Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.13 n.1 Centurion Jan./Mar. 2014
HIP
Uncemented primary total hip arthroplasty in patients aged 55 years or younger: Results at a minimum of 5 years in a consecutive series
P RyanI; Prof IE GogaII
IFCS Orth(SA). Consultant Orthopaedic Surgeon
IIMD, FRCS(Edinburgh), FCS Orth(SA). Head of Department: Orthopaedic Surgery Inkosi Albert Luthuli Central Hospital, Durban, KwaZulu-Natal, South Africa
ABSTRACT
INTRODUCTION: Surgical management of younger patients requiring primary total hip arthroplasty is challenging due to increased activity levels, physical demands, and the need for longevity of implanted components. There is debate regarding the most suitable component type, and the optimal fixation, should a stemmed component be utilised.
MATERIALS AND METHODS: We retrospectively reviewed a sequential group of patients, aged 55 years or younger at the time of surgery, who underwent uncemented primary total hip arthroplasty, and are currently at a minimum of 5 years post operation. Eighty-eight primary uncemented total hip replacements were performed between January 2004 and December 2006.
The patient ages ranged from 18 to 55 years with a mean of 43.1 years at time of operation. At last review, eight patients (ten hips) had demised of unrelated causes and 16 patients (20 hips) were lost before completing 5 years of follow-up.
RESULTS: Complications included one peri-operative mortality, ten intra-operative femoral calcar fractures, two revisions for sepsis, one dislocation and one deep vein thrombosis. All stems achieved bony fixation as per Engh's criteria. At a minimum of 5 years post operation, there were no revisions for aseptic loosening.
CONCLUSION: We present our radiological results, complications, and survivorship of uncemented primary total hip replacements in patients 55 years or younger.
Key words: total hip arthroplasty, uncemented hip, young patient, hip replacement.
Introduction
Total hip arthroplasty is effective in the management of patients with advanced hip joint disease of variety of aetiologies. Surgical management of the younger patient requiring arthroplasty remains challenging due to their increased activity levels, physical demands, and the need for longevity of implanted components.
High rates of failure of cemented implants in this young, active patient group led to an expanding interest in uncemented hip arthroplasty.1 The results of first generation uncemented, and some of the second generation uncemented implants have been unacceptably poor.2
Other second generation femoral components, both porous and hydroxyapatite-coated, have yielded excellent long-term results, with survivorships of up to 96.8% at 20 years.3
However, concerns remain regarding the acetabular side, with high rates of liner wear, osteolysis and revision of sockets in certain implant types.4-7
Resurfacing arthroplasty appeared to be a good solution for the young active patient, providing greater range of motion with the large heads, and bone conservation allowing for easier revision when required. Due to recent concerns regarding metal debris and pseudo-tumour formation, large bearing metal-on-metal replacements, including resurfacing, are being employed less frequently. There is renewed interest in stemmed prostheses, and continued debate on component fixation.
With this in mind, we retrospectively reviewed a cohort of patients who underwent uncemented total hip arthro-plasty, were 55 years or younger at the time of surgery, and who were at a minimum of 5 years post operation at the time of analysis. The aims were to evaluate the radiographic outcomes, the early and late complications, and the need for revision surgery.
Materials and methods
We performed a retrospective chart and radiographic review. Patient notes were canvassed for demographic and operative details, as well as details regarding early or late complications, or revision surgery. Radiographs were evaluated as described below.
Between January 2004 and December 2006, 88 primary uncemented total hip replacements were performed in 72 adults under the age of 55 years. The cohort included 37 men and 35 women, with a mean age 43.1 years (range 18 to 55 years). At time of analysis, eight of the 72 patients had demised and 16 were lost before 5 years of follow-up, leaving 59 hips in 48 patients.
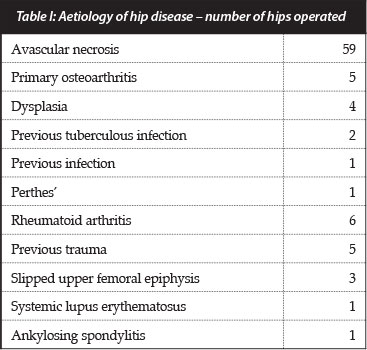
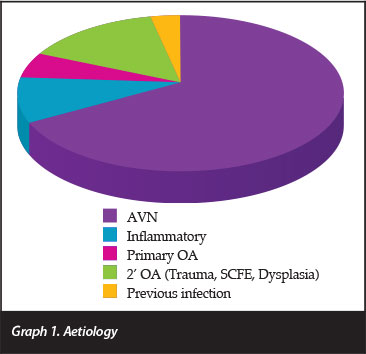
The aetiology (Table I and Graph 1) was avascular necrosis (AVN) in 59 hips (67%) and inflammatory in eight (9%). Twenty-six arthroplasties were done on the right hips, 30 on the left, and 16 bilaterally.
As the surgeries were performed in an academic training hospital, they were done by a number of surgeons. The antero-lateral approach was utilised in 69 hips, the posterior in 18.
The femoral component was a collarless, fully hydroxyap-atite-coated, press-fit stem (Corail, De Puy International Ltd) in 77 of the 88 hips; a tapered proximally coated stem in nine (Summit, De Puy International Ltd); a cementless, proximally porous-coated tapered stem in one (Synergy, Smith And Nephew); and a tapered grit-blasted stem in one (CLS Zimmer).
The acetabular component was a hemispherical or sub-hemispherical, porous-coated press-fit in all cases: Pinnacle 300 or Duraloc 300 in 80; Pinnacle Sector or Duraloc 1200 in six (De Puy International LTD); Reflection in one (Smith and Nephew); and Durom in one (Zimmer).
The bearing surface was metal-on-polyethylene (Marathon ultra-high molecular weight, moderately cross linked polyethylene, De Puy International LTD) in 67 and metal-on-metal (MOM) in 21. The head size was 28 mm in all the metal-on-UHMWPE, and in the MOM articulations it was 36 mm in 16, 28 mm in three, 32 mm in one and 38 mm in one. The use of metal-on-metal articulations was abandoned by the unit in 2007 due to concerns raised in the literature. The current unit protocol is the use of ceramic-on-ceramic articulations for this age group.
All patients received peri-operative antibiotics and thrombo-prophylaxis as per protocol, and were mobilised on day one/two post-operatively - partial weight bearing initially, with progression to full weight bearing as tolerated.
The initial post-operative X-ray was an antero-posterior view of the pelvis, centred over the pubis, including the most distal aspect of the femoral component. The 6-week X-rays included a repeat of the above view, as well as a lateral view which included the acetabular component and the distal tip of the femoral component. These served as reference for follow-up films.
X-rays
One surgeon, not involved in the index surgeries, independently evaluated the early post-operative and most recently available radiographs. The anteroposterior radiograph taken in the early post-operative period, and the antero-posterior and lateral radiographs taken at the 6-week follow-up were used as the baseline for further comparisons. Linear and angular measurements were taken using Siemens Magicweb software, and magnification errors were accounted for.
The following radiographic assessments were made:
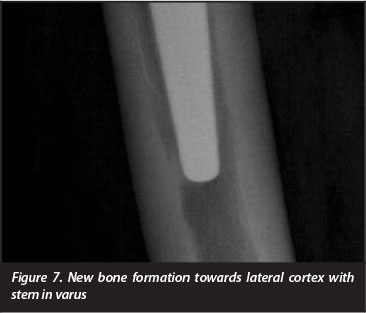
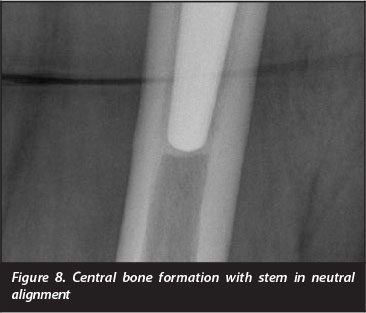
1. Femoral component alignment classified as valgus (tip engaging the medial cortex), neutral or varus (tip engaging the lateral femoral cortex)
2. Femoral component subsidence as defined by a change of more than 3 mm of the distance from the superolateral aspect of the femoral stem to the tip of the greater trochanter8
3. Femoral zonal analysis as per Gruen et at9
4. Femoral stress shielding as per Engh et al10
5. Femoral component fixation and stability classified as: bone ingrowth, stable fibrous or unstable according to the criteria of Engh et al10
6. Femoral bone remodelling: calcar resorption, reactive bone formation or cortical hypertrophy
7. Acetabular component alignment
8. Acetabular migration as defined by a linear change of 3 mm or a rotational change of 8° or greater11
9. Acetabular zonal analysis as per DeLee and Charnley12
10. Acetabular loosening defined as a change in position of the component or a continuous circumferential radiolucent line >2 mm on AP and lateral radiographs
11. Presence of periacetabular or femoral osteolysis
12. Heterotopic ossification graded according to Brooker et al13
Results
Patients
At a minimum of 5 years post hip replacement, eight patients (ten hips) had demised, at an average of 3.3 years post operation. Three of these patients had AVN secondary to chronic alcohol abuse, one of them died from liver failure, and the other two (both smokers) suffered acute myocardial events. Two patients had AVN secondary to systemic conditions (SLE and sarcoidosis respectively) and demised from complications of their underlying disease. One patient died from complications related to advanced immune-compromise secondary to HIV infection, one died in a motor vehicle accident, and in the last the cause of death is unknown.
At time of last clinical review, none had required nor were planned for reoperation.
Seventeen patients (21 hips) were lost to follow-up. This was at an average of 18 months (range 0.5 to 36) post surgery. At time of last review, none had required further intervention.
Forty-seven patients (57 hips) had completed 5-year clinical follow-up (average 77.5 months post-operative).
Complications
Intra-operative complications included iatrogenic femoral calcar fractures in ten hips (11.4%). Three required fixation with Charnley wiring. All of these fractures occurred during the insertion of Corail stems, and all healed uneventfully without any implant subsidence.
One patient suffered an acute myocardial event intra-operatively and demised in the early post-operative period. The patient was a 55-year-old male whose only pre-operative identified risk factor for ischaemic heart disease was a 20 pack/year smoking history. There was no excessive intra-operative blood loss.
There was one clinically evident deep vein thrombosis (DVT) which resolved with pharmacological therapy and without long-term sequelae. It is not the unit policy to actively screen asymptomatic post-operative patients for DVTs with either Doppler ultrasound or venography.
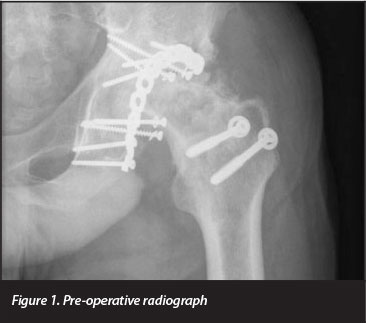
One hip (Figures 1 to 3) dislocated on the second post-surgical day. The indication for arthroplasty was Steinberg stage 6 avascular necrosis. The AVN was a consequence of open reduction and posterior column fixation performed for a fracture-dislocation 3 years prior. Pre-operatively the patient was noted to have fixed flexion and external rotation deformities of 50° and 20° respectively. The hip replacement was done through a posterior approach, extensive scarring was encountered, which required significant release. The dislocation was managed by closed manipulation and immobilisation in an abduction cast. The patient later developed Brooker grade 3 heterotopic ossification and chronic moderately severe pain. One patient had a transient sciatic nerve palsy, which recovered fully.


Superficial wound infections developed in two hips. These settled on dressings and short courses of oral antibiotic therapy.
There were two cases of deep infection. The first patient, a 34-year-old male smoker, presented 5 months post replacement with peri-prosthetic infection. A cloxacillin sensitive Staphylococcus aureus was grown on culture, and he was managed successfully with a two-stage revision.
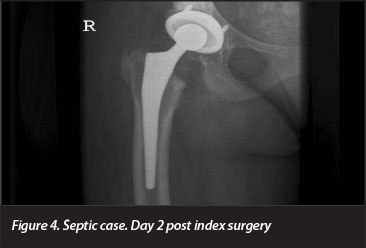
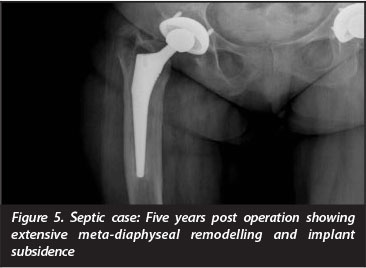
The second patient developed clinical symptoms and elevated inflammatory markers 5 years post hip replacement. Radiographically, on the acetabular side the gaps initially seen in zones 1 and 2 had disappeared, but in zone 2 an area of washout, typical of sepsis, was noted. The femur had undergone extensive meta-diaphyseal remodelling and the femoral component had subsided (Figures 4 and 5). The patient has since been diagnosed with HIV infection (CD4 of 53), and has been started on antiretroviral therapy. Her prosthesis has been removed, and she awaits the second stage of her revision. Microbiological specimens taken at the first stage revealed a cloxacillin-sensitive Staphylococcus aureus.
Revisions
Apart from the above revisions for deep sepsis, there were no further revisions.
Radiographic outcomes
Of the 57 hips that had completed 5 years of clinical review, three hips had less than 4 years of radiological follow-up, and two had been revised for deep infection. These were excluded from radiological analysis. Of the remaining 52 hips, the average length of radiological follow-up was 73.6 months (range 49 to 93).
The femoral component was neutral in 47 (90%), varus in three (6%) and valgus in two (4%). There was one case of subsidence. In the single case in which a Synergy stem was used, the component was noted on the 6-week postoperative visit to have subsided 15 mm. At last radiograph, 68 months later, the position had remained unchanged and there were no other radiographic features of loosening. On review, the femoral component was noted to be relatively undersized, leading to the initial subsidence.
Radiographic double line formation in zone 1 was demonstrated in 27 hips (52%), and in zones 1 and 7 in three (6%) hips. Twenty-three hips (44%) had femoral cortical thickening and 42 of the 52 (81%) had developed reactive bone formation at the prosthesis tip. This reactive bone was seen to extend from the tip of the component to the medial cortex when the stem was in valgus, the lateral cortex when the stem was in varus, and was central or pancentral when the stem was neutral (Figures 6 to 8). Twenty-nine (56%) had developed medial calcar rounding and 23 (44%) showed evidence of further proximal stress shielding which was graded as second degree in 19 and third degree in four.


All of the 52 femoral components were graded as having achieved bony fixation as per Engh's criteria.
The average acetabular inclination on the antero-posterior radiograph was 46.04° (range 32 to 60°). Fourteen (27%) of the hips had lateral uncoverage, with an average of 10.57° (range 4° to 23°). At last radiographic review, none of the cups had migrated. Circumferential radiolucencies of less than 1 mm in all three zones were seen in three hips (6%). One of these was noted in the immediate post-operative period, and is attributed to incomplete component seating.
A further 26 cups (50%) had radiolucent lines (of less than 1 mm thick) in one or more of the DeLee and Charnley zones: 13 in zone A (average 12 mm), one in zone B (15 mm), seven in zone C (average 18 mm), three in zones AB (average 33 mm) and two in zones BC (average 30 mm).
There were three cases (6%) of focal peri-acetabular osteolysis, graded mild (<1 cm2) in two and moderate (<2 cm2) in one. Two of the cups had pegs and the other had screws. There was no evidence of liner wear in any of the above.
Twenty of the 52 radiographs (38%) demonstrated heterotopic ossification, Brooker grade 1 in ten hips (19%), grade 2 in six (11%), and grade 3 in four (8%).
Discussion
Total hip replacement is being performed on younger patients. The Finnish registry shows a progressive increase, since the late 1980s, in the proportion of primary surgeries done in the age group 49 to 59 years. In the UK national joint registry, patients under the age of 55 years account for 12% of the arthroplasty burden.14
There remains debate regarding component fixation and bearing surface in this patient population. The available options for component fixation are: all cemented, all uncemented and hybrid/reverse hybrid (acetabular cementation and uncemented femoral fixation). Evolving implant technology, and improved surgical and cementation techniques have resulted in a progressive improvement in prosthesis survival in both cemented and uncemented arthroplasty, the most dramatic being uncemented. This improvement has however not been uniform across different prostheses, with certain cemented and uncemented options demonstrating unacceptably high revision rates.
There has been a marked increase in the use of uncemented components, as seen in registry data. The Norwegian Arthroplasty register report of June 2010, and the British registry report of 2011 indicate that the most commonly used stem in primary hip arthroplasty is a fully hydroxyapatite-coated uncemented prosthesis. In the Canadian registry, in 2009/2010 82.9% of the primary total hip replacements were uncemented.15
Cemented stems are still considered by many to be the gold standard. Burston et al, using a polished tapered stem and new generation cementing technique, reported no stem revisions for aseptic loosening or osteolysis at a minimum of ten years.16
There is, however, good long-term evidence in support of certain of the hydroxyapatite-coated stems, with survival rates of greater than 95% at 20 years.3
Survival data from the Norwegian arthroplasty register in patients under the age of 60 years supports the use of hydroxyapatite-coated femoral prostheses. It also supports the use of cemented acetabular components over any of the uncemented options. Over the past 12 years in that register, there has been a progressive increase in the percentage of reverse hybrid arthroplasties. In a review of just under 4 000 reverse hybrid total hip replacements in patients under 60 years on the Norwegian register, survival rates at 5 and 7 years (up to 10) were the same as cemented total hip replacements.17
As noted by a number of authors, the major problem in both cemented and uncemented arthroplasty in young patients remains the acetabular component.18-20 Surgery for aseptic loosening, osteolysis and liner exchange forms a large part of the revision burden.
In this study, besides the two revisions for deep sepsis, none of the stems has been revised. All have shown radiographic evidence of fixation via bony ingrowth. There was a high rate of intra-operative femoral calcar fracture, which is likely due to attempts by trainee surgeons to fit larger stems, and consequently overstuffing the proximal femur. Reassuringly all of these fractures healed uneventfully and without subsidence.
Eighty per cent of the hips demonstrated reactive bone formation at the femoral component tip, and 81% demonstrated a reactive double line formation in zone 1. These findings are in keeping with previous reports on the use of the Corail stem. The double line formation is attributed to distraction forces on the proximal-lateral aspect21 (Figure 10). One of the stems subsided in the early post-operative period, but was judged to have achieved bony fixation at review 5 years later. The subsidence is attributed to a technical error and undersizing of the component. The particular stem used in this case is rarely used in the unit, which may also be a contributing factor.
Although we report a high rate of heterotopic bone formation (20 of 52 hips), the vast majority were Brooker grade 1 or 2, and not clinically significant. We report three cases of focal peri-acetabular osteolysis. As these were non-progressive, and the patients asymptomatic, no further surgery has been undertaken.
Notably, the patient demographics in this study differ significantly from those in other studies and in registry data. The primary indication for surgery was avascular necrosis in over two-thirds of the cases, inflammatory in 9% and primary osteoarthritis in only 5%. Streit et al22 in a study of primary hip arthroplasty done in German patients under the age of 60 years had 52% osteoarthritis and only 20% avascular necrosis, while Archibeck et al had 32% osteoarthritis and 20% avascular necrosis in an American population under the age of 50 years.23
Identifiable risk factors for the development of avascular necrosis were noted as follows: in male patients, alcohol abuse in 65%, smoking in 62%, steroid use in 25%, trauma in 14%, and known HIV-positive status in 3%.
In female patients, alcohol abuse was noted in 18%, smoking in 9%, steroid use in 28%, trauma in 14%, and known HIV-positive status in 28%. The significance of HIV status, the development of AVN, and the outcomes of hip arthroplasty are currently being investigated by our unit.
The significance of the difference in aetiologies and how it may influence surgical outcomes, is however unclear. Radl et al evaluated stem subsidence and stem survival in patients with osteoarthritis and patients with AVN. They found a significant difference in stem subsidence, and stem survivals of 74% for avascular necrosis versus 89% for osteoarthritis at a median of 6 years. They suggest the differences can be attributed to the pathological process in the proximal femur of patients with avascular necrosis.24
Ince et al, however, showed no greater risk of subsidence and had no stem revisions in patients with avascular necrosis at an average of 7 years post uncemented arthro-plasty with a porous-coated stem.25 This was confirmed by Min et al who had a 95% stem survival at 10 years in patients with AVN.4
At time of last follow-up, eight of the 88 patients (9%) had demised. Although this may seem excessive, it should be taken in context. The death rate for adults aged 40 to 54 years in South Africa is estimated at 15 per 1 000 per year for females and 27 per 1 000 per year for males.26 This equates roughly with the death rate seen in this cohort of patients over the study period.
There are a number of limitations to this study. First, it is retrospective, and therefore reliant on information gained from previous notes. Secondly, as our institution performs mainly uncemented arthroplasty in this age group, there is no matched cohort of patients with which to compare our results. Thirdly, there was a high rate of attrition due to death and loss to follow-up which may have altered the analysis.
Conclusion
We have analysed a consecutive group of patients who underwent total hip replacement, and present our radiological results and complications at a minimum of 5 years' follow-up. Our findings regarding the radiographic features are in keeping with the published literature, and we have encountered no revisions for aseptic loosening. Uncemented component fixation remains a suitable option for patients under the age of 55 years requiring total hip arthroplasty.
References
1. Dorr LD, Kane TJ, 3rd, Conaty JP. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger. A 16-year follow-up study. J Arthroplasty, 1994;9(5):453-56. [ Links ]
2. Duffy GP, et al. Primary uncemented total hip arthroplasty in patients <40 years old: 10- to 14-year results using first-generation proximally porous-coated implants. J Arthroplasty, 2001;16(8 Suppl 1):140-44. [ Links ]
3. Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop, 2011;35(2):189-94. [ Links ]
4. Min BW, et al. Second-generation cementless total hip arthroplasty in patients with osteonecrosis of the femoral head. J Arthroplasty, 2008;23(6):902-10. [ Links ]
5. Eskelinen A, et al. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop, 2006;77(1):57-70. [ Links ]
6. Moyer JA, et al. Durability of second-generation extensively porous-coated stems in patients age 50 and younger. Clin Orthop Relat Res, 2010;468(2):448-53. [ Links ]
7. Blacha J. High osteolysis and revision rate with the hydroxya-patite-coated ABG hip prostheses: 65 hips in 56 young patients followed for 5-9 years. Acta Orthop Scand, 2004;75(3):276-82. [ Links ]
8. Garcia-Cimbrelo E, et al. Total hip arthroplasty with use of the cementless Zweymuller Alloclassic system. A ten to thirteen-year follow-up study. J Bone Joint Surg Am, 2003;85-A(2):296-303. [ Links ]
9. Gruen TA, McNeice GM, Amstutz HC. 'Modes of failure' of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res, 1979;141:17-27. [ Links ]
10. Engh CA, Bobyn JD,Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br, 1987;69(1):45-55. [ Links ]
11. Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration. An experimental study. J Arthroplasty, 1989;4(3):245-51. [ Links ]
12. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res, 1976;121:20-32. [ Links ]
13. Brooker AF, et al. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am, 1973;55(8):1629-32. [ Links ]
14. National Joint Registry for England and Wales 8th Annual Report. 2011. [ Links ]
15. Hip and Knee Replacements in Canada - 2011 Annual Statistics (Clinical Data) from the Canadian Institute for Health Information, 2011. [ Links ]
16. Burston BJ, et al. Cemented polished tapered stems in patients less than 50 years of age: a minimum 10-year follow-up. J Arthroplasty, 2010;25(5):692-99. [ Links ]
17. Lindalen E, et al. Is reverse hybrid hip replacement the solution? Acta Orthop, 2011;82(6):639-45. [ Links ]
18. Kim YH, et al. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg Br, 2011;93(4):449-55. [ Links ]
19. Wangen H, et al. Hip arthroplasty in patients younger than 30 years: excellent ten to 16-year follow-up results with a HA-coated stem. Int Orthop, 2008;32(2):203-208. [ Links ]
20. Kim YH, et al. Periacetabular osteolysis is the problem in contemporary total hip arthroplasty in young patients. J Arthroplasty, 2012;27(1):74-81. [ Links ]
21. Rokkum M, Reigstad A. Total hip replacement with an entirely hydroxyapatite-coated prosthesis: 5 years' follow-up of 94 consecutive hips. J Arthroplasty, 1999;14(6):689-700. [ Links ]
22. Streit MR, et al. High survival in young patients using a second generation uncemented total hip replacement. Int Orthop, 2012;36(6):1129-36. [ Links ]
23. Archibeck MJ, et al. Cementless total hip arthroplasty in patients 50 years or younger. J Arthroplasty, 2006;21(4):476-83. [ Links ]
24. Radl R, et al. Higher failure rate and stem migration of an uncemented femoral component in patients with femoral head osteonecrosis than in patients with osteoarthrosis. Acta Orthop, 2005;76(1):49-55. [ Links ]
25. Ince A, et al. No increased stem subsidence after arthroplasty in young patients with femoral head osteonecrosis: 41 patients followed for 1-9 years. Acta Orthop, 2006;77(6):866-70. [ Links ]
26. Statistics-SA. Adult mortality data (aged 16-64) based on death notification data in South Africa. Report no 03-09-05. 2006. [ Links ]
 Correspondence:
Correspondence:
Dr Paul Ryan
Private Bag X03
Mayville 4058
Tel: 031 240 2160
Email: paulrya@ialch.co.za
I have no conflicting interests, and received no benefits for writing this original article.














