a very large and homogenous-appearing study population. The authors can continue their data collection and present their 2-year follow-up study.
Gastrocnemius recession for chronic noninsertional Achilles tendinopathy
Reviewer: Dr G McCollum
Foot and Ankle Reconstruction Unit Groote Schuur Hospital University of Cape Town
NJ Kiewit, SM Holthausen, DR Bohay, JG Anderson Foot Ankle Int. 2013;34(4);481-85
This article reviews a series of patients undergoing treatment of a clinical problem that is frustrating for both patients and treating surgeons alike. Chronic Achilles tendinopathy responds to conservative and rehabilitative treatments in the majority of cases but can be resistant. For these, surgery may play a role, usually involving debridement and resection of diseased tendon with or without some form of reconstruction. The outcomes reported are fairly good in most papers, but the complication rate is high and time to return to function lengthy.
The authors, D Bohay and J Anderson (who presented the paper at the recent South African Foot congress in 2013) reviewed the results of a series of patients undergoing a gastrocnemius recession for resistant Achilles tendinopathy.
The surgical technique involves a posteromedial or posterior incision just distal to the musculotendinous junction of the gastrocnemius. After opening the facia, the gastrocnemius tendon was exposed and cut transversely while protecting the sural nerve. Neither the tendon nor the facia was repaired. The patients remained in a boot, weight bearing for the first 2 weeks, after which they returned to normal shoe wear and daily activities.
Twelve patients underwent the procedure, of which seven were available for clinical follow-up at a mean of 34 months. One of the patients had a telephonic interview and scoring as they had moved state. Of the four patients who were lost to follow-up, clinical notes showed that three demonstrated significant improvement in clinical function and pain at a mean of 5.4 months.
The VAS score improved from 7.3 to 1.0 and five of the seven patients were able to perform multiple single leg heel raises. Calf circumference was equivocal to the non-operated side. The mean AOFAS hindfoot score was 94.4 (75-100).
The clinical results were then compared to Achilles debridement with FHL transfer pooled from previously published data. On average the AOFAS scores were significantly higher in the Gastroc recession group at the same time post surgery. The SF36 scores were not significantly different.
There were no wound complications, infections, DVTs or nerve injuries.
Although the sample size is small and the follow-up not inclusive it does present an elegant, minimally invasive way of treating these patients without having to perform a major operation. The authors are following on from a case report published in their unit in 20081 demonstrating healing of noninsertional tendinopathy after gastrocnemius recession and MRI-confirmed resolution of intra-tendinous signal change. Gastrocnemius contracture is thought to be a driver of many forefoot and hindfoot problems and it seems a logical procedure if eccentric stretching is the main form of conservative treatment. The procedure is simple with a low incidence of complications and bridges are not burnt. If the disease is resistant to the surgery, later debridement and reconstruction is not compromised.
This small study needs to be expanded upon and prospective trials undertaken to see if this is not just a 'flash in the pan' or 'flavour of the month' but it certainly seems to be an attractive way of treating a difficult problem.
There were two other shortcomings of the paper, besides the small cohort and poor follow-up. The authors failed to compare the post-operative calf strength with pre-operative and with the contralateral side, and they did not mention if the patients had a gastrocnemius contraction pre-surgery, as demonstrated by a positive Silfverskiold test.
Reference
1. Gentchos CE, Bohay DR, Anderson JG. Gastrocnemius recession as the treatment for refractory Achilles tendinopathy: a case report. Foot Ankle Int. 2008;29(6):620-23.
Surgical versus non-surgical treatment of acute Achilles tendon rupture. A meta-analysis of randomized trials
Reviewer: Dr S Sombili
Department of Orthopaedics Steve Biko Academic Hospital University of Pretoria
Alexandra Soroceanu, Feroze Sidhwa, Shahram Arabi, Annette Kaufman, Mark Glazebrook Investigation performed at University Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada Journal of Bone and Joint Surgery, December 2012;94-A(23)
The non-surgical treatment of acute Achilles tendon ruptures remains controversial because of the high incidence of re-rupture rates. Surgical treatment of acute Achilles tendon ruptures remains a common method of treatment for most orthopaedic surgeons.
In this interesting study a meta-analysis of ten randomised controlled trials of the treatment of acute Achilles tendon ruptures was done. The aim of the study was to compare surgical treatment with regard to the re-rupture rate, the overall rate of other complications like return to work, calf circumference and functional outcomes.
The study revealed that if early functional rehabilitation in the conservative group was employed, the re-rupture rates were the same for non-surgical and surgical patients. The absolute risk reduction achieved by surgery was 8.8% if early range of motion was not employed in the conservative group.
Surgery was associated with an absolute risk increase of 15.8% for complications other than re-rupture. These complications include deep infection, skin necrosis, tendon necrosis and a draining sinus.
The only benefit of surgery in this meta-analysis was return to work which was 19.16 days earlier than the non-surgical group. There was no significant difference between the two treatments with regard to calf circumference or functional outcomes.
The study concluded that conservative treatment of acute Achilles tendon ruptures should be considered in those centres that use early functional rehabilitation. This results in re-rupture rates similar to the surgical treatment of the acute Achilles tendon ruptures. What I also learned from this article was an indication for an ultrasonography or MRI in acute Achilles tendon ruptures.
The musculoskeletal effects of cigarette smoking
Reviewer: MN Rasool
Department of Orthopaedics University of KwaZulu-Natal Tel: (031) 260 4297
JJ Lee, R Patel, JS Biermann, PJ Dougherty JBJS 2013;95A:850-59
This concept review highlights the effects of cigarette smoking on the musculoskeletal system and emphasises the benefits of cessation pre- and post-operatively. The harmful effects of smoking on the lung and vascular system are well known but the effects on the musculoskeletal system are not emphasised. The authors have referenced 187 articles.
Research has shown that cigarette smoke consists of two phases: a volatile phase of nearly 500 gases and a particulate phase of ± 3 500 chemicals. Nicotine has numerous physiological effects, including vascular disturbance and cell death. The nicotine metabolite cotinine is often used to assess recent cigarette smoking and is detected in urine.
Smoking is hypothesised as being a cause of osteonecrosis because of its effects on the haematological system. Nicotine and carbon monoxide cause endothelial damage, decrease microperfusion and polycythaemia, and increase blood viscosity, resulting in microclotting. A four-fold increased risk of development of osteonecrosis of the femoral head in smokers has been reported as well as passive smoking and the development of Perthes' disease in children has been reported. Significantly lower bone marrow density (BMD) has been found in smokers. This is due to inhibition of function of osteoblast activity. Osteoclast function is increased. There is also a decrease in calcium absorption in smokers. Female smokers enter menopause two years earlier than non-smokers. Osteocalcin secreted by osteoblasts, used as a marker for bone formation, is decreased in post-menopausal female smokers.
Studies conducted in Brazil and England have shown an increase rate of fractures of the hip, spine and distal radius in smokers. The patients were mainly male and younger than non-smokers. The deleterious effects on BMD were also shown in young adults (18 to 20 years of age). Reduction in peak bone mass made them more prone to injury. This is also related to lifestyle habits in young smokers, such as lower calcium intake, decreased activity and appetite. Smoking has been associated with delayed fracture union, non-union, infection and poor wound healing in various studies quoted in the review. These problems are associated with open reduction of proximal humeral fractures and calcaneal fractures, open and closed reduction of ankle and tibial fractures, and also with the Ilizarov technique. A new serum marker for fracture healing transforming growth factor beta (TGFBI) is found to be decreased at four weeks after injury in smokers. Pseudarthrosis is more common with spinal fusion in smokers.

Backache and degenerative disc disease is also more common. Tendon and ligament healing are also found to be negatively affected by smoking. Larger tears of the rotator cuff have been found in smokers.
Some studies have shown increased knee cartilage loss in smokers. Smoking is known to be a risk factor for rheumatoid arthritis. These patients are less responsive to treatment.
Poor wound healing is described in smokers due to alteration of fibroblasts, mesenchymal stem cells and growth factors that are important in the formation of granulation tissue. Nicotine causes increase in chalones, which inhibit epithelialisation. Cigarette smoke creates numerous radicals that result in cellular damage. Cigarette smoking also has a detrimental effect on the immune system. Smokers are more prone to infection due to decreased white cell counts, serum levels of immunoglobulins, T-cell and antibody response. Lymphoid tissue mass is also decreased. However, important facts from the review show that the effects of smoking on the skeleton may be at least partially reversible. Immune function, wound healing and pulmonary function appear to recover in four to eight weeks after abstinence; former smokers have been found to have lower fracture risk than current smokers. They also had improved outcomes with regard to systematic post-operative complications, infection, return to work and recovery rates.
Orthopaedic surgeons should encourage all patients who are contemplating elective procedures to quit smoking four to six weeks in advance of the proposed procedure and advise them of the serious negative outcomes associated with active smoking in the peri-operative period. Informed consent should include notification of the higher risk of peri-operative complications with cigarette smoking and the benefits of temporary cessation. A urine cotinine test can be used to monitor smoking.
Safety and efficacy of denosumab for adults and skeletally adolescents with giant cell tumour of bone: interim analysis of an open-label, parallel-group, phase 2 study
Reviewer: Dr LC Marais
Tumour, Sepsis and Reconstruction Unit Department of Orthopaedic Surgery University of KwaZulu-Natal Grey's Hospital Pietermaritzburg Tel: (033) 897 3424 Leonard.Marais@kznh.ealth.gov.za
S Chawla, R Henshaw, L Seeger, E Choy, J Ferrari, J Kroep, R Grimer, P Reichardt, P Rutkowski, S Schuetze, K Skubitz, A Staddon, D Thomas, Y Qian, I Jacobs The Lancet Oncology 2013;14(9):901-908. doi:10.1016/S1470-2045(13)70277-8.
The contemporary surgical modalities utilised in the management of giant cell tumours, including extended curettage (including the use of a high speed burr to extend the resection margins), local adjuvant therapy, PMMA bone cement and internal fixation, have enhanced our ability to achieve cure. Although recurrence rates as low as 10% have been reported with these techniques, others found much higher rates, as high as 30% in some studies. Giant cells tumours may also be complicated by metastases (in up to 4% of cases) and pathological fracture occurs in approximately 30% of cases. Furthermore, the location of certain tumours (in the sacrum or pelvis, for example) may make surgical management impossible.
Typically giant cell tumours occur in the epiphyseal regions of long bones and these locally aggressive lesions frequently cause significant destruction of periarticular bone. As a result intrale-sional excision is not always feasible and en bloc resection combined with endo-prosthetic replacement has been advocated in the setting of severe bone loss or pathological fractures. In a recent multicentre study, Van der Heijden et al., compared the outcomes of curettage combined with local adjuvants with resection and endoprosthetic replacement of giant cell tumours associated with pathological fractures. They found that although local recurrence was drastically reduced by resection (0% versus 30% in the curettage and local adjuvant group), complications were significantly increased in the resection group (16% versus 4%). Furthermore, at a mean of 101 months, the mean Musculoskeletal Tumour Society (MSTS) score was higher following curettage and local adjuvants than after resection and replacement. They concluded that resection and replacement should only be considered in cases with soft tissue extension, when there is a fracture through local recurrence or when structural integrity cannot be achieved with reconstruction. This study unfortunately did not look at the incidence of late arthritic changes (a known complication) but still recommended that all attempts be made to try and salvage the native joint.
This move towards joint maintenance, the fact that certain cell tumours are inoperable and the high recurrence rate of aggressive lesions have created considerable interest around the use of adjuvant therapy for giant cell tumours. Balke et al., for example, utilised osteoclast inhibition through bisphosphonate therapy in the management of complicated giant cells tumours. They found that inoperable tumours did not increase in size and also noted no post-operative recurrence with the use of intravenous bisphosphonates.
In the study of interest, Chawla et al., investigated the use of denosumab in the management of giant cell tumours. Denosumab is a human monoclonal antibody that specifically inhibits normal and tumour-associated bone lysis by preventing RANKL-mediated formation and activation of multinucleated osteoclasts or giant cells from RANK-positive mononuclear pre-osteoclasts and macrophages. A previous report, by Branstetter et al., showed that denosumab resulted in a 90% decrease in tumour giant cells, as well as replacement of proliferative RANKL-positive stromal cells with dense fibro-osseous tissue and/ or new woven bone. In this multicentre, phase 2 study, the primary aim was to investigate the safety profile of denosumab. Of the 282 patients enrolled, 9% experienced serious side effects including hypocalcaemia (5%), hypophosphatemia (3%), osteonecrosis of the jaw (1%), anaemia and back or extremity pain. More interesting, however, was the analysis of the response to treatment in two subsets of patients. In the first cohort of 169 patients with inoperable tumours, 96% of cases had no disease progression after a median of 13 months. In the second cohort of 100 patients, 74% of patients did not require surgery and 62% of patients who did have surgery underwent a less morbid procedure than planned.
These results are certainly promising, in terms of adjuvant and palliative therapy for giant cell tumours. Certain issues however still need to be resolved. Although denosumab has been approved by the FDA for the management of inoperable tumours, what is the role in the pre- and post-operative setting? How does denosumab compare with bisphosphonates? We assume it will be better because it inhibits both osteoclasts and proliferating stromal cells. Finally, pathological fractures related to the use of denosumab in the management of osteoporosis have been reported. What will the optimal duration of treatment be and what will happen when we stop treatment?














