Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.12 no.3 Centurion Set. 2013
PAEDIATRIC
Ipsilateral medial and lateral condylar fracture of the humerus in a 4-year-old boy
Dr MA MoruleI ; Dr SS GoleleII; Prof RG GoleleIII
IMBChB(Medunsa) Registrar: Orthopaedics
IIMBChB(Medunsa), MMed(Ortho)(Medunsa), FCS(SA) Orthopaedic Consultant: Orthopaedics, Hand and Microsurgery
IIIMBChB(Natal), MFGP(CMSA), MMed(Orth)Medunsa, FC(Orth)SA Senior Consultant: Paediatrics, Tumour and Infection Unit
Dr George Mukhari Hospital (GMH), University of Limpopo Medunsa Campus, Ga-Rankuwa, South Africa
ABSTRACT
T-Condylar humeral fractures in children are rare. Medial condylar, lateral epicondylar, and T-condylar fractures combined, constitute less than 1% of all fractures in the elbow. Rarer is a T-condylar fracture in a skeletally immature child. We present a case of a T-condylar fracture in a 4-year-old boy following a fall on a flexed elbow.
Keywords: T-condylar, distal humerus, paediatric, fracture
Introduction
T-condylar humeral fractures are rare in skeletally immature children.1-5 Medial condylar, lateral epicondylar and T-condylar fractures combined, constitute less than 1% of all fractures in the elbow.6 They are also rare in adults, comprising 0.5% of all fractures.7 They may occur in association with other injuries, although rarely.
Little has been written about these fractures in this age group.3,4 Therefore dogmatic recommendation for the treatment of T-condylar fractures in this age group cannot be made because of limited experience.2,4,8 We present a case of a flexion injury type of T-condylar humeral fracture in a 4-year-old boy.
Case report
A 4-year-old boy was referred to us from a peripheral hospital. He had fallen onto his right flexed elbow. He was allegedly tripped by an older child while running (the patient's mother witnessed the incident). The elbow was swollen, deformed and tender. All distal pulses were palpable. The radial, median and ulnar nerves were clinically intact.
X-rays showed what the registrar on call termed ipsilateral medial and lateral mass fractures of the right elbow (Figures 1 and 2). A diagnosis of a closed T-condylar humeral fracture, flexion type, was made.


Within a week of admission the patient was taken to theatre. Under general anaesthesia, using direct lateral and medial approaches to the right elbow, with minimal dissection, the T-condylar fracture was reduced and internally fixed with smooth K-wires (Figures 3a, 3b). Postoperatively the patient was splinted with an above elbow backslab at 90 degrees flexion and supination. After three weeks the backslab was removed and active range of motion (ROM) exercises started with the help of a physiotherapist. The K-wires were removed 5 weeks post-operatively in theatre under general anaesthesia.


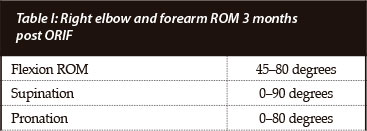
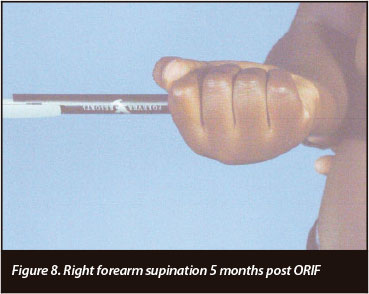
Table I and Figures 4 to 9 depict the patient's progress at follow-up. Right elbow flexion, extension and supination ROM at 5 months post-operatively were the same as at 3-months follow-up. Pronation at 5 months was 0-50 degrees.





Discussion
There are two types of T-condylar fractures: the flexion type and the extension type.5 The flexion type mostly represent wedge-type fractures as the anterior margin of the semilunar notch is driven into the trochlea by a fall on the posterior aspect of the elbow in more than 90 degrees of flexion.9 The extension type in this uncommon mechanism, a fall onto an outstretched upper extremity, results in a wedge fracture as the coronoid process of the ulna is driven into the trochlea.9 The fracture pattern in adolescents is similar to that in adults.5 Fractures in the young child may have a relatively intact distal humeral articular surface despite osseous displacement of the overlying condylar fragments because of the elasticity of the cartilage in the skeletally immature patient.9 Toniolo and Wilkins classify these fractures into three types,5 as follows: type I - the fracture is minimally displaced; type II - the fracture is displaced, with no comminution; type III - the fracture is displaced with comminution of the metaphyseal fragments. Our patient had a type II fracture.
X-rays are used in making the diagnosis. Anteroposterior (AP) and lateral views are the minimum. They should demonstrate the medial and lateral Thurston-Holland sign.2 This sign was demonstrated in our patient. Stress X-rays and/or an arthrogram under general anaesthesia are recommended to demonstrate the intra-articular component of the fracture.2,5 Similarly, magnetic resonance imaging (MRI) may be used.2,5 No MRI or arthrogram was done in our patient.
The T-condylar fracture was reduced and internally fixed with smooth K-wires
Fractures in the young child may have a relatively intact distal humeral articular surface despite osseous displacement of the overlying condylar fragments because of the elasticity of the cartilage in the skeletally immature patient
A type I fracture is treated with cast immobilisation. A type II fracture is treated with closed reduction and percutaneous K-wire fixation. Closed reduction is done using K-wires as joysticks.1,3 For type III and irreducible type II fractures surgical intervention with minimal dissection is indicated.2,5 In our patient the fracture fragments were widely separated and rotated and our primary goal for open reduction and internal fixation was to achieve anatomical alignment of the articular surface.
Various approaches to the elbow are described, with proponents for each.2,4,5,7,8,9,10 Three types of posterior approaches are recommended:
1. Triceps splitting approach:
• A V-shaped tendon flap of the triceps to restore the articular surface and a proper alignment of the physis.
• Possible disadvantages are that triceps division may result in strength loss or scarring which would compromise motion of the elbow joint2 and damage the physeal plates in children. Osada K et al2 recommend this approach for young patients.
2. Olecronon osteotomy:
• This approach is less technically demanding and provides maximal exposure but involves additional injury to the articular surface, and puts the patient at risk for displacement or non-union.
Olecranon osteotomy is generally not necessary for exposure and should be avoided.9
3. Postero-medial approach (Bryan-Morrey):
• This approach allows excellent exposure of the fracture and articular surface, decompression and mobilisation of the ulnar nerve, and the initiation of continuous passive motion (CPM).
We used a direct lateral and medial approach with minimal dissection and K-wire fixation.
Rehabilitation programmes in the literature include the following:
• Physiotherapy
• Continuous passive motion
• Use of axillary brachial blocks in adults6
In our patient only active ROM exercises were performed. Outcomes reported in the literature vary from poor to good.1-3 In a study by Re et al4 the outcome in 15 children who were treated surgically using different approaches was as follows:
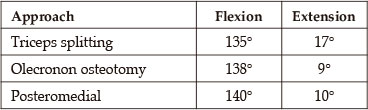
The olecranon osteotomy and the posteromedial approach both resulted in a statistically significant better final means of extension than did the triceps splitting approach. In another study by Osada et al, a 3-year-old patient was treated with an open reduction and internal flexion using the triceps splitting approach, and they reported a good functional outcome with no complaint of triceps weakness.2
Complications of T-condylar and other elbow fractures and their treatment are known and reported,4 such as osteonecrosis of the trochlea, loss of range of motion, neurovascular injury and growth arrest.
Our patient had two complications:
1. Decreased ROM. Right elbow flexion (45-80 degrees) and forearm pronation (0-50 degrees).
2. X-rays at 5 months follow-up showed sclerosis around the trochlea site, a suspicion of osteonecrosis.
The patient will need to be followed up for a longer period to evaluate the long-term outcome regarding osteonecrosis of the trochlea and the range of movement.
Conclusion
T-condylar fractures in skeletally immature children are rare. A high index of suspicion is needed for diagnosis of subtle T-condylar fractures. The following investigations are essential:
• X-rays, to demonstrate the medial and lateral Thurston-Holland sign.2
• Stress X-ray views and/or arthrogram under general anaesthesia, to demonstrate the intra-articular component of the fracture.2,5
More experience and literature reporting on these fractures are needed to guide treatment. Follow-up is needed in this patient as he is still young (4 years old).
No benefits of any form have been received from a commercial party related directly or indirectly to the subject of this article. The content of this article is the sole work of the authors.
References
1. Kanellopoulos AD, Yiannakopoulos CK. Closed reduction and percutaneous stabilization of pediatric T-condylar fractures of the humerus. Journal of Paediatric Orthopaedics. 2004;42:13-16. [ Links ]
2. Osada D, Tamai K, Saotome K. T-condylar fracture of the distal humerus in a three-year-old child. Hand Surgery. 2005;10(1):125-29. [ Links ]
3. Ruiz AL, David W, Kealey C et al. Percutaneous pin fixation of intercondylar fractures in young children. Journal Paediatric Orthopaedics Part B. 2001;10:211-13. [ Links ]
4. Re PR, Waters PM, Hresko T. T-condylar fractures of the distal humerus in children and adolescents. Journal of Paediatrics Orthopaedics. 1999;19:313-18. [ Links ]
5. Beaty JH, Kasser JR. Rockwood and Wilkins' Fractures in Children. 6th Edition. Pages 6592-658. [ Links ]
6. Staheli LT. Paediatric Orthopedic Secrets, 2nd Edition. Page 155. [ Links ]
7. Atalar AC, Demirhan M, Salduz A et al. Functional results of the parallel-plate technique for complex distal humerus fractures. Acta Orthop Traumatol Turc. 2009;43(1):21-27. [ Links ]
8. Sherr N, Bennet GC. Fractures of the elbow in children. Current Orthopaedics. 2001;15:206-13. [ Links ]
9. Egol KA, Koval KJ, Zukerman JD. Paediatric elbow in Handbook of Fractures. 4th Edition. Wolters Kluwer/Lippincott Williams and Wilkins. P625-628. [ Links ]
10. Morrissy RT, Weinstein SL. Management of fractures. In: Lovell and Winter's Paediatric Orthopaedics. Volume II. 5th Edition. Lipincott Williams and Wilkins. Pages 1344-50. [ Links ]
 Reprint requests:
Reprint requests:
Dr MA Morule
Dept of Orthopaedic Surgery.
PO Box 224. 0204 Medunsa
Tel: 012 521 4049
Email: Leonie.Strauss@ul.ac.za














