Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.12 no.4 Centurion dic. 2013
BONE INFECTION
Open tibial bone transport following a failed bi-Masquelet procedure -a case report
N Ferreira, LC Marais
BSc, MBChB, HDip Orth(SA), FC Orth(SA), MMed(Orth) MBChB, FCS(Orth)(SA), MMed(Orth), CIME Tumour, Sepsis and Reconstruction Unit, Department of Orthopaedic Surgery, Grey's Hospital, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
ABSTRACT
Large bone defects are challenging to reconstruct and require specialised techniques, multiple surgeries, and long treatment periods. When these bony defects are associated with large soft tissue defects, it complicates the management further, necessitating soft tissue reconstruction in the form of local or free flaps. We report a case of a 25-year-old male, where a failed bi-Masquelet procedure resulted in a large bone and soft tissue defect of the tibia. Local or free flap reconstruction was not possible due to the extensive scarring and lack of vascular donor vessels. Open bone transport, using distraction histogenesis, was successful in reconstructing both the bone and soft tissue defects.
Key words: bone transport, bi-Masquelet, Ilizarov, bone defect, reconstruction
Background
Managing large bone defects can be challenging for any orthopaedic surgeon.1-5 Achieving satisfactory anatomical and functional results places increased demands on both the patient and surgeon, and requires a significant investment in terms of resources and time.4,6,7 Most reconstructive techniques involve soft tissue reconstruction during the initial phase, which is then followed by bony reconstruction.1,8 This sequence of events is not always possible as extensive soft tissue damage may preclude local flaps and patent donor vessels are required for free flaps.
We report a case of successful open bone transport following a failed bi-Masquelet procedure. Soft tissue and bony reconstruction was achieved simultaneously with the use of a circular external fixator and distraction histo-genesis.
Case report
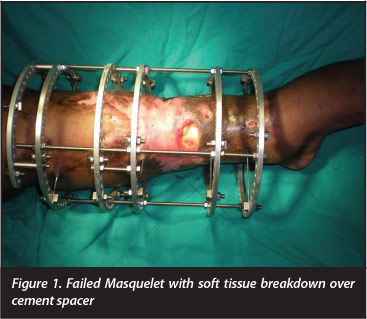
A 25-year-old man was referred to our tertiary level limb reconstruction unit after a failed bi-Masquelet procedure at a referring hospital/institution. He had sustained a severe open tibia fracture (Gustilo-Anderson IIIB) with circumferential soft tissue loss one year prior to presen-tation.9-11 His initial management included multiple debridements and monolateral external fixation. The bi-Masquelet procedure was undertaken to reconstruct an infected non-union of the left tibia. At presentation to our unit the extensively scarred soft tissue overlying the cement spacer had broken down and the wound was infected (Figure 1).
Soft tissue and bony reconstruction was achieved simultaneously
Local and systemic staging, according to the Cierny and Mader system, confirmed the diagnosis with stage IV B chronic osteomyelitis.12 Host status was compromised by both systemic and local factors. These included smoking; extensive circumferential soft tissue scarring; and the fact that no donor vessels were available for free flap soft tissue reconstruction. The foot was sensate and well perfused despite only having patent peroneal and tibialis posterior arteries. Although no significant joint contrac-tures were present, active ankle dorsiflexion was not possible due to muscle and tendon loss in the anterior compartment.
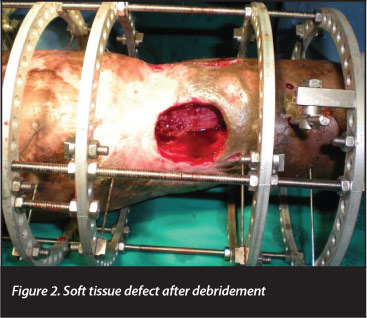
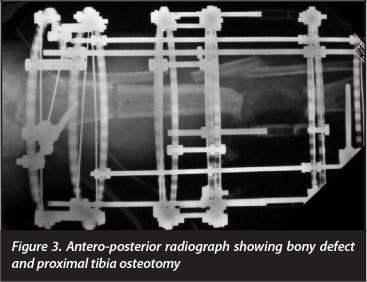
After counselling the patient about the available treatment options, including amputation, the decision to attempt limb salvage and reconstruction was made. The initial surgery involved removal of the cement spacer and debridement of all infected tissue, which resulted in a large antero-medial soft tissue defect and a 6 cm bone defect (Figures 2 and 3). Stability was maintained with the Truelok circular external fixator (Orthofix, Verona, Italy), and a transverse De Bastiani osteotomy of the proximal tibia was performed.13
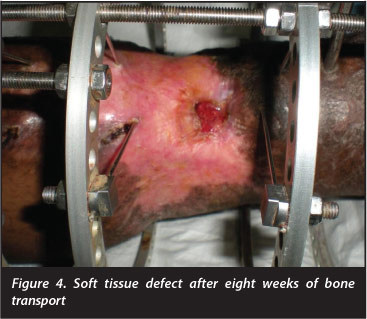
After a latency period of 10 days, distraction was commenced at a rate of 1 mm per day through four increments of 0.25 mm. Over the ensuing eight weeks, the soft tissue defects were closed through the process of distraction histogenesis (Figure 4). Formal docking was performed at 28 weeks, once the soft tissue over the docking site was completely healed. This comprised debridement of the interposed fibrous tissue, and a cancellous onlay graft was performed via an anterolateral approach.14 A saw-tooth regenerate pattern (Ru Li type 8)15 became apparent at seven months after the corticotomy and a further 32 weeks was required for regenerate consolidation and docking site union.
The circular external fixator was removed after a total of 60 weeks. The patient has subsequently returned to his employment as an automotive mechanic. No joint contrac-tures had developed as a result of the bone transport and he only required ankle-high boots to compensate for the loss of ankle dorsiflexion. At 2-year follow-up he has remained free of infection (Figure 5).

Discussion
Orthopaedic surgeons are frequently faced with segmental bone defects, either as a result of trauma, or secondary to debridement or tumour resection.1,2,5 Advances in the management of large bone defects have resulted in an increased use of limb salvage protocols in these patients.3,5 Where tibial defects smaller than 2 cm can be treated with simple cancellous bone grafting, defects larger than 4-5 cm will require specialised reconstructive techniques to prevent amputation.3,16,17
Two of the most common techniques used to reconstruct large bone defects are bone transport according to Ilizarov principles and bone graft into an induced membrane as described by Masquelet.11"1 As bone loss is frequently associated with soft tissue defects, either as a result of the primary injury or the subsequent surgical debridement, bony reconstruction is often combined with soft tissue reconstruction.1
Defects larger than 4 - 5 cm require specialised
reconstructive techniques to prevent amputation
Not only could bone continuity be restored through
distraction osteogenesis but in this case gradual distraction
was successful in facilitating soft tissue reconstruction
through distraction histogenesis
The Ilizarov bone transport and the Masquelet bone graft techniques incorporate different philosophies/principles in order to achieve skeletal integrity. Bone transport involves creating a free segment of living bone through a corticotomy or osteotomy. This free segment of bone is gradually transported into the bone defect while regenerate bone is formed at the trailing end through the process of distraction osteogenesis. Bone continuity is restored when the transported bone segment fuses with the target bone at the docking site.16 The Masquelet procedure is performed in two stages.6,20,21 The first stage relies on provoking a foreign body reaction around a cement spacer left in the osseous void.21 This results in the formation of an induced membrane in which cancellous bone graft is packed as a second stage. The induced membrane serves as a resilient receptacle for the graft and, in addition, prevents graft resorption.6,20,21 It has also been found that the membrane exhibits histologic characteristics and biological properties that facilitate bone healing.21-24 In the presence of soft tissue defects both these approaches, however, require soft tissue reconstruction in the form of local or free flaps during the initial phase of reconstruction.1,7,8,21,23,25-27
Bone transport was chosen to reconstruct the bony defect in our patient. Not only could bone continuity be restored through distraction osteogenesis but in this case gradual distraction was successful in facilitating soft tissue reconstruction through distraction histogenesis.1,28,29 The soft tissue defect healed completely during the process of bone transport and no additional soft tissue procedures were required.
Bone transport is associated with multiple challenges and complications.30 The most obvious challenge is the extended period of external fixation required.29 Our patient required 60 weeks of external fixation in order achieve adequate regenerate consolidation. This was probably influenced by smoking, as the saw-tooth regenerate that developed is frequently seen in smokers.15 Some of the most frequent complications of bone transport include: pin tract sepsis, failure of regenerate formation, regenerate fracture, regenerate deformity, docking site non-union, knee and ankle contractures, and recurring infection.30,31 Of these potential complications, only a five degree varus regenerate deformity occurred in our patient. This deformity was non-progressive and no further treatment is planned.
Conclusion
Open bone transport is a labour-intensive procedure that demands attention to detail, meticulous technique, lengthy hospitalisation and prolonged periods of external fixation. This technique should not be considered as a first option reconstruction procedure, but can be successfully employed where a bone defect is associated with an unreconstructable soft tissue defect.
Consent
Written consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The content of this article is the sole work of the author. No benefits of any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1. El-Alfy B, El-Mowafi H, El-Moghazy N. Distraction osteogenesis in management of composite bone and soft tissue defects. International Orthopaedics (SICOT) 2010;34:115-18. Doi: 10.1007/s00264-008-0574-3 [ Links ]
2. Chaddha M, Gulati D, Singh AP, Singh AP, Maini L. Management of massive posttraumatic bone defects in the lower limb with the Ilizarov technique. Acta Orthop Belg. 2010;76:811-20. [ Links ]
3. Kesemenli C, Subasi M, Kirkgoz T, Kapukaya A, Arslan H. Treatment of traumatic bone defects by bone transport. Acta Orthop Belg. 2001;76(4):380-86. [ Links ]
4. Lavini F, Dall'Oca C, Bartolozzi P. Bone transport and compression-distraction in the treatment of bone loss of the lower limbs. Injury, Int J. Care Injured. 2010;41:1191-95. [ Links ]
5. Manish K, Rabi J. Bone transport in tibial gap non-union - A series of 25 cases. Open Journal of Orthopedics. 2012;2:144-49. Doi: 10.4236/ojo.2012.24027 [ Links ]
6. Karger C, Kishi T, Schneider L, Fitoussi F, Masquelet AC. Treatment of posttraumatic bone defects by the induced membrane technique. Orthop Traumat Surg Res. 2012;98:97-102. Doi:10.1016/j.otsr.2011.11.001 [ Links ]
7. Donegan DJ, Scolard J, Matuszewski PE, Mehta S. Staged bone grafting following placement of an antibiotic spacer block for the management of segmental long bone defects. Orthopedics. 2011;34(11):e370-e735. DOI: 10.3928/0147744720110922-16 [ Links ]
8. Gordon L, Chiu EJ. Treatment of infected non-unions and segmental defects of the tibia with staged microvascular muscle transplantation and bone-grafting. J Bone Joint Surg Am. 1988;70(3):377-86. [ Links ]
9. Standards for the management of open fractures of the lower limb. http://www.boa.ac.uk/Publications/Documents/LowerLimbGuide.pdf [ Links ]
10. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 1976;56(4):453-58. [ Links ]
11. Gustilo RB, Mendoza RM, Williams DN. Problems in the mangement of type III (severe) open fractures. A new classification of type III open fractures. J Traum 1984;24(8):742-46. [ Links ]
12. Cierny G, Mader JT, Pennick JJ. A clinical staging system for adult osteomyelitis. Contemp Orthop. 1985;10:17-37. Doi: 10.1097/01.blo.0000088564.81746.62 [ Links ]
13. De Bastiani G, Aldegheri R, Renzi-Brivio L, Trivella G. Limb lengthening by callus distraction (callotasis). J Pediatr Orthop. 1987;7:129-34. [ Links ]
14. Phemister DB. Treatment of ununited fractures by onlay bone grafts without screw or tie fixation and without breaking down the fibrous union. J Bone joint Surg Am. 1947;29:946-60. [ Links ]
15. Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24(3):339-47. Doi: 10.1002/jor.20026 [ Links ]
16. Lasanianos NG, Kanakaris NK, Giannoudis PV. Current management of long bone large segmental defects. Orthopaedics and Trauma. 2009;24:149-63. [ Links ]
17. Keating JF, Simpson AHRW, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg [Br]. 2005;87-B:142-50. Doi: 10.1302/0301-620X.87B2 [ Links ]
18. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and soft tissues preservation. Clin Orthop 1989;238:249-81. [ Links ]
19. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate of frequency of distraction. Clin Orthop 1989;239:263-85. [ Links ]
20. Masquelet AC, Fitoussi F, Begue T, Muller GP. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000;45(3):346-53. [ Links ]
21. Masquelet AC, Beque T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41(1):27-37. Doi: 10.1016/j.ocl.2009.07.011 [ Links ]
22. Motsitsi NS. Masquelet's technique for management of long bone defects: from experiment to clinical application. East Cent. Afr. J. surg. 2012;17(2):43-47. [ Links ]
23. Uzel A-P, Lemonne F, Casoli V. Tibial segmental bone defect reconstruction by Ilizarov type bone transport in an induced membrane. Orthop Traumatol Surg Res. 2010;96:194-98. [ Links ]
24. Viateau V, Bensidhoum M, Guillemin G, Petite H, Hannouche D, Anagnostou F, Pelissier P. Use of the induced membrane technique for bone tissue engineering purposes: animal studies. Orthop Clin N Am. 2010;41:49-56. [ Links ]
25. Dendrinos GK, Kontos S, Lyritsis E. Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg. 1995;77A:835-46. [ Links ]
26. Paley D, Catagni M, Argnani F, Villa A, Benedetti GB, Cattaneo R. Treatment of tibial non-unions with bone loss. Clin Orthop. 1989;241:146-65. [ Links ]
27. Schottle PB, Werner CM, Dumont CE. Two-stage reconstruction with free vascularized soft tissue transfer and conventional bone graft for infected nonunions of the tibia: 6 patients followed for 1.5 to 5 years. Acta Orthop. 2005;76(6):878-83. [ Links ]
28. Sugar G, Fleischmann W, Hartwig E, Kinzl L. Open segmental bone transport. A therapeutic alterative in post-traumatic and osteitis soft tissue and bone defects. Unfallchirurg 1995;98(7):381-85. [ Links ]
29. Paley D, Maar DC. Ilizarov bone transport treatment of tibial defects. J Orthop Trauma. 2000;14(2):76-85. [ Links ]
30. Iacobellis C, Berizzi A, Aldegheri R. Bone transport using the Ilizarov method: a review of complications in 100 consecutive cases. Strat Traum Limb Recon. 2010;5:17-22 DOI 10.1007/s11751-010-0085-9 [ Links ]
31. Fabry K, Lammens J, Delhey P, Stuyck J, Pellenberg UZ. Ilizarov's method: a solution for infected bone loss. Eur J Orthop Surg Traumatol. 2006;16:103-109. DOI 10.1007/s00590- 005-0052-1 [ Links ]
 Correspondence:
Correspondence:
Dr N Ferreira
Department of Orthopaedic Surgery Grey's Hospital
Private Bag X9001
Pietermaritzburg 3201
Tel: +27 33 897 3299
Fax: +27 33 897 3409
Email: drferreiran@gmail.com














