Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.12 n.2 Centurion Jan. 2013
EXPERT OPINION ON PUBLISHED ARTICLES
The relationship between displacement and clinical outcome after distal radius (Colles') fracture
Reviewer: Prof Ulrich Mennen
V Finsen, O Rod, K Rod, B Rajabi, PS Alm-Paulsen, H Russwurm, Faculty of Medicine, Norwegian University of Science and Technology and Department of Orthopaedic Surgery, St Olav's University Hospital, Trondheim, Norway Journal of Hand Surgery (European) 2012;38e(2):116-26
This article should be read by all orthopaedic surgeons who deal with upper-limb injuries, especially distal radius fractures of the Colles' type.
The authors treat over 500 Colles' fractures every year. They have analysed hundreds of patients after treatment with a follow-up of 2.5 to 12.7 years (mean 6.3 years), with the aim to correlate remaining deformity with function and pain. They have used numerous parameters to evaluate outcome vs. various anatomical measurements.
Their conclusions are:
1. Open surgery, i.e. ORIF with distal radius plates, has an 11% complication rate as opposed to closed reduction (1%).
2. ORIF of Colles' fractures do not result in better outcome and have a significantly higher incidence of pain.
3. Mal-union of Colles' fractures has little bearing on final outcome, i.e. there is no association between radiological displacement and clinical outcome.
4. Most symptoms of Colles' fractures will disappear after 2 years.
5. No parameter measured or circumstantial factor seems to constantly influence the outcome, or cause a specific complication.
6. Many patients who suffer from an acute Colles' fracture have most likely had previous upper limb injuries which are often not known or ignored. These past injuries have a detrimental effect on eventual outcome.
In the 'Discussion', this article brings home certain very important principles in Orthopaedic Surgery:
1. Much of our technical advances are not necessarily driven by improved results but often by commercial interests and the trade. Why do we have more than 30 different distal radius volar plates available to choose from?
2. There is a disturbing trend that deformities after injury should be exactly restored to within a fraction of a degree or millimetres using high tech equipment. Are we treating the X-rays? Have we lost the fact that we are dealing with biological, active, living tissue? Has technique indeed triumphed over reason? This article shows that surgery is not the ultimate or only method of treatment.
This article should be read by all orthopaedic surgeons who deal with upper-limb injuries,
3. What happened to the art of closed manipulation and applying a skilled cast? One sees very seldom correctly and neatly applied casts. Is it that the training of orthopaedic surgeons focuses more on surgical techniques and gadgets, and leaves the plaster application to a technician?
4. This article also points out that we may be over-treating patients; that expensive equipment and implants need not always be used, but that these costly expenses can better be used in other areas of medicine.
Treatment algorithms for chronic osteomyelitis
Reviewer: Dr LC Marais
Tumour, Sepsis and Reconstruction Unit Department of Orthopaedic Surgery University of KwaZulu-Natal Greys Hospital Pietermaritzburg Tel: (033) 897 3424 Leonard.Marais@kznh.ealth.gov.za
G Walter, M Kemmerer, C Kappler, R Hoffmann Dtsch Arztebl Int 2012;109(14):257-64. DOI: 10.3238/arztebl.2012.0257
Despite the advances in the management of chronic osteomyelitis over the past few decades, several crucial questions remain unanswered. In this recent review article the authors aim to elucidate the current concepts in management and attempt to provide an algorithm for the treatment of chronic osteomyelitis. The article recognises the fact that the absence of a uniform definition makes comparison of different diagnostic and treatment modalities virtually impossible. In addition the authors note the shortcomings of current classification systems and state that there is currently no generally accepted, interdisciplinary classification of osteomyelitis.
Appropriate emphasis is placed on the fact that there are currently no evidence-based guidelines in terms of the treatment of chronic osteomyelitis. The authors introduce the idea that the primary decision, when embarking on treatment, should be a choice between either a palliative or curative therapeutic pathway. This concept fits elegantly into the oncolog-ically oriented approach to chronic osteomyelitis that is currently evolving. Curative treatment is referred to as either amputation or radical surgical excision while palliative treatment involves simple debridement, drainage and antibiotics. The terminology used is unfortunately confusing and the term radical resection is inconsistent with musculoskeletal oncology principles, where it generally refers to resection of an entire compartment. The authors' description of the surgical procedure involved in a reconstructive/non-ablative curative treatment option could more accurately be described as wide or marginal resection. The authors correctly state that there are no objective criteria for defining resection margins and that it remains the decision of the treating surgeon. Previous studies have, however, shown increased treatment failure rates with marginal resections in compromised hosts. The problem we face is the fact that host stratification remains a subjective exercise as a result of the absence of incumbent objective criteria.
Curative surgical procedures are described as having four crucial steps, namely bone resection, dead space management, soft tissue reconstruction and restoration of skeletal stability.
In terms of dead space management PMMA beads and spacers are mentioned. The omission of absorbable implants may not be unintentional as there has been a movement towards induced membrane techniques. Newer techniques, including the use of bio-active glass, unfortunately did not receive attention. Notably Walter et al recommend a two-stage procedure with definitive soft tissue reconstruction being performed approximately one week following the index procedure, whereas in certain other protocols single-stage procedures are implemented.
The statement that surgery is the most important element of a curative approach remains accurate. Additional measures, including systemic antibiotics, are however also recommended. The authors prefer oral antibiotics, which is in accordance with other review articles on the topic. Combination therapy is discussed as a debatable subject. In contrast to their summation, some evidence does exist for the use of a combination of antibiotics. As stated in the article, the optimal duration of antibiotic therapy remains unknown.
This excellent review article will serve the surgeon faced with the intimidating problem of chronic osteomyelitis well, and introduces a novel concept in its treatment. In my opinion the approach suggested in this article may prove very useful and further development of the concept is required. A crucial step in the decision-making process has, however, been omitted. The authors fail to provide guidelines as to how the appropriate treatment strategy, albeit curative or palliative, should be selected. In other words, how should patient classification be integrated with the treatment protocols suggested and which patients would optimally be managed with a palliative treatment strategy? Extrapolation of these ideas and further research into integration of host classification and selection of the appropriate treatment strategy is therefore imperative.
The prevention of orthopaedic implant infection in patients undergoing dental procedures
Reviewer: Prof EEG Lautenbach
Milpark Hospital PO Box 5921 Cresta 2118
Evidenced-based guideline and evidence report J Bone Joint Surg Am. 2013;95:745-7
This article, as published in the J Bone Joint Surg Am 2013;95:745-17, consists of only a summary of the findings. The full report on the material and methods is published on a website http://www.aaos.org/research/guide-lines/PUDP/PUDP._guideline.pdf. The web page has over 320 pages of tables and figures illustrating the material studied, the results of analysis and evaluation.
This is a monumental work conducted with the collaboration mainly of the AAOS (American Academy of Orthopaedic Surgeons) and ADA (American Dental Association). The working group consisted of 13 members of these two organisations and another ten professionals engaged in research and statistics. The process was peer reviewed by representatives of 20 associations with an interest in this field. A literature search of three electronic data bases harvested 3 702 abstracts. Of them, 2 475 were excluded on the basis of their relevance or quality. The full texts of 1 227 articles were then reviewed. Only 213 of these articles had indirect evidence on orthopaedic implant infection and were considered for background microbiology.
Then 188 articles were selected because they had indirect evidence of post-dental procedure bacteraemia and prophylaxis. On closer scrutiny and elimination 31 articles were adjudged to be relevant for orthopaedic implant infection. A further 61 articles on post-dental bacteraemia were considered for background microbiology. There was only one article of high quality in this very large group with direct evidence considered for recommendation. The power of articles was based on stringent criteria. They were assessed for flaws based on whether the study was prospective, numerically significant, blinded with unbiased assignment and with a comparable control group and other essential characteristics. The quality of a paper was classified high if there was 0-1 flaw, moderate 2-3 flaws, low 4-5 flaws and very low for more than 5 flaws. Analysis proceeded for a year and then carefully worded recommendations were made.
We are designed to cope in an environment swamped by micro-organisms except to a degree, the immune-compromised.
Unjustified prophylactic antibiotic therapy contributes to our serious and growing problem with multi-resistant nosocomial infections
In summary the recommendations were:
1. The practitioner might consider discontinuing the practice of routinely prescribing prophylactic antibiotics for patients with hip and knee prosthetic joint implants undergoing dental procedures. Grade of recommendation: Limited - A limited recommendation means the quality of the supporting evidence that exists is unconvincing or that well-conducted studies show little clear advantage to one approach versus another.
2. We are unable to recommend for or against the use of topical oral antimicrobials in patients with prosthetic joint implants or other orthopaedic implants undergoing dental procedures. Grade of recommendation: Inconclusive. An inconclusive recommendation means that there is a lack of compelling evidence resulting in an unclear balance between benefits and potential harm.
3. In the absence of reliable evidence linking poor oral health to prosthetic joint infection, it is the opinion of the work group that patients with prosthetic joint implants, or other orthopaedic implants, maintain appropriate oral hygiene. Grade of recommendation: Consensus. A consensus recommendation means that expert opinion supports the guideline recommendation even though there is no available empirical evidence that meets the inclusion criteria.
I am delighted with this paper. It vindicates my long-held belief that we are designed to cope in an environment swamped by micro-organisms except to a degree, the immune-compromised. Bacteraemia occurs regularly in response to a host of daily natural activities without consequences. It has long been known that one can inoculate animal tissue with bacteria without infection resulting unless one exceeds a minimum critical number of organisms, or a quorum, or one interferes with the local or systemic conditions of the host.
Many of these bacteraemias result from activities related to dental care but the fact is that the bacterial flora found in the mouth and teeth differs from the flora causing infection around arthroplasties.
As one concerned with infection control in hospitals, unjustified prophylactic antibiotic therapy contributes to our serious and growing problem with multi-resistant nosocomial infections.
Conversion of open tibia Illb to Ilia fractures using intentional temporary deformation and the Taylor Spatial Frame
Reviewer: Dr N Ferreira
Tumour, Sepsis and Reconstruction Unit Department of Orthopaedic Surgery University of KwaZulu-Natal Greys Hospital Pietermaritzburg Tel: +27 033 897 3299 Nando.Ferreira@kznhealth.gov.za
Sharma H, Nunn T Strat Traum Limb Recon (2013), DOI 10.1007/s11751-013-0160-0
South African roads are some of the most dangerous in the world. According to a World Health Organization (WHO) report, South Africa has the second highest road traffic death rate in Africa (31.9/100 000) with pedestrians accounting for 37% of those deaths. The high incidence of road traffic accidents also contributes to the tremendous burden of open fractures currently overwhelming the South African health system.
Gustilo and Anderson type IIIb open tibial injuries are especially demanding to manage, as these patients require soft tissue reconstructive procedures in addition to bony procedures. Unfortunately, due to the high-energy nature of South African trauma a large percentage of open tibial fractures fall into this category. Data from Greys Hospital confirm this with 48% of open tibia fractures being Gustilo and Anderson type IIIb injuries.
The article by Sharma et al refers to the British Orthopaedic Association Standards for Trauma (BOAST) guidelines that emphasise the need for a multidisciplinary team, including orthopaedic and plastic surgeons in the treatment of these injuries. This may not always be possible in the South African setting where a relative shortage of plastic surgeons can cause delays in soft tissue cover. For this reason, innovative ways of dealing with soft tissue defects must be explored. In certain instances where IIIb open fractures are associated with segmen-tal fracture comminution or bone loss, soft tissue defects can potentially be closed with acute shortening of the limb. This should however be done with caution, as excessive acute shortening can potentially lead to limb-threatening vascular complications.
The technique of deformity-assisted wound closure is discussed in the article and illustrates its potential to obviate the need for soft tissue reconstructive procedures. It relies on distraction histogenesis for soft tissue reconstruction. This is achieved by intentional limb deformation to allow tension-free soft tissue closure followed by gradual deformity correction once the soft tissue envelope has healed. The authors utilised the Taylor Spatial Frame (Smith & Nephew, Memphis, TN) for gradual reduction as it 'simplifies deformity correction and easily allows further corrections if the position is suboptimal'.
The authors outline the ideal cases that can benefit from this approach and the factors that should be borne in mind when selecting an appropriate patient. These include:
• Soft tissues - Antero-medial wounds are ideally suitable. Closure must be possible without compromising vascularity and adequate subcutaneous tissue must be present to support the skin and prevent wound breakdown.
• Fracture pattern - The fracture must allow deformation. Comminuted fractures with same level fibula fractures are ideal. Comminution also allows shared strain during the correction process.
• Patient factors - Patients must be willing to tolerate temporary limb deformation and prolonged external fixation. The possibility of failure and limb ablation should also be raised and discussed initially.
This article reports two cases where temporary intentional deformation was successfully employed for soft tissue reconstruction. It identifies the subgroup of Gustilo-Anderson IIIb injuries where this technique could be useful and alerts the reader to potential pitfalls and complications. As the use of hexapod external fixators becomes more widespread and surgeons become more proficient with their application and programming, this innovative strategy for dealing with soft tissue loss could prove beneficial for many patients.
Management of Legg-Calvé-Perthes disease using an A-frame orthosis and hip range of motion. A 25-year experience
Reviewer: EB Hoffman
Emeritus Associate Professor Division of Orthopaedic Surgery University of Cape Town Tel: 021 404-5108
MM Rich, PL Schoenecker J Pediatr Orthop 2013;33:112-19
Containment treatment for Perthes' disease is widely accepted, but whether this should be done conservatively or by surgical means (pelvic or femoral osteotomy) remains controversial. The authors retrospectively reviewed 240 hips (213 patients) in the necrotic or fragmentation stage treated with a weight-bearing A-frame orthosis and multiplanar twice-daily exercises (AF-ROM).
On presentation the hips were examined under general anaesthesia and if hip abduction was <25°, an adductor tenotomy was done to achieve 35°of abduction. An abduction cast was applied for 6 weeks after which a custom-made A-frame orthosis was fitted with the hips abducted 35° and in slight internal rotation, therefore limiting external rotation. Multiplanar hip exercises were done twice daily. The patient was weaned from the ortho-sis when there was reconstitution of the lateral column (average 13 months).
Of the 240 hips, 113 were Herring group B (up to 50% loss of lateral pillar), and 115 Herring group C (>50% loss of lateral pillar). All results were assessed at maturity by a modified Stulberg classification. Stulberg I and II were spherically congruent and were considered good. Stulberg III hips were ovoid and congruent and considered fair. Stulberg IV (flat >1 cm, congruous) and Stulberg V hips (flat and incongruous) were considered poor. Group B hips had 89% good, 7% fair and 4% poor results. Group C had 67% good, 23% fair and 10% poor results.
These results differ from the often quoted multicentre study of Herring et al1 which suggested that surgical treatment only benefited group B hips >8 years, and that treatment for group C offered no benefit. Studies of treatment with the Scottish Rite orthosis reported only 40% good results2 because it did not restrict external rotation as is done in the AF-ROM. The authors feel that their results are superior to surgical containment and argue that a femoral or pelvic osteotomy may not permit accommodation of the enlarging head and thereby limit dynamic con-tainment.3
An abduction cast was applied for 6 weeks after which a custom-made A-frame orthosis was fitted with the hips abducted 35° and in slight internal rotation
The average age of the patients was 6.4 years (range 2.6 to 11.3 years). Although the patients with group C hips were significantly younger than those in group B, the age within each pillar group had no influence on outcome. This is contrary to current belief. They treat all patients. This vindicates the authors who advocate that Perthes' does not necessarily have a good outcome <5 years of age,4 and it refutes the pessimistic outlook for the older patients.
I have two questions regarding the study. They do not use pre-op traction. In our unit we find it beneficial especially in the late presenter with a stiff hip. They also do not discuss the role of non-weight bearing. They do however advise the use of crutches in the periods that the patient is out of the orthosis. The best results ever published5 used long-term bed rest and containment. Our unit uses containment and a wheelchair, but this is not always practical in the older and bigger child. MRI studies6 suggest that non-weight bearing may be beneficial but the excellent results of this study, emphasising containment by means of adequate abduction plus multiplanar movement, makes one wonder if the extra effort to obtain compliant non-weight bearing is worth it.
References
1. Herring et al. J Bone Joint Surg 2004;86-A:2121-34.
2. Weinstein et al. J Bone Joint Surg 1992;74-A:12-21.
3. Rab et al. J Pediatr Orthop 1985;5:8-12.
4. Schepers and Robertson. SA Orthop J 2011;10:67-73.
5. Brotherton and McKibbin. J Bone Joint Surg 1977;58-B:8-14.
6. De Sanctis et al. J Pediatr Orthop 2000;20:455-70.
Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review
Reviewer: Prof JG Myburgh
Department of Orthopaedic Surgery Steve Biko Academic Hospital Tel: (012) 354-2851
Michael J Griessser, Joshua D Harris, Brett W McCoy, et al Journal of Shoulder and Elbow Surgery, February 2013, vol 22, no. 2
This article is interesting because it highlights all the complications reported in the literature following the Latarjet or Bristow shoulder stabilisation procedure that surgeons should discuss with their patients before and after the operation. The one complication that is not specifically mentioned is failure of hardware, but it may fall under removal of hardware and nonunion.
The authors analysed 45 studies (1 904 shoulders) in this review article. The studies were all level IV evidence and confined to the English literature. All the studies dealt with complications after Bristow or Latarjet procedures. Ninety per cent of the surgeries were performed open while 9.3% were all arthro-scopic procedures.
The reported complication rate was high (30%). The redisloca-tion rate was 2.9% and the recurrent subluxation rate was 5.8%. Forty-eight patients (2.5%) required revision stabilisation surgery, while 46 needed removal of hardware. Five patients needed total shoulder arthroplasty. Neurovascular injuries comprised six axillary artery injuries (one intra-operative and five pseudo aneurysms), 11 musculocutaneous nerve, six axillary nerve, four ulnar nerve, three radial nerve, two median nerve, one suprascapular nerve and two trunk level brachial plexus injuries.
It highlights all the complications reported in the literature following the Latarjet or Bristow shoulder stabilisation procedure that surgeons should discuss with their patients
The arthroscopic procedures had a lower re-operation rate but most of the procedures were performed by experienced shoulder surgeons. There was a greater loss of external rotation following the arthroscopic procedures (16° vs 12° for the open surgery.) The length of follow-up was 22.1 months post-arthro-scopic vs 88.0 months for the open techniques. Most of the redis-locations and re-operations occurred within the first year following surgery. There was no significant difference in the nonunion rate or neurovascular injuries between the open and arthroscopic procedures.
The non-union or fibrous union rate was 9.4%.
In conclusion, the Bristow-Latarjet procedures are very effective stabilisation procedures for recurrent shoulder instability associated with a substantial risk of complications.
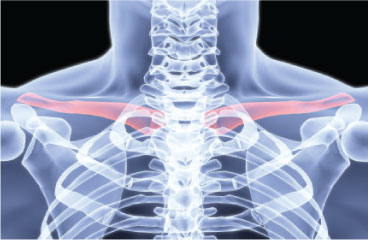
Early failures with single clavicular transosseous coracoclavicular ligament reconstruction
Jay B Cook, James S Shaha, Douglas J Rowles et al Journal of Shoulder and Elbow Surgery, December 2012, vol 21, no. 12
This is an honest retrospective review of all the coracoclavic-ular (CC) reconstructions performed at the author's institution from January 2009 until 2011. They performed ten CC ligament reconstructions in nine active duty male soldiers with an average age of 25.9 years using the GraftRope® which provides temporary fixation with a high strength suture combined with a biologic graft. All procedures were performed by a single surgeon. There were seven Rockwood grade V and two grade III acromioclavicular joint separations.
Eighty per cent revealed a significant loss of reduction at an average follow-up of 9.7 months. Seven of the patients were compliant and did not sustain any trauma. The non-compliant patient was considered a traumatic failure and revised. One patient had subsidence of the button through the medial cortex of the coracoid and the other seven had intact hardware. Complete recurrence of the deformity occurred in 40% of patients. Revision surgery was performed in 40% of patients for continued pain, deformity and dysfunction. No patients had fractures of the coracoid or clavicle. Clavicular tunnel widening was noted in all follow-up X-rays.
There were five good / excellent results, one fair result and four poor results. The authors conclude that, based on their results, they cannot recommend the use of this device in CC ligament reconstruction. Their patients were young male soldiers and high demand patients and the technique might have been more successful in low demand patients. A weakness of the study is their small numbers, but they had to change their approach due to the early high failure rate.
In conclusion, acromioclavicular dislocations remain a very challenging condition to treat and there is no fail-safe technique for treatment.
Venous thromboembolism: Prophylactic and therapeutic practice guideline 2013
Reviewer: A Visser
Clinical Pathologist Vermaak and Partners Eugene Marais Hospital Pretoria
S Afr J Med April 2013, Vol 103, No 4
The previous South African guideline for prophylactic and therapeutic use of anticoagulants was published in June 2009 and is now revised in the April 2013 edition of the South African Medical Journal. The guideline was compiled by the Southern African Society of Thrombosis and Haemostasis (SASTH), which consists of a range of specialists from both laboratory medicine (Haematology) and clinical disciplines (Surgery, Vascular Surgery, Critical Care, Internal Medicine, Paediatrics, Neurology, Obstetrics and Gynaecology as well as Anaesthesia). Although the previous guideline was co-authored by an orthopaedic surgeon, and the current guideline states inclusion of orthopaedics, none of the current authors are orthopaedic surgeons. In addition, the current SASTH website does not mention any orthopaedic surgeons as members.
However, it should be considered that all recommendations are based on evidence-based research, and the role of expert opinion is by and large omitted. The question aimed to be answered here is, how exactly does the 2013 guideline differ from the 2009 guideline, and what is the implication in orthopaedic practice?
Prophylactic use of anticoagulants within the surgical population still requires classification of a patient based on certain patient- and procedure-based risk factors. This has largely remained the same, except for the inclusion of HIV/AIDS, autoimmune disease and antiphospholipid syndrome as patient-associated risk factors. Once the patients are classified, the use of various prophylactic anticoagulants is suggested, and is the same as for the 2009 guideline but for two issues.
First, the use of aspirin in low-risk patients is specified to have a weak preventative effect for venous thromboembolism (VTE). Secondly, the medium risk group (high risk procedure with no patient risk factors or low risk procedure with patient risk factors) specifies the acceptability of post-operative initiation of thromboprophylaxis and stipulates the modest preventative effect of intermittent pneumatic compression.
The major addition to this guideline is information on the new oral anticoagulants (NOACs). Use of these drugs in prophylaxis should always be initiated post-operatively - for dabigatran 4 hours and rivaroxaban 6 hours after surgery. Epidural catheter removal should be performed after 22-26 hours of NOAC cessation. Following removal of the epidural catheter, rivaroxaban should only be administered after 6 hours and dabigatran after 1 hour. Although routine monitoring is not advocated in patients using the NOACs, certain clinical conditions may necessitate this, which is clearly outlined in this manuscript.
Recommendations regarding thromboprophylaxis in gynaecological surgery and treatment of acute cerebral venous thrombosis have been expanded significantly (not for the purpose of this article).
Treatment of VTE remains by and large the same, as NOACs have not been registered for use in this setting. Of note, the duration of initial therapy using low molecular weight heparin, nadroparin or dalteparin has been reduced to five days, from the previously advocated seven days. Subsequent anticoagula-tion therapy however has been increased for idiopathic DVT and pulmonary embolism patients to nine months from the previous six months.
A welcome addition to the article is a very simple definition of a mobile patient, albeit in the section dealing with medical patients. Here, a patient is considered as mobile if he/she participates in any more physical activity than sitting in a chair and mobilising to the bathroom.
On the whole, the guidelines are largely similar to the previous edition, with the inclusion of recommendations regarding novel drugs. As orthopaedic surgery is considered a major risk factor for thromboembolic phenomena, it may be prudent for experts in the field to become more involved and so let the voice of the major prescribing clinicians be heard.














