Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.12 n.4 Centurion Dec. 2013
PAEDIATRIC
The epidemiology of femur shaft fractures in children
MA MughalI; SI Dix-PeekII; EB HoffmanIII
IMD. Registrar
IIMBChB, FCS(SA)Orth, MMed. Consultant
IIIMBChB, FCS(SA)Orth. Associate Professor. Red Cross War Memorial Children's Hospital, and the Department of Orthopaedic Surgery, University of Cape Town
ABSTRACT
Femur shaft fractures constitute 21.9% of the orthopaedic fractures seen in our unit. The epidemiology is well described in literature from developed countries. To assess the epidemiology in a developing country and to identify socio-demographic risk factors, we did a retrospective study of 759 children with femur fractures treated over a 5-year period. We utilised the Census of 2011 to calculate the annual incidence. The socio-economic status was determined by means of a social deprivation category based on the parental occupation obtained from the Census as per the parental address.
The mean annual incidence of 152 patients with femur fractures extrapolated to 0.25 per 1 000 children per year. The commonest mechanism of injury was a fall (39%) with a peak at 2 to 3 years of age, followed by motor vehicle accident (MVA) (33.7%), of which 88% were pedestrian (PVA). Ninety per cent of the patients were from the lowest two socioeconomic classes. The peak incidence at 4 to 5 years due to a PVA was younger than the >6 years reported from developed countries. Children at 4 to 5 years have not developed the cognitive and perceptuo-motor abilities to adapt to a traffic environment. The peak of 4 to 5 years due to PVAs is the result of lack of guided parental training, adequate supervision and play area in the lower socio-economic classes.
In children <1 year of age, 59.3% were due to non-accidental injury (NAI) and 23.7% due to osteogenesis imperfecta.
Key words: epidemiology, femur shaft fractures, children
Introduction
Femoral shaft fractures as a group in children is the third most common orthopaedic fracture after forearm and elbow fractures seen in our paediatric tertiary hospital trauma unit. They are the most costly to treat and require the longest stay in hospital.1
The literature from developed countries (Scandinavia, United Kingdom and the United States) report a mean incidence of paediatric femur fractures of 0.2 per 1 000 per year, with a male:female ratio of 2:1 and a bimodal age distribution at 2 to 3 years and >6 years.2-7
Studies from the United States5 and England6 showed an eight and three times higher risk of femur fractures respectively in children from a deprived socio-economic group.
The purpose of this study was to assess the epidemiology of femur fractures in a tertiary paediatric hospital in a developing country, and attempt to identify socio-economic risk factors.
Methods
We retrospectively reviewed all patients with femur fractures that were treated at our unit in the 5-year period from January 2005 to December 2009. A total of 759 patients with 770 femoral shaft fractures (11 or 1.4% were bilateral) were identified. Femoral neck and intertrochanteric fractures, slipped upper femoral epiphyses, and distal femoral physeal fractures were excluded.
Data collected from records were age, gender, mechanism of injury, location of injury occurrence, residential suburb, and the method of treatment. In patients with suspected non-accidental injury (NAI), the diagnosis was preceded by a clinical examination, a skeletal survey, a CT brain and a thorough investigative interview by a social worker.
The annual incidence for the population was calculated utilising the Census of 2011. The socio-economic class was determined by means of a social deprivation category based on the parental occupation obtained from the Census as per parental address: class I, professional occupation; class II, managerial and technical occupation; class III, skilled occupation non-manual and manual; class IV, semi-skilled occupation; class V, unskilled occupation and unemployed.8
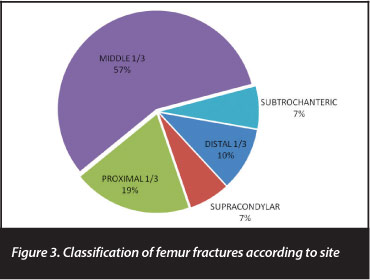
All radiographs were reviewed by the primary author and fractures classified as subtrochanteric (within 2 cm below the lesser trochanter), proximal third shaft, middle third shaft, distal third shaft, and supracondylar (the distance from the centre of the fracture to the knee joint was equal to or less than the width of the condyles).
The 95% confidence interval was used to statistically estimate the validity of the data.
Results
Incidence
The mean incidence of femoral shaft fractures was 21.9% (152 patients) of all patients with orthopaedic fractures (rib and skull fractures excluded) treated in our unit annually (Table I). All patients with femur shaft fractures were admitted.
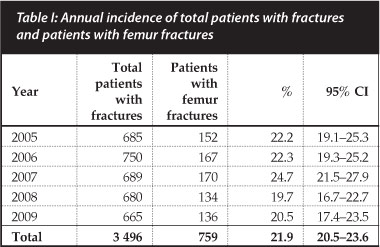
According to the 2011 Census, the population of our province was 5.8 million. The two tertiary hospitals in the province serve about 80% of the population, of which 1.2 million are <14 years old. We therefore serve about 600 000 children. This extrapolates to an incidence of 0.25 femur shaft fractures per 1 000 children per year.
Gender
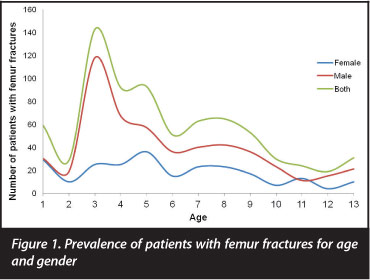
Our study showed a male:female ratio of 2.2:1. Figure 1 shows the male:female ratio for age. In patients <1 year where 59.3% of the femur fractures were due to NAI, the incidence was similar for both genders.
We serve about 600 000 children, which extrapolates to 0.25 femur shaft fractures per 1 000 children per year
Mechanism and age
The mechanisms of injury are given in Table II. The commonest mechanism was a fall (39%). Eighty-eight per cent of falls occurred at home.
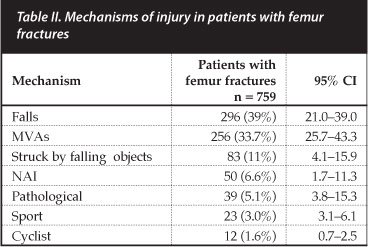
Motor vehicle accidents (MVAs) were responsible for 33.7% of fractures, of which 88% were pedestrians (PVAs). Of all the patients, only 1.6% were cyclists.
In 11% the patients were struck by falling objects ranging from falling shack roofs to collapsing gates and doors. The majority occurred in the 'safe' home environment.
Non-accidental injury (NAI) was the cause of 50 (6.6%) fractures. Seventy per cent (35 of 50) were <1 year old. Fifty-nine fractures occurred <1 year of age, therefore the chance of a femur fracture <1 year being due to NAI was 59.3% (35 of 59).
Pathological fractures occurred in 39 patients (5.1%). Twenty were due to cerebral palsy, 14 to osteogenesis imperfecta, three to a non-ossifying fibroma and two were subtrochanteric fractures due to fibrous dysplasia.
Sports-related injuries were responsible for 35 (4.6%) fractures.
The age at presentation varied from 1 day (traumatic femur fracture during childbirth or osteogenesis imperfecta) to 12 years of age, which is the upper age limit for patients seen at our institution. The mean age was 4.9 years and the median age was 3.6 years.
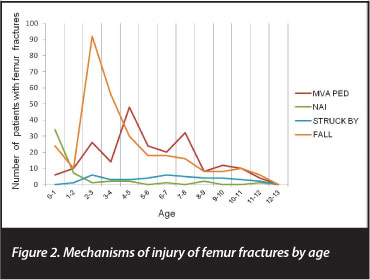
Figure 2 shows the incidence of the mechanism of injury for each age group. The peak incidence for fractures due to NAI was <1 year (70% of fractures <1 year); a fall 2 to 3 years (median age 3 years); and a PVA 4 to 5 years (median age 4 years). The median age of patients struck by falling objects was 4.8 years and of patients with sport-related injuries was 5 years.
Socio-economic status
Ninety per cent of our patients were from families of the lowest socio-economic classes IV and V (occupation of the parents were semi-skilled, unskilled or unemployed).8
Fracture location and treatment
Figure 3 shows the classification of the fractures according to site.
The method of treatment was determined by the age of the patient, the classification or site of the fracture, the type of fracture, and the presence of associated injuries. A spica was used in 40.3%; traction in a Thomas splint in 33%; gallows or Pavlik harness in 8.4%; intramedullary titanium nails in 7.8%; 5.4% percutaneous pin fixation; 2.5% POP only for supracondylar fractures; and 2.6% were plated.
Discussion
Incidence
Femoral shaft fractures as a group is the third most common orthopaedic fracture (21.9%) treated at our unit after forearm fractures (27%) and elbow fractures (24%). Our annual incidence of 0.25 per 1 000 of the childhood population is more than the 0.19 reported from the United States in 1999 by Hinton et al,5 but comparable to the 0.28 reported from Denmark in 1992 by Nafei et al,4 and the 0.22 reported from England by Bridgman and Wilson in 2004.6 Bridgman et al6 report a decrease of 0.33 in 1991 to 0.22 in 2001, and von Heideken et al7 from Sweden a decrease of 0.19 in 1987 to 0.11 in 2005. They ascribe this to reduced physical activity and improved safety in the playground and traffic environment. The absence of an increased incidence in our study from 2005 to 2009 (Table I) with an increase in population of the province from 4.5 million in 2001 to 5.8 million in 2011 suggests a decreased incidence of femur fractures.
The male:female ratio of 2.2:1 is similar to other studies.3,5,6,7,9 This probably reflects the increased risk of boys for all fractures due to higher-risk play activities being more acceptable for boys.5,6,9 This is further supported by the equal gender incidence in NAI (Figure 1), which is not activity related.
Age and mechanism
The bimodal age distribution of 2 to 3 years for falls and >6 years for MVA, is well described in the literature. The first peak due to falls occurs universally at 2 to 3 years.3-7,9 Fall (39%) was the commonest mechanism of injury in our study with a peak in the toddler aged 2 to 3 years. Three reasons are given why a low energy mechanism does not result in a femur fracture in an older child, but results in a fracture in a toddler. In the toddler the femoral cortical thickness is decreased due to more woven bone vs lamellar bone. This remodels in the older child so that the cortical thickness increases in relation to the canal with increase in bone strength.1 In toddlers physical capabilities outpace judgment skills and protective reflexes are not fully developed.5 This is the reason why forearm fractures are more common in the older child where the outstretched arm is a reflex protection mechanism.5
The age of the second peak due to MVAs varies. Hinton et al5 describe a peak incidence due to PVAs at 6 to 9 years and another peak due to passenger MVAs in teenagers (14 to 17 years). Bridgman et al6 describe a peak due to MVAs at 6 to 10 years, but does not differentiate between pedestrians and passengers. Loder et al9 describe peaks due to PVAs and cyclist injuries at 6 to 12 years, and MVA passengers in teenagers.
The peak of 4 to 5 years for a femur fracture due to an MVA in our study is younger than the >6 years described in the literature.5,6,9 In a study of all orthopaedic injuries due to road traffic accidents in Johannesburg, Pretorius and Firth found a similar peak at age 5 years.10
The common scenario is the child in a residential area not far from his or her home who played outside or returned from school and dashed into the street often between parked cars. The driver involved claims that he or she did not see the child and nothing could be done to avoid the accident. There is controversy whether counter measures should improve the road-user behaviour of the children or alter the traffic conditions to suit the children. Children imagemaqui<8 years have not yet developed the cognitive and perceptuo-motor abilities to adapt to a traffic environment.11-13 Their road-crossing incompetence is due to a decreased capacity to appreciate the interrelationships between duration, velocity and distance plus lapses of attention leading to overcautious or delayed crossing. Parental accompaniment and parental guided training in realistic traffic situations have been shown to decrease PVAs in children.12 We believe that the younger peak of 4 to 5 years in our society reflects absence of parental training and the tendency of children from a deprived social class to play in the road unsupervised because of an inadequate playing area.
Ninety per cent of the patients in the study were from the lowest socio-economic classes (class IV and V). Studies from the USA5 showed an eightfold increased incidence and from the UK6 a threefold increased incidence of femur fractures in the lowest socio-economic groups compared to children from the highest income areas. These low socio-economic areas are overcrowded and lack protected play areas. The head of the family is often a single parent who works and therefore the child lacks guided traffic training and trained supervision. Hinton et at5 showed that a low socio-economic level and greater crowding of housing structures were the strongest predictors of fractures.
An informal review of private hospitals in our area suggests a significantly lower incidence of femur fractures in children. This supports our conclusion that lack of guided training, supervision and play areas in the lower socioeconomic groups is the main cause of PVAs.
Non-accidental injury (NAI)
Long bone fractures in our unit only constitute 5% of the injuries in NAI. Sexual abuse, soft tissue and head injuries predominate. Femur fractures are the commonest long bone fractures in NAI.14 King et at14 from the USA found that 42% and Theunissen et at15 found that 50% of long bone fractures in NAI were femur fractures. They also found that 60.5% and 72% respectively occurred in infants <1 year old. In the current study 70% (35 of 50) of patients with femur fractures due to NAI were <1 year old.
The incidence of patients with femur fractures due to NAI in our study was 6.6%. This is much higher than the1.2% in the Bridgman et at study from England6 and the 0.28% in the von Heideken et at study from Sweden.7 This Swedish study with only 4.2% of femoral fractures <1 year due to NAI is the lowest ever reported. They put it down to the fact that Sweden was the first country to ban corporal punishment. The likelihood of a child <1 year with a femur fracture in our study being due to NAI is 59.3% (35 of the 59 fractures <1 year), which is more in line with the study from the USA by Schwend et at who showed that the likelihood of a non-walking infant <1 year old with a femur fracture being caused by abuse was 42%, but in a walking toddler 1 to 4 years of age, the likelihood was only 2.6%.16
Pathological fractures
The commonest causes of pathological fractures were insufficiency fractures due to cerebral palsy (20 of 39) and osteogenesis imperfecta (14 of 39).
Five of the 20 wheelchair-bound total body cerebral palsy patients (Gross Motor Function Classification System level V) with fractures had 'institutionalised rickets'. This is due to a combination of factors:17 lack of sunlight, dietary vitamin D and calcium. Anticonvulsant therapy also induces hepatic enzymes that enhance the degradation of vitamin D precursors in the liver. A patient with a pathological femur fracture in cerebral palsy should have rickets excluded. Maree et at have shown that after the acute treatment of the rickets a multifactorial approach of increased exposure to sunlight, increased calcium intake and changing from enzyme-inducing anti-convul-sants prevents further fractures.17 Bischof et at18 however, advise lifelong vitamin D supplementation to all institutionalised patients, and others have shown an increase in bone mineral density (BMD) and decreased fracture incidence in these patients with bisphosphonate treatment.19
Ninety per cent of the patients in the study were from the lowest socio-economic classes who live in areas that are overcrowded and lack protected play areas
In a retrospective study from our unit of 32 patients with osteogenesis imperfecta treated over a 20-year period, all the patients had femur fractures and the first fracture always occurred under 1 year of age (38% perinatally).15 In the current study therefore, of the 59 femur fractures <1 year old, 35 (59.3%) were due to NAI and 14 (23.7%) due to osteogenesis imperfecta. The other 17% of femur fractures <1 year were due to accidental trauma. The differential diagnosis of osteogenesis imperfecta and NAI can be challenging.20,21 Most of the patients with osteoge-nesis imperfecta are severely affected and have obvious radiological signs of osseous fragility (osteopaenia, antero-lateral bowing of femurs and tibiae, and thin or gracile long bones). In mild cases without signs of bone fragility, a family history and blue sclera in type I, a family history and normal sclera in type IV, and Wormian bones in all types can help with the diagnosis.15
Limitations of this retrospective study are that the Census only supplies figures for children <14 years of age, while our unit only treats patients <12 years old. We assume that the patient distribution is equal between the two tertiary hospitals. There are also no accurate figures for private patients.
Conclusions
In children under the age of 1 year 59.3% of femur fractures are due to NAI, and 23.7% due to osteogenesis imperfecta. The peak of 4 to 5 years due to PVAs is mainly due to lack of guided parental training, adequate supervision and play areas in the lower socio-economic classes.
The content of this articte is the sote work of the authors. No benefits of any form have been or are to be received from a commerciat party related directly or indirectly to the subject of this articte. The research has been approved by the Research Ethics Committee, Heatth Sciences Facutty, University of Cape Town (reef: 292/2010).
References
1. Beaty JH, Kasser JR. Femoral Shaft Fractures. In: Beaty JH, Kasser JR, (eds). Rockwood and Wilkins' Fractures in Children. Lippincott Williams and Wilkins;2006:894-936. [ Links ]
2. Gross RH, Stranger M. Causative factors responsible for femoral fractures in infants and young children. J Pediatr Orthop 1983;3:341-43. [ Links ]
3. Hedlund R, Lindgren U. The incidence of femoral shaft fractures in children and adolescents. J Pediatr Orthop 1986;6:47-50. [ Links ]
4. Nafei A, Teichert G, Mikkelsen SS, Hvid I. Femoral shaft fractures in children: an epidemiological study in a Danish urban population, 1977-1986. J Pediatr Orthop 1992;12:499-502. [ Links ]
5. Hinton RY, Lincoln A, Crockett MM, Sponseller P, Smith G. Fractures of the femoral shaft in children. J Bone Joint Surg [Am]1999;81-A:500-509. [ Links ]
6. Bridgman S, Wilson R. Epidemiology of femoral fractures in children in the West Midlands region of England 1991 to 2001. J Bone Joint Surg[Br]2004;86-B:1152-57. [ Links ]
7. von Heideken J, Svensson T, Blomqvist P et al. Incidence and trends in femur shaft fractures in Swedish children between 1987 and 2005. J Pediatr Orthop 2011;31:512-19. [ Links ]
8. Sharma S, Sibinski M, Sherlock DA. A profile of Perthes' disease in greater Glascow. J Bone Joint Surg[Br]2005;87- B:1536-40. [ Links ]
9. Loder RT, O'Donnell PW, Feinberg JR. Epidemiology and mechanisms of femur fractures in children. J Pediatr Orthop 2006;26:561-66. [ Links ]
10. Pretorius CJ, Firth GB. Road traffic accidents and orthopaedic injuries in children. SAOJ Spring 2010:65-68. [ Links ]
11. Demetre JD, Lee DN, Thompson JA et al. Errors in young children's decisions about traffic gaps: experience with roadside simulation. Br J Psych 1992:83:189-202. [ Links ]
12. Assailly JP. Characterization and prevention of child pedestrian accidents: an overview. J Applied Dev Psych 1997; 18:257-62. [ Links ]
13. Demetre JD. Applying developmental psychology to children's road safety: problems and prospects. J Applied Dev Psych 1997;18:263-70. [ Links ]
14. King J, Diefendorf D, Apthorp J et al. Analysis of 429 fractures in 189 battered children. J Pediatr Orthop 1988;8:585-89. [ Links ]
15. Theunissen HB, Dix-Peek S, Hoffman EB et al. The differential diagnosis of non-accidental injury from osteogenesis imperfecta in small children. Paper presented at SAOA congress September 2002. [ Links ]
16. Schwend RM, Werth C, Johnston A. Femur shaft fractures in toddlers and young children: rarely from child abuse. J Pediatr Orthop 2000:20:475-81. [ Links ]
17. Maree M, Dix-Peek S, Hoffman EB. The treatment and prevention of pathological fractures due to rickets in children with quadriplegic cerebral palsy and mental retardation. SAOJ May 2006:56-60. [ Links ]
18. Bischof F, Basu D, Pettifor JM. Pathological long-bone fractures in residents with cerebral palsy in a long-term care facility in South Africa. Dev Med Child Neurol 2002;44:119-22. [ Links ]
19. Sholas MG, Tann B, Gaebler-Spira D. Oral bisphosphonates to treat disuse osteopenia in children with disabilities: a case series. J Ped Orthop 2005;25:326-31. [ Links ]
20. Ablin DS, Greenspan A, Reinhart M, Grix A. Differentiation of child abuse from osteogenesis imperfecta. AJR 1990;154:1035- 46. [ Links ]
21. Ablin DS, Sane SM. Non-accidental injury: confusion with temporary brittle bone disease and mild osteogenesis imperfecta. Pediatr Radiol 1997;27:111-13. [ Links ]
 Correspondence:
Correspondence:
Prof EB Hoffman
7 Marne Avenue Newlands 7700
Cape Town, South Africa
Tel: +27 21 6718939 Email: teddie@absamail.co.za














