Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.13 no.1 Centurion Jan./Mar. 2014
TRAUMA
Pre-hospital antibiotics for open fractures: Is there time?
Dr JK McCaulI; Mr MG McCaulII
IMBChB(UCT). Medical Officer in Orthopaedics, Somerset Hospital
IIBTech EMC(DUT), MSc Clin Epi (Stell) (c). Researcher, Biostatistics Unit, Centre of Evidence-based Health Care, Stellenbosch University
ABSTRACT
Early administration of intravenous (IV) antibiotics providing cover against Gram positive and negative organisms can be argued to be the single most important factor in reducing infection rate in patients with open (compound) fractures. By examining trends in the time period from injury to ultimate administration of IV antibiotics, the authors aim to clarify if there would be opportunity for pre-hospital antibiotic administration to significantly shorten the delay. A retrospective and prospective descriptive study was conducted of all patients with open fractures of the limbs or girdles arriving via ambulance at a single district hospital in a suburban area in KwaZulu-Natal, South Africa. Thirty-eight patients were identified from May to December 2012. The median time from injury to antibiotics was 465 minutes (7.75 hours) (first quartile = 230 minutes, third quartile = 615). Administration of antibiotics was delayed beyond 3 hours in 78.9% (95% confidence interval [CI] 65.3-92.52) of patients and beyond 6 hours in 60.5% (95% CI 44.2-76.8). Although much of the delay occurred due to clinic and in-hospital delays, there is also a hypothetical window available to pre-hospital healthcare providers where antibiotics could be administered. This would potentially decrease the delay and bypass many of the difficulties encountered in-hospital.
Key words: pre-hospital, antibiotic, open fracture, compound fracture.
Introduction
Early administration of intravenous (IV) antibiotics providing cover against Gram positive and negative organisms can be argued to be the single most important factor in reducing infection rate in patients with open (compound) fractures.1 A delay of more than 3 hours from injury (open fractures or war wounds including fractures) to antibiotic administration is associated with a significantly higher infection rate.2-4
Infection is a complication of open fractures. There have been reports of osteitis in 5.7%5 and 8.2% of patients (across all grades of fractures) with up to 23.7% observed for Gustilo-Anderson type IIIC fractures.6 Early surgical debridement has also been shown to be important in preventing infection.2 However, some studies have shown that, when early prophylactic IV antibiotics and open fracture first aid had been implemented, delaying aggressive debridement and lavage up to 13 hours post injury did not adversely affect the outcome.7 In animal studies, a delay to debridement of up to 24 hours increased the risk of infection, but not significantly; rather again showing that delay in timing of antibiotic administration (to 6-24 hours instead of less than 6 hours) had the most profound effect regardless of timing of surgery.8
Current practice in South Africa regarding management of open fractures involves administration of IV antibiotics soon after the patient arrives at a hospital or clinic. The patient is often treated in the pre-hospital setting by emergency medical care providers (EMCPs) on scene and en route to hospital. If early administration of IV antibiotics is important, is there not a role for an immediate dose of IV antibiotics in the pre-hospital setting?
The purpose of this study is to identify the proportion of patients in a suburban sample that experience delay in antibiotic administration after open fracture. By examining trends in the time period from injury to ultimate administration of IV antibiotics the authors aim to clarify if there would be opportunity for pre-hospital antibiotic administration to significantly shorten the delay.
Materials and methods
A retrospective and prospective descriptive study was conducted of all patients with open fractures of the limbs or girdles arriving via ambulance at a single district hospital in a suburban area in KwaZulu-Natal, South Africa. Data collection was performed from folders of patients arriving at the hospital from May to December 2012 (inclusive).
Prospective data was collected from September to December, supplemented with retrospective review of the previous four months. Ethical approval was obtained from Durban University of Technology (IREC Reference number: REC:42/12). Consent was obtained from the hospital manager to assess patient folders. Patients were not approached directly for information.
Inclusion and exclusion criteria
Included: All patients with fractures of their limbs, extremities, shoulder girdles or pelvis that were classified and managed as open and who were transported to the hospital's emergency department (ED) via an ambulance, either from the scene of trauma or from the local clinic. A fracture was classified as 'open' if it had a full-thickness skin wound which could conceivably communicate with the fracture site. Gunshot wounds with fractures were all regarded as open.
Excluded: Patients with open fractures of the skull or mandible, patients with incomplete or absent records where the total injury-to-antibiotic time could not be calculated, patients who came to the hospital with their own transport, and patients who had delay in seeking medical attention after injury.
Data gathering
Patients were identified from admission/transfer registers in the ED and the orthopaedic wards. Data were extracted and time intervals in minutes calculated from the hospital's copy of ambulance trip sheets kept in patients' folders as well as doctors' and nurses' clinical notes in the folder. Data were entered onto a pre-prepared electronic spreadsheet. Circumstances resulting in delay were collected when noted in the folder. The following data were collected: age, gender, mechanism of injury, grade of fracture (Gustilo-Anderson and Ganga Hospital score); times of: injury, call-out of ambulance, arrival on scene, departure from scene, out-of-hospital IV access, arrival at emergency department, antibiotic administration; choice and dose of antibiotic; route to hospital (via clinic or direct); and selected or notable circumstances causing delay.
Bias
A single researcher gathered the data from the folders. Hospital staff was informed about the study; this could have caused increased vigilance regarding administration of antibiotics, but this was not considered to add significant bias due to the study's focus on pre-hospital time available for administration.
Statistical methods
The sample size was calculated for the primary outcome (binary variable) with a baseline proportion of 0.8 with 13% precision. The estimated sample size was reached.
Quantitative variables were recorded in Excel and imported into Stata 11 for analysis. Basic descriptive analysis was used to describe the data, reporting medians and interquartile ranges (IQR) as the data were not normally distributed. The primary outcome variable was stratified into different time-subgroups to accommodate analysis. Subgroups were examined using basic summary statistics. Missing data were considered to be missing at random and analysed as missing data. All efforts were made to account for missing data.
Results
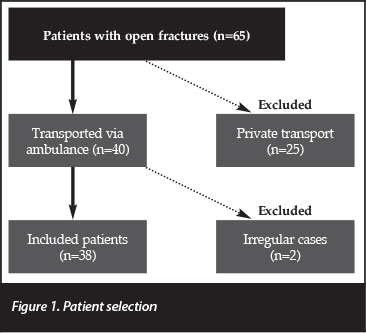
Sixty-five patients with open fractures arrived at the ED between May and December 2012 (inclusive). Twenty-five were excluded as they had utilised their own private transport to the hospital. Two further patients were excluded; one having first gone home before seeking medical care the next morning, while the other did not receive antibiotics at the study hospital and was transferred out without the relevant data being recorded. The final number of included patients was 38. See Figure 1 for a summary of patient selection. The mean age was 28.7 years (95% confidence interval [CI] 24.9-32.5) and 73.7% of patients were male (95% CI 59.0-88.4). For further demographic and clinical characteristics of included cases see Table I.
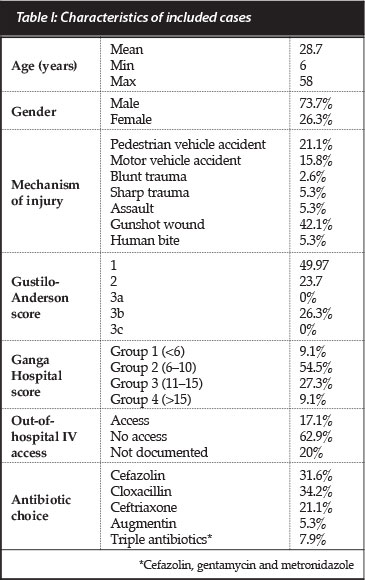
The median total time from injury to antibiotics was 465 minutes (7.5 hours) (first quartile [Q1] = 230 minutes, third quartile [Q3] = 615). Administration of antibiotics was delayed beyond 3 hours in 78.9% (95% CI 65.3-92.52) of patients and beyond 6 hours in 60.5% (95% CI 44.2-76.8).
The longest delay occurred after arrival at the hospital with a median of 363 minutes (Q1=171, Q3=505) until antibiotic administration. A median of 164 minutes (Q1=115, Q3=222) was spent out of hospital with emergency medical care practitioners (EMCPs) being in attendance for a median of 56 minutes (Q1=37, Q3=64). See Table II for all timeframes. Pre-hospital IV access was documented as obtained in 17.1% of patients, not obtained in 62.9% and no documentation was available for the remaining 20%.

Just over a quarter (26.3%) of patients were transported directly from the scene (of injury) to the hospital; they had a median time from injury to antibiotics of 170 minutes.
A subgroup of 13.2% patients travelled via a clinic and received antibiotics at the clinic after a median of 230 minutes after injury. The remaining 60.6% also travelled via a clinic but were not given antibiotics at the clinic, only receiving antibiotics at the hospital a median of 570 minutes after injury. There was a statistically significant difference in median times between patients who received clinic antibiotics and patients where the clinic omitted antibiotics (P<0.05). Other comparisons between routes were nonsignificant, possibly due to the small sample size.
Patients whose antibiotics were omitted by the clinic were 22 times more likely to experience delay greater than 3 hours (P=0.010) when compared to direct transfer from the scene, while patients who received clinic antibiotics were only 1.5 times more likely to be delayed (P=0.715).
Some data for time interval calculations were missing: only total time (injury to antibiotics) was available in two patients. Only time of injury, arrival at ED and administration of antibiotics was available in seven patients. One patient was missing the time of callout of ambulance. In 20% of patients it was not clear whether IV access was obtained in the pre-hospital setting or not.
Discussion
There was a delay to administration of antibiotics in a large proportion of patients in this study. This provides the opportunity to consider measures to decrease delay.
Pre-hospital antibiotics have been used in the military setting, where rapid evacuation to hospital is not always possible in conflict scenarios. It is suggested that antibiotics may be added to civilian pre-hospital care (consisting of control of haemorrhage, sterile dressing, reduction of gross deformity and pain management) if the transport time is anticipated to be greater than 60 minutes.3 The time intervals in this study show that the median time from injury to arrival at hospital was 100 minutes (Q1=61, Q3=115) for direct transfers to hospital (300 and 184 minutes for transfers via clinics with and without antibiotics, respectively). EMCPs were in attendance for a median of 56 minutes in the study sample. It has been suggested that pre-hospital times of up to 60 minutes are acceptable if the skill of the EMCP is sufficient and the destination hospital is capable of providing definitive trauma care.9
Unique protocols in civilian pre-hospital care may be worth considering in South Africa, with its own unique challenges and context. This study provides a glimpse into transport times and practices in KwaZulu-Natal and may not be able to be generalised to other countries or even other provinces/areas within South Africa. A systematic review and meta-analysis of transport times in the United States showed average ground ambulance pre-hospital times from callout to arrival at hospital for trauma patients to be 30.96, 30.97 and 43.17 minutes for urban, suburban and rural settings respectively. These included response times of 5.25, 5.21 and 7.72 minutes respectively. On-scene time contributed to 13.40, 13.39 and 14.59 minutes, while transport to the destination hospital took up 10.77, 10.86 and 17.28 minutes respectively.10 A British audit of patients requiring emergency laparotomy for liver or spleen injury found a median time from activation of the aeromedical team to arrival at the ED of 73 minutes.11
Possible factors causing delay in pre-hospital time in the study sample could include delay in contacting ambulance services; a high call load causing delay in dispatching of units to the scene; travelling times as influenced by distance, traffic and road conditions; shortage of resources; and time spent on scene stabilising patients and/or extricating entrapped patients. No patients in this sample were entrapped; however, this circumstance presents a special situation where a great delay in the pre-hospital setting could be anticipated and pre-hospital antibiotics could be of value.
One of the risks for delay in the study included omission of antibiotics when the patient first went to a clinic (via private transport or ambulance) before ambulance transfer to the hospital. Reasons for omission of antibiotics as part of emergency care at the clinics could possibly include lack of resources at the smaller clinics, insufficient staff to cope with patient load or lack of knowledge about the significance of early antibiotic administration. Administration of antibiotics soon after presentation at a clinic did lessen the risk of delay, but the lowest risk occurred when the patient was transferred directly to the hospital from the scene of injury. Correct transport directly to the appropriate facility would be ideal, possibly achieved by EMCP training in recognising open fractures in the pre-hospital setting and direct transport to appropriate hospitals. Community awareness of services provided at various levels of care is part of Batho Pele principles12 and striving to achieve this ideal would assist in empowering patients to present to the appropriate facilities should they choose to use their own transport.
The largest proportion of total time before antibiotic administration was spent in the hospital's ED. Reasons for delay included: delay in a doctor attending to the patient when the department was very busy; antibiotics not being ordered in the ED and only commenced on arrival to the wards; antibiotics being ordered in the ED but not administered; initially missing fractures that were not clinically evident, and initially misdiagnosing fractures as 'closed' before re-evaluation revealed accurate classification as 'open'. Measures that could reduce these delays include: clear protocols on emergency treatment; adequate triage; and improvements in patient flow through the department.
In an attempt to exclude in-hospital delay as a potential confounder causing a large proportion of patients to experience total-time delay, one could consider a hypothetical situation where no in-hospital delay is experienced, i.e. antibiotics are administered immediately on arrival to the ED. In this sample there would then still be a delay of greater than 3 hours in 54% of patients travelling via a clinic without antibiotics (0% of patients transferred directly to hospital would be delayed).
Choice of antibiotic is important. Staphylococcus aureus and Staphylococcus epidermidus are often cultured early from open fractures, while Pseudomonas and Enterococcus have been considered as nosocomial infections.13 Benzylpenicillin is ineffective for these types of organisms, with a second-generation cephalosporin being more suitable.13Clostridium species have also been identified and require IV antibiotics effective against anaerobes,3 e.g. in cases of soil contamination. A wide variety of antibiotics was used in the study sample (see Table I) which is perhaps due to lack of knowledge of correct protocol or inconsistencies in existing protocol; also it may reflect limited choice of antibiotic in local clinics as only ceftriaxone was administered by clinics in this study.
Limitations of this study include a small sample and limited observation period. No record of patient outcome (e.g. development of infection) was attempted; however, the patient database provides the possibility for follow-up in a future study to determine outcome. Reasons for delay, except when mentioned in the hospital folders, were not recorded. As previously mentioned, increased vigilance in in-hospital antibiotic administration, while potentially biasing the results toward shorter total time to antibiotics, was not considered to adversely affect the purpose of the study. This is because even if antibiotics were administered immediately after arrival at the hospital it would not affect pre-hospital times but rather reflect ideal in-hospital practice.
Further studies are required: similar studies in other centres and provinces would help to determine if antibiotic delay is a pervasive or isolated issue. Should other studies concur, considering introducing IV antibiotics to pre-hospital care could be of value. EMCP level of expertise (basic, intermediate or advanced life support practitioners) would need to be taken into account as IV antibiotics are not without complications - such as anaphylaxis.
Advanced life support practitioners are trained and equipped to deal with this scenario; therefore it is conceivable that it would be safer to introduce IV antibiotics to the advanced scope of practice only. Before considering introducing antibiotics to the EMCP spectrum of care, efficacy, safety and cost-effectiveness studies would need to be undertaken. Randomised controlled trials are also recommended to determine the effect of pre-hospital antibiotic administration on delay, infection rates and occurrence of adverse events.
There is much room for improvement within the study hospital and its drainage clinics in preventing delay in antibiotic administration. However, although much of the delay occurred due to clinic and in-hospital delays, there is also a hypothetical window available to pre-hospital healthcare providers where antibiotics may be administered. This could decrease the time interval and bypass many of the difficulties encountered in-hospital.
Acknowledgements
Thank you to Tonya Esterhuizen from the Biostatistics unit, Stellenbosch University for her support.
References
1. Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clinical Orthopaedics and Related Research. 1989;243:36-40. [ Links ]
2. McCaskill ME, Little DG. Time to definitive management of open fractures of long bones. Emergency Medicine. 1993;5(4):272-75. [ Links ]
3. Eardley W, Brown K, Bonner T, Green A, Clasper J. Infection in conflict wounded. Philosophical Transactions of the Royal Society B: Biological Sciences. 2011;366(1562):204-18. [ Links ]
4. Jackson D. Soldiers injured during the Falklands campaign 1982 sepsis in soft tissue limb wounds. JR Army Med Corps. 2007;153(Suppl 1):55-56. [ Links ]
5. Khatod M, Botte MJ, Hoyt DB, Meyer RS, Smith JM, Akeson WH. Outcomes in open tibia fractures: Relationship between delay in treatment and infection. The Journal of Trauma and Acute Care Surgery. 2003;55(5):949-54. [ Links ]
6. Seekamp A, Kontopp H, Schandelmaier P, Krettek C, Tscherne H. Bacterial cultures and bacterial infection in open fractures. European Journal of Trauma. 2000;26(3):131-38. [ Links ]
7. Harley BJ, Beaupre LA, Jones CA, Dulai SK, Weber DW. The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. Journal of Orthopaedic Trauma. 2002;16(7):484-90. [ Links ]
8. Penn-Barwell JG, Murray CK, Wenke JC. Early antibiotics and debridement independently reduce infection in an open fracture model. Journal of Bone & Joint Surgery, British Volume. 2012;94-B(1):107-12. [ Links ]
9. McDonell AC, Veitch C, Aitken P, Elcock M. Policy and service delivery. Journal of Emergency Primary Health Care (JEPHC). 2009;7(2):990308. [ Links ]
10. Carr BG, Caplan JM, Pryor JP, Branas CC. A meta-analysis of prehospital care times for trauma. Prehospital Emergency Care. 2006;10(2):198-206. [ Links ]
11. Henderson KIM, Coats TJ, Hassan TB, Brohi K. Audit of time to emergency trauma laparotomy. British Journal of Surgery. 2000;87(4):472-76. [ Links ]
12. White Paper on Transforming Public Service Delivery (Batho Pele White Paper). In: Administration DoPSa, editor. Notice 1459 of 1997 ed. Pretoria: Goverment Gazette; 1997. [ Links ]
13. Vainionpaa S, Vasenius J, Rokkanen P. Benzylpenicillin ineffective for open fractures: Prospective study of 60 cases. Acta Orthopaedica. 1990;61(2):158-60. [ Links ]
 Correspondence:
Correspondence:
Mr MG McCaul
Tel: (021) 938-9314
Email: mmccaul@sun.ac.za
The authors have no conflict of interest to declare. No direct funding was received for this project.














