Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.12 no.4 Centurion dic. 2013
PAEDIATRIC
The effect of two different plastering techniques on the rate of major surgery in idiopathic clubfoot
A HornI; SI Dix-PeekII; EB HoffmanIII
IMBChB(Pret) Registrar, Department of Orthopaedics, University of Cape Town
IIMBChB(UCT), FCS(SA)Ortho Head of Paediatric Orthopaedics Red Cross Children's Hospital and Maitland Cottage Paediatric Orthopaedic Hospital, Department of Orthopaedics, University of Cape Town
IIIMBChB(UCT), FCS(SA)Ortho Associate Professor (retired)
ABSTRACT
BACKGROUND: The Ponseti technique of clubfoot manipulation and casting is reported to have almost eliminated the need for extensive surgery (posterior and posteromedial release) and surgical decision-making is now largely based on clinical assessment, as opposed to pre-operative radiographs. The Ponseti method of manipulation and casting was introduced at our institution in 2002, prior to which we used the Kite method. Both prior to, and following the introduction of Ponseti casting, surgical decision-making was based on pre-operative radiology, and intra-operative clinical assessment.
METHODS: A retrospective comparative study was performed to compare the incidence of radical surgery following the use of the Kite method versus the Ponseti method. In addition, the accuracy of measured radiographic parameters in predicting which surgery was to be performed was investigated.
RESULTS: The incidence of radical surgery decreased from 40% with the Kite method to zero with the Ponseti method. Of the four routinely measured radiographic angles, only the tibiocalcaneal angle and the talometatarsal angle significantly correlated with the extent of surgery performed.
CONCLUSIONS: Using the Ponseti method greatly decreases the need for radical surgery in idiopathic clubfoot. Radiographic measurements do not influence surgical decision-making significantly.
Key words: clubfoot, Ponseti, posteromedial release, radiographic, angles
Introduction
Most orthopaedic surgeons agree that the initial treatment for idiopathic clubfoot should consist of gentle manipulation and serial casting, with surgery being reserved for resistant and relapsed feet.1-3 Many methods of manipulation and casting have been described, with varying degrees of success.
Kite described a technique whereby forefoot adduction was corrected first by abduction, using the calcaneocuboid joint as a fulcrum. Once this was corrected, the heel could be everted and lastly, the equinus corrected.4,5 Although Kite advocated conservative treatment with casting and even wedging of casts, most surgeons performed either a posterior release (PR)6,7 or a posteromedial release (PMR) for residual deformity based on clinical and/or radiographic evaluation.8-10
Ponseti revolutionised the treatment of clubfoot with the publication of his method in 1963.11 Based on thorough understanding of the three-dimensional patho-anatomy of the clubfoot, he developed his treatment principles. He emphasised that the cavus deformity is caused by pronation of the forefoot in relation to the hindfoot, and should be corrected first in order to realign the foot. He also stated that abduction of the forefoot should occur around the head of the talus, not at the calcaneocuboid joint, as this manoeuvre would successfully unlock the calcaneus from under the talus, allowing dorsiflexion to be achieved, usually with the aid of a percutaneous Achilles tenotomy.1,11,12 The indication for Achilles tenotomy was assessed clinically without radiographs. Pirani subsequently described a clinical classification which is now routinely used.13
Ponseti reported 74% good to excellent results using this method, although 40% of patients required Achilles tendon lengthening, and 46% tibialis anterior transfer for dynamic forefoot varus, the tibialis anterior transfers performed after the age of 2.5 years.14 Subsequent studies showed superior results to previous methods with the need for radical surgery being almost completely eliminated.
Many methods of manipulation and casting have
been described, with varying degrees of success
Some controversy still exists around the performance of a PMR as primary surgical intervention for idiopathic clubfoot. Many authors believe that even though PMR leads to correction of the anatomical deformity on radiographs, and has excellent short-term results, it leads to considerable stiffness of the foot and ankle at late follow-up, and recurrences as well as overcorrections are frequently observed.1,12,15 Other authors have found that patients undergoing PMR primarily have less need for subsequent operations16 and also better outcomes, as evidenced by better muscle strength, less hindfoot varus and less subtalar stiffness, when compared to patients who had minor surgical procedures.16,17 Turco, who first described the PMR as we know it today, claimed a 83% good or excellent result at 15-year follow-up, and found the best results were achieved in patients who were operated between one and two years of age.8,18
In this study the Ponseti method of treatment for idiopathic clubfoot was introduced in 2002. Prior to this, serial manipulation and casting was performed in the method described by Kite.5 PMR was performed on those feet that displayed inadequate talocalcaneal divergence (<20°) on pre-operative radiographs, or intra-operatively, where persistent cavus and hindfoot varus was evident after posterior release had been performed. It was noted that since adopting the Ponseti method of manipulation, the rate of major surgery (PMR) as primary surgical intervention for idiopathic clubfoot, decreased significantly.
The purpose of this study is to quantify retrospectively the change in incidence of major surgery since the introduction of the Ponseti method. Additionally, the value of pre-operative radiographs was assessed as a tool for predicting the extent and complexity of surgery, i.e. PR vs PMR.
Patients and methods
A retrospective review of the clinical records and radiographs of all patients presenting to our clubfoot clinic was performed. Two cohorts were identified; those from 1999-2000 (pre-Ponseti) and those from 2009-2010 (Ponseti).The groups were chosen to represent patients preceding and following the introduction of a different plastering technique introduced in 2002. Patients were included in the study if they had idiopathic clubfoot, presented within the first three months of life and had received no prior treatment. Teratological clubfeet were excluded. Ethical approval was obtained from our institution's Research Ethics Committee.
In the pre-Ponseti group there were 60 patients with 85 clubfeet. There were 24 females and 36 males; 25 were bilateral, 19 were left-sided and 16 were right-sided. Average age at presentation was 4.2 weeks (range 1-12 weeks), average number of plasters applied was 9 (range 0-18). Average age at first surgery was 10.3 months (range 3-44).
In the Ponseti group there were 50 patients with 70 clubfeet. There were 16 females and 34 males; 20 cases were bilateral, 11 were left-sided, and 19 were right-sided. Average age at presentation was 4 weeks (range 0-12), average number of plasters applied was 7 (range 1-14). Average age at surgery was 6.7 months (range 3-18 months).
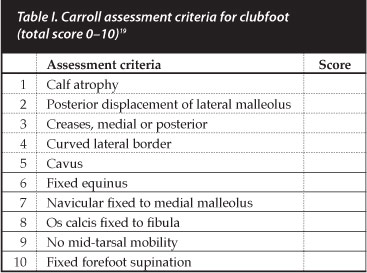
Radiographic parameters were measured in all cases where radiographs were available by a single investigator (AH). The angles measured were on the antero-posterior (AP) view, the talocalcaneal angle and the talometatarsal-I angle; and on the lateral view, the talocalcaneal and the tibiocalcaneal angle. All radiographs were performed in a standardised fashion as described by Simons,9 and were taken after the initial period of plaster casting, prior to surgery. Pre-operative clinical severity was quantified using the scoring system described by Carroll (Table I).19
Statistical analysis
The Chi-square test was performed to determine the significance of the change in rate of posteromedial release being performed as primary surgical intervention.
In order to determine the predictive value of pre-operative radiographs in determining whether major surgery was to be performed, the data from both cohorts were pooled. This follows the fact that surgical decision-making for both groups was performed either by, or under the supervision of the same surgeon (EBH). The patients were divided into three groups as follows: major surgery (PMR), minor surgery and no surgery. Analysis of variance (ANOVA) tests were performed on the data sets that were normally distributed, and if the data was not normally distributed, the Kruskal- Wallis test of significance was performed.
Results
In the pre-Ponseti group 34 of the 85 feet (40%) had a PMR as primary intervention. Posterior release (PR) was performed on 41 feet (48%); three feet (4%) were treated with a percutaneous tenotomy; and the remaining seven feet (8%) required no surgery. The average pre-operative Carroll score was 8 for the patients treated with PMR, and 2.8 for patients treated with PR or lesser surgeries.
In the Ponseti group, PMR was performed on no patients as primary surgical intervention. PR was performed on 32 feet (48%); 12 feet (17%) had formal elongation of the Achilles tendon (ETA); percutaneous tenotomy was performed on two feet only (3%); 18 feet (26%) required no surgery; and four patients were lost to follow up after initial presentation. The average Carroll score for patients undergoing PR was 3.8 and for patients undergoing ETA 2.4.
The decrease in the rate of major surgery was found to be highly statistically significant using the Chi-square test (p<0.002). In addition the average Carroll score decreased from 6.8 in the pre-Ponseti group to 3.4 in the Ponseti group.
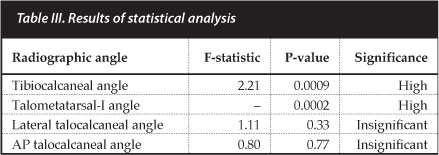
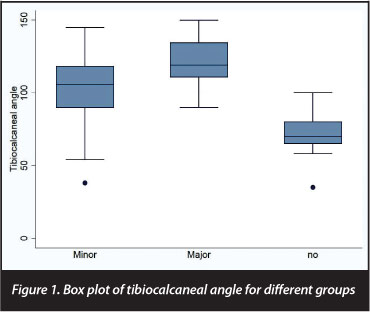
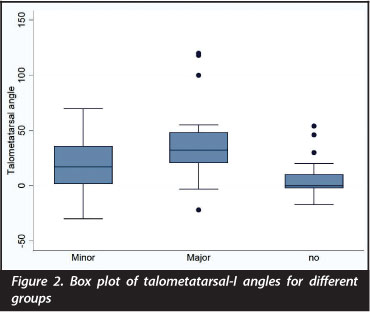
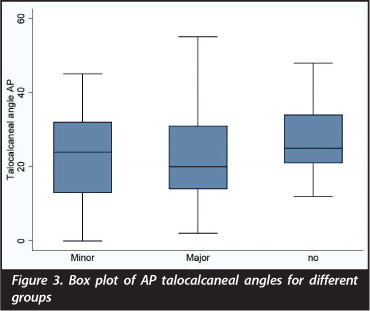
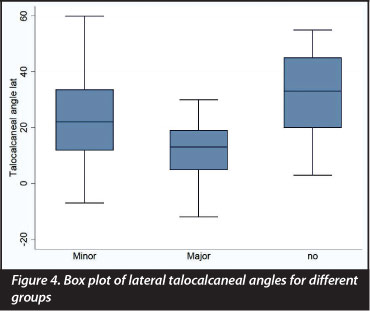
The average measured radiographic angles for the different surgical groups are summarised in Table II, and the results of the statistical analysis in Table III. The oneway analysis of variance was determined for all angles except the AP talometatarsal-I angle, for which the Kruskal-Wallis test was performed, as the data for this angle was not normally distributed. A p-value of 0.05 was chosen as the cut-off for significance. Graphic illustration of the distribution of measured angles in the different groups is provided in Figures 1-4.
Discussion
In this study, the average pre-operative Carroll score changed from 6.8 to 3.4 after the introduction of the Ponseti plastering technique. In addition, and more clinically relevant, 40% of patients in the group treated with the traditional manipulation and casting technique required PMR as primary intervention, whereas in the Ponseti group, not one PMR was performed as initial surgical intervention for idiopathic clubfoot. This result was found to be highly statistically significant using the Chi-square test (p<0.002).
Herzenberg et al previously compared the rate of PMR between patients treated by traditional means to those treated with a strict Ponseti protocol. In his control group, 32 out of 34 patients required PMR, in the Ponseti group, only one PMR was performed in 34 patients, and this was after multiple recurrences due to persistent non-compliance with abduction bracing. At follow-up, he also noted significantly decreased subtalar and ankle motion in the group treated with early PMR.2
In their review of 70 patients treated with strict Ponseti protocol including bracing, Firth et al found a very low rate of major surgery (7%) and only a 23% recurrence rate requiring repeat bracing. Included in this study were teratological clubfeet.20
In this study, in the Ponseti group, not one PMR
was performed as initial surgical intervention
for idiopathic clubfoot
In contrast to these findings, in a similar review by Molteno and Colyn, 897 idiopathic clubfeet treated from 1978-2003 were evaluated. In their study the rate of PMR as primary surgical intervention, decreased from 85.1% to 64.5% after changing plastering techniques from the Kite method to the Ponseti method. They stated that this relatively high rate of major surgery is attributed to the nature of the patients attending their clinic, noting that patients had to travel hundreds of kilometres to attend the clinic, and that compliance was low, therefore necessitating more radical intervention at an earlier stage.21 The pre-operative criteria for determining the degree of surgery to be performed was not included in this study.
Radiography
The talocalcaneal angle, on both the AP and lateral projections, is the most commonly quoted radiographic measure in clubfoot literature and is thought to be a measure of correction of hindfoot varus. Simons wrote extensively on the subject and found that a combination of an AP talocal-caneal angle of less than 15° and a talometatarsal-I angle of more than 15° always indicated the presence of talonav-icular subluxation.9 In our study, neither the AP nor the lateral talocalcaneal angle were found to be significantly related to the degree of surgery performed. This is in agreement with Radler et a/,3 who noted a poor correlation between these two angles and clinical severity as measured using the Pirani13 and Diméglio22 scores. Contrary to this, several authors, including Laaveg,1 Ponseti and Turco8 found the lateral talocalcaneal angle to be a good indicator of clinical severity. Thompson et a/ concluded that of all radiographic measures, the lateral talocalcaneal angle had the best correlation with clinical severity and the AP talocal-caneal angle the worst.16
In our study, both the tibiocalcaneal
angle and the AP talometatarsal-I angle were
significantly related to the degree of surgery performed
In our study, both the tibiocalcaneal angle and the AP talometatarsal-I angle were significantly related to the degree of surgery performed.
The talometatarsal-I angle is a measure of forefoot adduction and normal ranges vary with age23 but is generally considered to 0° to -20°, with any positive value considered abnormal.9 The tibiocalcaneal angle is measured on the lateral projection between a line parallel with the axis of the tibia and a line parallel with the plantar surface of the calcaneus, and is indicative of the degree of hindfoot equinus. This angle measures 25°-60° in normal feet and was also found to correlate well with the Pirani and Diméglio scores respectively by Radler et al.3
Herbsthofer et al performed a statistical analysis in order to determine the significance of radiographic measurements in clubfoot. They found that clubfeet did have on average a smaller talocalcaneal (TC) angle (AP and lateral) but due to high standard deviations, definite assignment of angle measurements to healthy feet or clubfeet was not possible. They also felt that a differentiated distribution of clubfoot change according to degrees of severity based on the TC angle would make no sense. They concluded that the routine use of radiographic studies in the diagnosis, classification and follow-up of clubfoot does not appear to be a useful tool in view of the wide range of deviation of values within individual clinical groups.24 Radler et al concluded that, although there was generally poor correlation between radiographic measurements and clinical severity in clubfoot, X-rays were useful in diagnosing pseudo-correction and aiding decision to do a tenotomy.3 In our study, even though there was correlation between the tibiocalcaneal angle and the talometatarsal-I angle, radiography did not supersede the value of clinical evaluation in deciding the need for surgery and the extent thereof.
We conclude that, based on our results and a review of the current literature, the Ponseti method of casting significantly reduces the need for major surgery in the treatment of idiopathic clubfoot, compared to traditional methods.
We also suggest that the use of routine radiographs in the treatment of clubfoot does not appear to contribute to decision-making and is therefore not justified.
The content of this article is the sole work of the authors. No benefits of any form have been or are to be received from a commercial party related directly or indirectly to the subject of this article. The research has been approved by the Research Ethics Committee, Health Sciences Faculty, University of Cape Town (ref: 349/2008).
References
1. Laaveg SJ. Long-term results of treatment of congenital club foot. Journal of Bone and Joint Surgery [Am] 1980;62(1):23-31. [ Links ]
2. Herzenberg JE. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop 2002;22(4):517-21. [ Links ]
3. Radler C. Radiographic evaluation of idiopathic clubfeet undergoing Ponseti treatment. Journal of Bone and Joint Surgery [Am] 2007;89(6):1177-83. [ Links ]
4. Fripp AT, Shaw NE. Club-foot. 1st ed. London: E. & S. Livingstone; 1967. [ Links ]
5. Kite JH. The Clubfoot. 1st ed. New York: Grune & Stratton, Inc.; 1964. [ Links ]
6. Attenborough G. Early posterio soft-tissue release in severe congenital talipes equinovarus. Clinical Orthopaedics and Related Research 1972;3(1):10-21. [ Links ]
7. Hudson I. Posterolateral release for resistant club foot. Journal of Bone and Joint Surgery [Br] 1994;76(2):281-84. [ Links ]
8. Turco VJ. Surgical correction of the resistant club foot one-stage posteromedial release with internal fixation: A preliminary report. Journal of Bone and Joint Surgery [Am] 1971;53(3):477-87. [ Links ]
9. Simons GW. Analytical radiography of club feet. Journal of Bone and Joint Surgery [Br] 1977;59(4):485-90. [ Links ]
10. Beatson TR. A method of assessing correction in club feet. Journal of Bone and Joint Surgery [Br] 1966;48(1):40-50. [ Links ]
11. Ponseti IV, Smoley EN. Congenital clubfoot: The results of treatment. Journal of Bone and Joint Surgery [Am] 1963 March;48-A(2):261-344. [ Links ]
12. Ponseti IV. Treatment of congenital club foot. Journal of Bone and Joint Surgery [Am] 1992 March;74-A(3):448-54. [ Links ]
13. Pirani S. A reliable and valid method of assessing the amount of deformity in the congenital clubfoot deformity. Journal of bone and joint surgery [Br] 2008;90( Suppl 1):53. [ Links ]
14. Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital clubfoot. Journal of Bone and Joint Surgery [Am] 1980;62-A(1):23-31. [ Links ]
15. Cooper DM. Treatment of idiopathic clubfoot. A thirty-year follow-up note. Journal of Bone and Joint Surgery [Am] 1995;77(10):1477-89. [ Links ]
16. Thompson GH, Richardson AB, Westin GW. Surgical management of resistant congenital talipes equinovarus deformities. Journal of Bone and Joint Surgery [Am] 1982;64(5):652-65. [ Links ]
17. Haasbeek JF. A comparison of the long-term results of posterior and comprehensive release in the treatment of clubfoot. J Pediatr Orthop 1997;17(1):29-35. [ Links ]
18. Turco VJ. Resistant congenital club foot - one-stage postero-medial release with internal fixation. A follow-up report of a fifteen-year experience. Journal of Bone and Joint Surgery [Am] 1979;61(6A):805-14. [ Links ]
19. Carroll NC, McMurty R, Leete SF. The pathoanatomy of congenital clubfoot. Orthopedic clinics of North America 1978;9(1):225-32. [ Links ]
20. Firth G, Eltringham M, Shnier G. Early results of the Ponseti technique for a clubfoot clinic in South Africa. South African Orthopaedic Journal 2009;8(Summer):67-72. [ Links ]
21. Molteno R, Colyn S. The treatment of idiopathic clubfoot: A comparison of two methods of manipulative treatment. South African Orthopaedic Journal 2005;4(May):12-18. [ Links ]
22. Diméglio A, Bensahel H, Souchet PH et al. Classification of Clubfoot. J Pediatr Orthop B;1995;4(2):129-36. [ Links ]
23. Vanderwilde R, Stahelli LT, Chew DE et al. Measurements on radiographs of the foot in normal infants and children. Journal of Bone and Joint Surgery 1968;70-A(3):407-15. [ Links ]
24. Herbsthofer B. Significance of radiographic angle measurements in evaluation of congenital clubfoot. Arch Orthop Trauma Surg 1998;117(6):324-29. [ Links ]
 Correspondence:
Correspondence:
Dr Anria Horn
Postnet Suite 342
Private Bag X18
Rondebosch 7701
Cape Town
Cell: 071 679 4228
Work: 021 404 5108
Email: anriahorn@gmail.com














