Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.12 n.4 Centurion Dec. 2013
KNEE
Focal full thickness articular cartilage lesions treated with an articular resurfacing prosthesis in the middle-aged
H HobbsI; N Ketse-MatiwaneII; W van der MerweIII, IV; M PosthumusV
IMBChB(UCT), Dip PEC(SA), FC Orth(SA), MMed Orth (UCT) The Sports Science Orthopaedic Clinic, Cape Town, South Africa
IIMSc UCT/MRC Research Unit for Exercise Science and Sports Medicine of the Department of Human Biology, Faculty of Health Sciences, University of Cape Town, South Africa
IIIMBChB(UOFS), Social Studies (Oxford), BMed Sport Hons(UCT) FCS(SA)Ortho The Sports Science Orthopaedic Clinic, Cape Town, South Africa
IVMBChB(UOFS), Social Studies (Oxford), BMed Sport Hons(UCT) FCS(SA)Ortho UCT/MRC Research Unit for Exercise Science and Sports Medicine of the Department of Human Biology, Faculty of Health Sciences, University of Cape Town, South Africa
VPhD, BSc(Hons) UCT/MRC Research Unit for Exercise Science and Sports Medicine of the Department of Human Biology, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
INTRODUCTION: Localised full thickness articular defects of the knee are common and disabling in the middle-aged. There are numerous treatment options for articular defects, the results of which are unpredictable in this age group. The purpose of this study was to evaluate a focal articular resurfacing prosthesis used in the treatment of these defects.
METHODS: A consecutive series of patients treated between 2005 and 2010 with a HemiCAP® resurfacing procedure were retrospectively reviewed. Follow-up scores of the KOOS, IKDC, SF-36 and patient satisfaction were obtained. Radiographic evaluation was also obtained.
RESULTS: Twenty-two patients met the inclusion criteria. Nineteen patients were followed-up 4.7 ± 5.9 years after surgery. Three patients had revision surgery and were not followed up. The patients were 44.7 ± 5.9 years old. The follow-up KOOS scores demonstrated comparable scores on the pain and activities of daily living sub-scales when compared to normative data; however, the sports (P<0.001) and quality of life (P=0.001) sub-scales scores were lower in the HemiCAP® patients when compared to normative data. Only the physical functioning sub-scale score of the SF-36, and not the other seven sub-scale scores, was lower (P=0.016) in the HemiCAP® patients when compared to normative data. General patient satisfaction revealed that 79% considered their result as very good or excellent.
CONCLUSION: HemiCAP® articular resurfacing is an effective treatment option for pain in the middle-aged patient with a focal articular cartilage defect in the knee.
Key words: HemiCAP®, knee cartilage lesion, resurfacing prosthesis, cartilage repair, arthroplasty
Introduction
The number of total knee arthroplasties continues to grow each year and as these increase in number, the number of revision total knee arthroplasties continues to increase substantially.1-3 Total or uni-compartmental knee arthro-plasty is also associated with an increased morbidity and revision rate in younger patients.4-6
Articular cartilage performs an important function in the homeostasis and functioning of joints.7-8 Focal full thickness articular lesions not only cause pain but also disturb this homeostasis and can lead to osteoarthritis if left untreated.7-5-11 The majority of these full thickness cartilage lesions are observed in patients over the age of 40 years.1112
A plethora of cartilage repair techniques is described in the literature,1314 with the most common form of surgical treatment undertaken being microfracture. The results with these surgical treatments are promising in young patients; however, the results are inconsistent and poorer in patients older than 40 years of age.15-18
The purpose of our study was to evaluate an articular resurfacing prosthesis (HemiCAP®, Arthrosurface Inc., Franklin, MA, USA) being used in middle-aged patients for focal full thickness articular cartilage lesions. This prosthesis forms a junction between biological healing and conventional arthroplasty. We evaluated our results and failures done in a single centre and report our results in the context of previously reported normative data19,20 as well as published data from previous multi-centred studies.21,22
Materials and methods
Participants
We retrospectively reviewed 30 patients who had undergone a HemiCAP® resurfacing procedure between 2005 and 2010. All patients had previously failed conservative and/or surgical management. All surgeries were performed by the same surgeon (author WvdM). All focal full thickness articular defects of the femoral condyle and patellofemoral joint were included in the review. All patients were screened according to the inclusion and exclusion criteria. The inclusion criteria were: all patients were >35 years old; had clinically significant baseline pain requiring surgical intervention; failed conservative and/or surgical management; good joint stability in the affected joint with a grade 1 Lachman or less with no pivot shift for anterior instability and no posterior translation of more than Grade 1; passive motion deficit measured as a lack of extension less than 10 degrees; normal or asymptomatic contralateral joint; and had signed the informed consent form to participate in the study. Exclusion criteria were as follows: patients with more than one grade IV (ICRS) articular surface defect on their femur as diagnosed intra-operatively resulting in inadequate implant coverage; severely obese with a BMI >35 kg/m2 at the time of surgery; impaired mental comprehension and literacy, including dementia, psychological impairment, and misuse of drugs or alcohol; displays varus or valgus joint malalignment greater than seven mechanical degrees in the affected limb; presents evidence of rheumatoid arthritis, gross joint destruction, infectious/crystal arthropathy; bone resorption visible on pre-operative roentgenogram or presents evidence of chronic instability or deficient soft tissues, support structures, vascular or muscular insufficiency; had a prior meniscal allograft, a failed osteochondral grafting with the presence of cysts, or partial joint replacement; significant damage (defined as worse than grade II changes) to the articular surface opposing the implant on the tibia as diagnosed intra-operatively; significant symptomatic damage to articular surfaces in other compartments within the affected joint as diagnosed pre- and intra-operatively or has infection, sepsis, and osteomyelitis or other active infections that may spread to the implant site.
Seven patients were lost to follow-up and were excluded from this series. One patient was excluded due to the fact she was diagnosed with rheumatoid arthritis at re-operation, when being revised from a HemiCAP® to a total knee arthroplasty.
Of the 22 patients who met the inclusion and exclusion criteria, 15 were male and seven female. All patients gave written informed consent. All the patients had swelling of the affected knee and moderate to severe pain at the time of presentation. All patients had a pre-operative MRI, which demonstrated an articular lesion with underlying bony changes.
Ethical approval was obtained and all patients signed a consent form to participate in the review.
Follow-up
All patients were invited to attend and were followed up for this case series between 4 and 6 years after surgery. All patients were assessed using the subjective Knee Injury and Osteoarthritis Outcome Score (KOOS),23 the subjective general health SF-3624 and patient satisfaction questionnaires. The KOOS score has been validated for the treatment of focal cartilage lesions.25 Data for the KOOS score and the SF-36 was compared to previously published normative data.19,20
In addition, the outcomes were also rated by an independent orthopaedic surgeon, following the International Knee Documentation Committee (IKDC) evaluation form.26 Radiographic assessment entailed comparing pre-operative radiographs to those obtained at the follow-up visit (AP and lateral knee X-rays weight bearing and a mechanical axis). These were then assessed using the Kellgren-Lawrence classification27 and Osteoarthritis Research Society International (AORSI) grading system28 to see if there were any changes.
Surgical technique and prosthetic device
A standard arthroscopy was performed and the lesion was evaluated in all included patients.
A small medial para-patellar arthrotomy was then undertaken. A guide pin was placed into the centre of the defect and the cancellous screw inserted. Mapping instruments were used to measure the surface curvature, upon which a matching surface reamer was used to prepare the bed. Sizing was then done using trials. The articular component was then inserted onto the fixation device and recessed slightly below the surrounding articular cartilage.
Statistics
The statistical analysis was performed using GraphPad Instat version 3 (GraphPad Software Inc., California, USA). Values were reported as a mean ± standard deviation (SD). To identify if the reported values were in range of the previously reported normative data for the validated scores reported, unpaired t-tests were performed between the means and standard deviations of the HemiCAP® patients and the means and standard deviations of the reported normative data. Significance was accepted when P<0.05.
Results
Patient characteristics
Of the 22 patients who met the inclusion criteria for the study, 15 were male and seven female. The average age of the patients was 44.7 ± 5.9 years (range 35-57). Patients were followed up 4.7 ±1.6 years (range 2-6) years after surgery. Fifteen of the lesions involved the right knee and seven the left. Sixteen had one or more prior cartilage procedure(s). Seven of the lesions were in the medial femoral condyle, 14 in the trochlea (of which five also involved the patella) and one was in the patella. Five of the patients had cartilage lesions elsewhere in the knee but were grade 2 or less. Six had partial medial meniscec-tomies (less than 50%) at the same procedure which could be a confounding factor. Of the seven lesions in the medial femoral condyle, six were resurfaced with a 20 mm prosthesis and one with a 15 mm prosthesis. Fourteen of the patellofemoral lesions, which were trochlea lesions, were resurfaced with a 20 mm prosthesis (five of these also had a patella resurfacing). One patient had a patella resurfacing only.
Three of the 22 patients had been revised since implantation and inclusion in this study. The three failures are discussed below. The outcomes at the current follow-up were recorded in the remaining 19 patients.
All patients reported that they would undergo the procedure again,
and that they would recommend it to family or friends
KOOS, SF-36 and patient satisfaction
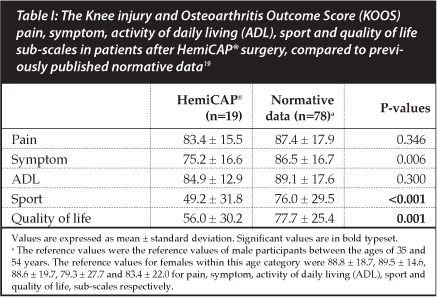
The KOOS (Knee injury and Osteoarthritis Outcome Score) questionnaire Pain (P=0.346) and ADL (P=0.300) sub-scales were not different between the HemiCAP® patients and the normative data (Table I). Symptom (P=0.006), sport (P<0.001) and quality of life (P<0.001) KOOS sub-scales were significantly lower within the HemiCAP® patients when compared to the normative data.
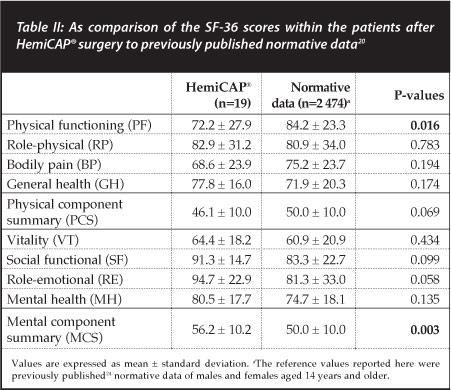
The short form (SF)-36 questionnaires consisted of eight sub-scales (Table II). The physical functioning (PF), role-physical (RP), bodily pain (BP) and general health (GH) sub-scales are combined into the physical component summary (PCS). The vitality (VT), social functional (SF), role-emotional (RE) and mental health (MH) sub-scales are combined into the mental component summary (PCS). Of the eight sub-scales, only the PF (P=0.016) was significantly lower within the HemiCAP® patients, compared to previously reported normative data.20 The MCS was significantly higher (P=0.003) within the HemiCAP® patients, compared to previously reported normative data.20
General satisfaction by the patients with the procedure was rated as excellent by nine (47%), very good by six (32%), good by two (11%), and fair by two (11%). All patients reported that they would undergo the procedure again, and that they would recommend it to family or friends. Nine patients had no pain at all, ten had mild pain requiring occasional analgesia. No subjective data was obtained for the three revisions.
Surgeon-rated outcomes
These outcomes were rated by one of the co-authors who is an independent orthopaedic surgeon. At follow-up 13 (68%), four (21%) and two (11%) of the patients had normal, nearly normal and abnormal effusion, respectively, according to the IKDC evaluation.26 No patients had severely abnormal effusion at follow-up. In addition, 15 (79%), three (16%) and one (5%) of patients had normal, nearly normal and abnormal passive motion deficits, respectively. No patients had severely abnormal passive motion deficits. Ligament examination was normal for all 19 patients. Eleven of the 19 patients (58%) were classified as normal for all measurements of the IKDC knee evaluation.
The result in six patients was rated by the surgeon(s) as excellent (32%), very good in nine (47%), good in three (16%), and fair in one (5%). Radiographically there were no lucencies or cysts around the prosthesis and no subsidence of the prosthesis in any patient. There was no significant change in any of the radiographic findings or grades. One patient had disengagement of the articular component from the fixation device.
Revisions
Re-operations were done in three of the 22 patients (14%). The first was a patient who had a resurfacing of her trochlea and patella. She subsequently had another arthroscopy for pain where scar tissue was debrided. She was finally converted to a total knee arthroplasty for ongoing pain and swelling. The second patient had a medial femoral condyle HemiCAP® who had continued pain and swelling, and at arthroscopy had progression of the disease with cartilage involvement posterior to the prosthesis.
She was converted to uni-compartmental knee arthroplasty. The last patient also had a medial femoral condyle HemiCAP® and initially did extremely well, but had injured himself and sustained an MCL tear and an impaction fraction of the medial femoral condyle. He was treated conservatively for this injury but subsequently a year later the articular component disengaged from the fixation device (Figures 2A and 2B). He was converted to osteochondral plugs. At re-operation in all three patients, the HemiCAP® was easily removed and it was easy to convert to the chosen new treatment modality.
Discussion
The current case series documents the outcome of 22 patients, who had undergone a HemiCAP® focal isolated articular resurfacing procedure. At the current follow-up, 19 of the 22 patients were satisfied with the treatment and had successful alleviation of their pain.
Compared to normative data, the KOOS sub-scales for pain and activities of daily living were not significantly different.
Full thickness cartilage lesions are common and lead to symptomatic painful knees, the majority of which occur in the middle-aged (40-60 years).10,12 If left untreated, these defects are unlikely to heal and are a predisposing factor for the development of osteoarthritis.7,11,29 Conventional biological treatment measures include marrow stimulation techniques, osteochondral autografts and autol-ogous chondrocyte implantation (ACI). However, the outcomes of these conventional biological treatments within a middle-aged population are inferior and less predictable when compared to a younger (<40 years) population.15,17,18 Marrow stimulation techniques have shown a strong correlation between the age of the patient and the size of the lesion, better for small lesions less than 2 cm2 and patients under 35 years.15,18 Osteochondral autografts and allografts are not only technically demanding but have also been shown to have better results in patients under 40 years. The autografts have the added problem of donor site morbidity whereas the allografts have an increased risk of disease transmission and immunological reactions.26,30 ACI has shown favourable results, especially for larger lesions (>2 cm2). ACI is however costly; it is a two-stage operation and there is a lengthy rehabilitation.16,31 It has been shown to have inferior results when performed after a previous failed cartilage repair procedure, especially microfracture.32,33
Arthroplasty is another option, especially if the patient has already failed biological repair. However, arthroplasty is this age group not only removes healthy soft tissue and bone stock, which should be preserved, but has a limited survivorship and a greater risk of revision surgery5,34
Full thickness cartilage lesions are common and
lead to symptomatic painful knees, the majority
of which occur in the middle-aged
The HemiCAP® is an articular resurfacing device that is contoured to match the patient's articular cartilage. It is designed to fill the articular lesion and be load-sharing, thereby stabilising the lesion and protecting the surrounding cartilage. It consists of two components: an articular and a fixation component that are connected with a morse taper (Figures 1A and 1B). The articular component is composed of cobalt chrome and is available in two sizes: 15 mm and 20 mm diameter. These are available in various off-set configurations which correspond to the radius of curvature at the implant site (Figure 1C). The fixation device is a titanium, fully cannulated cancellous screw.
In the current study we report KOOS and SF-36 scores similar to that of age and sex -matched normative data. Only the sport and quality of life sub-scale scores of the KOOS questionnaire were significantly lower when compared to normative data. These findings are however in agreement with previously published data,21 which also demonstrated decreased scores for the sports and quality of life sub-scales of the KOOS questionnaires. However, the KOOS sub-scale scores reported by Bollars et al.22 did not show a similar reduced score for sports and quality of life. The specific reason(s) for this discrepancy remains unknown. All the general health sub-scales, except for physical functioning, were similar or better than normative data in the current study. The previous two follow-ups published did not report measures of general health (the SF-36 questionnaire).
In the current study, most patients were generally very satisfied with the procedure and all patients would elect to have the surgery again. In addition, the surgeon also reported satisfactory to good outcomes in all the patients followed up.
The HemiCAP® focal isolated articular resurfacing procedure is proving to be a novel and successful treatment for middle-aged patients with focal full thickness cartilage lesions. Results reported here, as well as previously published data,21,22 demonstrate that this treatment may bridge the gap between biological healing and conventional arthroplasty. An additional benefit of the use of the HemiCAP® articular resurfacing procedure is that it does not compromise or affect further surgery, if required in the future. The HemiCAP® focal isolated articular resurfacing device is easily removed and converted to the procedure of choice.
It is however important to note that three of 22 patients failed. One of these patients had incurred a second injury and did not fail due to the surgery. The other two patients had progression of the presenting lesions and ongoing pain and swelling. They demonstrate the importance of adhering to strict indications. Due to the paucity of data and patient numbers with respect to this device, we were unable to compare our revision rate with other studies.
The HemiCAP® focal isolated articular resurfacing
procedure is proving to be a novel and successful
treatment for middle-aged patients
Conclusion
This study presents the results of 22 patients, which had undergone a HemiCAP® focal isolated articular resurfacing procedure. The strength of the current study is that all surgeries were performed by a single surgeon at the same centre. The two previously published HemiCAP® follow-ups were both multi-centre studies. The results from the present study agree with the previously published follow-ups that the device is an effective reconstructive treatment option for patients with large cartilage lesions in the medial femoral condyle, the trochlea and in the patella.
References
1. Dixon T, Shaw M, Ebrahim S, Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis 2004;63:825-30. [ Links ]
2. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-85. [ Links ]
3. Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am 2005;87:1222- 28. [ Links ]
4. Furnes O, Espehaug B, Lie SA, Vollset SE, Engesaeter LB, Havelin LI. Failure mechanisms after unicompartmental and tricompartmental primary knee replacement with cement. J Bone Joint Surg Am 2007;89:519-25. [ Links ]
5. Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res 2007;464:83-87. [ Links ]
6. Harrysson OL, Robertsson O, Nayfeh JF. Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res 2004;162-68. [ Links ]
7. Davies-Tuck ML, Wluka AE, Wang Y et al. The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthritis Cartilage 2008;16:337-42. [ Links ]
8. Dye SF. The knee as a biologic transmission with an envelope of function: a theory. Clin Orthop Relat Res 1996;10-18. [ Links ]
9. de Windt TS, Bekkers JE, Creemers LB, Dhert WJ, Sari s DB. Patient profiling in cartilage regeneration: prognostic factors determining success of treatment for cartilage defects. Am J Sports Med 2009;37 Suppl 1:58S-62S. [ Links ]
10. Heir S, Nerhus TK, Rotterud JH et al. Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 2010;38:231-37. [ Links ]
11. Hjelle K, Solheim E, Strand T, Muri R, Brittberg M. Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 2002;18:730-34. [ Links ]
12. Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 1997;13:456-60. [ Links ]
13. Alford JW, Cole BJ. Cartilage restoration, part 1: basic science, historical perspective, patient evaluation, and treatment options. Am J Sports Med 2005;33:295-306. [ Links ]
14. Buckwalter JA MH. Articular cartilage. Part i :Tissue design and chondrocyte-matrix interactions. Part ii :Degeneration and osteoarthrosis, repair, regeneration, and transplantation. J Bone Joint Surg 1997;79A:600-32. [ Links ]
15. Asik M, Ciftci F, Sen C, Erdil M, Atalar A. The microfracture technique for the treatment of full-thickness articular cartilage lesions of the knee: midterm results. Arthroscopy 2008;24:1214- 20. [ Links ]
16. Gomoll AH, Farr J, Gillogly SD, Kercher J, Minas T. Surgical management of articular cartilage defects of the knee. J Bone Joint Surg Am 2010;92:2470-90. [ Links ]
17. Knutsen G, Drogset JO, Engebretsen L et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 2007;89:2105-12. [ Links ]
18. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 2003;19:477-84. [ Links ]
19. Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM. Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord 2006;7:38. [ Links ]
20. Ware JE, Kosinski M, Keller SK. SF-36® Physical and Mental Health Summary Scales: A User's Manual. Boston, MA: The Health Institute, 1994. [ Links ]
21. Becher C, Kalbe C, Thermann H et al. Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 2011;131:1135-43. [ Links ]
22. Bollars P, Bosquet M, Vandekerckhove B, Hardeman F, Bellemans J. Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 2011. [ Links ]
23. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)- development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998;28:88-96. [ Links ]
24. Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473-83. [ Links ]
25. Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB. Validation of the Knee Injury and Osteoarthritis Outcome Score (KOOS) for the treatment of focal cartilage lesions. Osteoarthritis Cartilage 2009;17:1434-39. [ Links ]
26. Irrgang JJ, Anderson AF, Boland AL et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 2001;29:600-13. [ Links ]
27. Kellgren J, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. [ Links ]
28. Guermazi A, Hunter DJ, Roemer FW. Plain radiography and magnetic resonance imaging diagnostics in osteoarthritis: validated staging and scoring. J Bone Joint Surg Am 2009;91 Suppl 1:54-62. [ Links ]
29. Buckwalter JA, Mankin HJ, Grodzinsky AJ. Articular cartilage and osteoarthritis. Instr Course Lect 2005;54:465-80. [ Links ]
30. LaPrade RF, Botker JC. Donor-site morbidity after osteo-chondral autograft transfer procedures. Arthroscopy 2004;20:69-73. [ Links ]
31. Zaslav K, Cole B, Brewster R et al. A prospective study of autologous chondrocyte implantation in patients with failed prior treatment for articular cartilage defect of the knee: results of the Study of the Treatment of Articular Repair (STAR) clinical trial. Am J Sports Med 2009;37:42-55. [ Links ]
32. Bartlett W, Skinner JA, Gooding CR et al. Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a prospective, randomised study. J Bone Joint Surg Br 2005;87:640-45. [ Links ]
33. Harris JD, Siston RA, Pan X, Flanigan DC. Autologous chondrocyte implantation: a systematic review. J Bone Joint Surg Am 2010;92:2220-33. [ Links ]
34. Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am 2003;85-A:259-65. [ Links ]
 Correspondence:
Correspondence:
Dr M Posthumus
Tel: +27216504575
Fax: +27216867530
Email: michael.posthumus@uct.ac.za














