Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.12 no.2 Centurion ene. 2013
SPINE
Upper cervical deformities secondary to hydrocephalus - a case report
Dr Paul Ryan
MBChB FCOrtho Consultant Orthopaedic Surgeon Inkosi Albert Luthuli Hospital, Belair Road, Durban
ABSTRACT
BACKGROUND: Hydrocephalus may complicate upper cervical pathology but is seldom the cause of cervical spine pathology.
METHODS: This case report describes a child with hydrocephalus secondary to an intraventricular haemorrhage, who required atlantoaxial fusion for recurrent C1/C2 rotatory subluxation, and who has subsequently developed progressive subaxial deformity.
CONCLUSION: This case highlights some of the important fundamentals of the paediatric cervical spine, its biomechanics, susceptibility to injury, and the progressive nature of deformities where the inciting aetiology cannot be addressed.
Key words: subaxial subluxation, atlantoaxial, hydrocephalus, cervical
Introduction
Atlantoaxial subluxation has a number of causes or associations including congenital abnormalities of the atlantoax-ial complex and its ligaments, inflammatory arthritides, inflammatory processes in the upper respiratory area, trauma, bony dysplasia, and certain syndromes. Subaxial subluxation is seen in a number of conditions including rheumatoid arthritis, trauma, Down syndrome, rarely Marfan syndrome, and as a side effect of corticosteroid use. It must be distinguished from physiological subluxation which is seen in younger children especially at C2/3 level.1
Hydrocephalus may complicate upper cervical pathology but is seldom the cause of cervical spine pathology.2 We present a case of a child with hydrocephalus who required atlantoaxial fusion for recurrent C1/C2 rotatory subluxation, and has subsequently developed progressive subaxial deformity.
Case report
A 13-year-old patient is being followed up in the King George V spinal clinic for a problem of progressive subaxial subluxation, following C1/C2 fusion in March of 2007. The salient background history is as follows. She was born in 1996 - premature at 36 weeks gestation, was ventilated- for a short period in the neonatal ICU, and was discharged 2 months post-delivery in a satisfactory condition. At 5 months of age, it was noted that her head circumference had increased significantly to 44 cm (on the 97th centile), and she was referred to the neurosurgical unit where she was diagnosed with communicating hydrocephalus due to a previous intraventricular haemorrhage. At that time, she had no neurological sequelae. She underwent uncomplicated ventriculo-peritoneal (VP) shunting, and was routinely followed up for a further seven years, when in 2004 she was discharged with a diagnosis of arrested asymptomatic hydrocephalus.
She underwent right inferior rectus recession in 2001 (at age 4 years) for congenital squint. There was no delay in her developmental milestones and she began attending mainstream schooling at age 6.
She presented to the orthopaedic department of a local hospital in 2005 at age 9 with torticollis and C1-2 rotatory subluxation, neurologically intact. There was no evidence to suggest inflammatory arthropathy, any inflammatory process in the upper respiratory system, or any history of trauma. She responded to traction and conservative management. MR of the cervical spine demonstrated early syrinx formation from C2 to C4, and associated significant hydrocephalus. She was reviewed and discharged from the neurosurgical unit with the diagnosis of arrested asymptomatic hydrocephalus.
In March of 2007 she was re-admitted with a second episode of torticollis and atlantoaxial rotatory subluxation (Figure 1), which did not reduce on traction. She was myelopathic - Frankel grade D neurology.

She was noted to have decreased visual acuity and was referred to the ophthalmology clinic, where she was diagnosed with advanced irreversible optic atrophy.
She was referred to the spine surgery unit, and on 9 March 2007 she underwent posterior atlantoaxial fusion with Brooke's technique of sublaminar wiring and autolo-gous bone grafting.
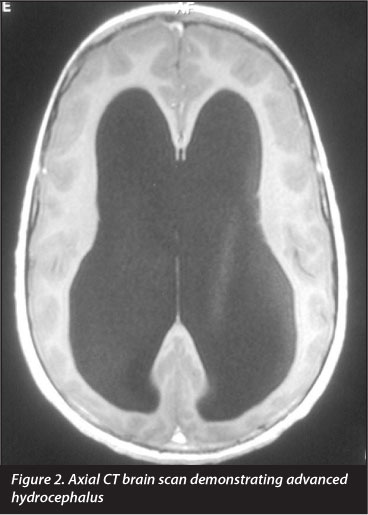
She was referred back in to the neurosurgical unit for review, where on CT (Figure 2) active hydrocephalus was diagnosed and she underwent reinsertion of VP shunt. She was rehabilitated at the spine care rehab centre and was discharged after 3 months - ambulant with the aid of a single walking stick.
She was followed up regularly by the unit on an outpatient basis, and was then noted in May of 2008 (one year post fusion) to have progressive subluxation of C3 on C4. Since then, the subluxation has been progressive in nature (Figures 3-6), but against advice and despite counselling, her parents have refused further surgical intervention.
On most recent clinical evaluation, she was found to be in good general health.
There was gross sagittal malalignment of the cervico-dorsal area with a kyphosis extending from C2 to C5, and compensatory lower cervical and upper dorsal lordosis (Figure 7). There was marked wasting of the sternocleido-mastoid, periscapular and upper paraspinal muscles. Movements of the cervical spine were grossly reduced: flexion to chin on chest, extension resulting in a neutral head position, only minimal rotational movement, and 10° of lateral flexion.

She had flexible planovalgus feet and bilateral hip flexion contractures of 10°. Neurological testing revealed evidence of myelopathy predominantly in the lower limbs, with increased tone (Ashworth 2), hyperreflexia (including abdominal reflexes) and bilateral unsustained ankle clonus.
Radiographs taken at her last visit in 2011 (Figure 6) demonstrate fusion of the atlantoaxial complex, segmental kyphosis from C2 to C5 with a Cobb angle of 90°, and compensatory hyperlordosis at the occipito-cervical junction and lower cervical levels.
Discussion
Atlantoaxial subluxation has a number of causes or associations including congenital abnormalities of the atlantoax-ial complex and its ligaments, inflammatory arthritides, inflammatory processes in the upper respiratory area, trauma, bony dysplasia, and syndromes such as Down, Morquio and more rarely Marfan. The upper cervical deformities may lead to secondary hydrocephalus. To the best of the author's knowledge, hydrocephalus alone has not been cited as a cause of atlantoaxial subluxation.
The fulcrum of motion in the cervical spine lies in the region of C1 to C3 under the age of 8 years. This progresses caudally till age 12 when it approximates that of adults - in the region of C5-6.3 Ligamentous laxity, shallow articular facets, undeveloped spinous processes and physiological wedging of the vertebral bodies result in increased mobility of the cervical spine in children. Coupled with a relatively large head, and muscle weakness, this predisposes the spine to instability and kyphosis deformity.
The aetiology proposed is an imbalance of the size and weight of the head, and the stabilising capability of the cervical paraspinal musculature
In this case, there was no history of trauma or evidence of inflammatory processes on initial presentation with torticollis. The aetiology proposed is an imbalance of the size and weight of the head, and the stabilising capability of the cervical paraspinal musculature. CNS lesions are also postulated to cause cervical deformities by disrupting the normal postural reflex mechanisms and coordinated spinal muscle control.2
Posterior upper cervical fusion in the paediatric population has been shown to be a successful procedure.4 Indeed, long-term maintenance of sagittal cervical alignment has been shown to improve in the post-operative period due to remodelling.5 Growth continues anteriorly in the fused segment and is maintained at a rate of 34% of normal.6 Even in cases of post-operative subaxial kyphosis, spontaneous sagittal realignment can be expected.7
Care should be taken, however, to ensure anatomical relationship during fusion, as there is a linear correlation between the atlantoaxial fixation angle and the degree of subsequent subaxial deformity.8 This is noted to be of particular importance in the setting of rheumatoid arthritis, where subaxial subluxation complicates up to 86% of cases fixed in excessive extension.9 Posterior wiring techniques rely on compressive forces for stability and tend to fix segments in a hyperlordotic position.
Subaxial subluxation is more commonly seen in cases of inflammatory arthropathies, Down's syndrome, and trauma, more rarely in Marfan syndrome, and in case reports as a side effect of systemic corticosteroid use.10,11 It may also be seen in otherwise normal children as physiological subluxation - especially in the younger child with a long neck and greater cervical mobility.12 Indeed, slight forward displacement of vertebra seen on lateral radiographs taken with a flexed neck is common in children, especially at C2-3 level.1
The fulcrum of cervical mobility is at this level, and similar to the C1-2 facets, the C2-3 facets are relatively horizontal in orientation when compared to the more caudal levels.
In this case, although the atlantoaxial complex was fixed in a relatively neutral position, the imbalance between the cervical stabilisers and the resultant force from the weight of the head has led to progressive sub-axial kyphosis and sagittal plane deformity, as demonstrated by the follow-up radiographs. This in turn has led to extrinsic cord compression, intrinsic cord damage, and myelopathy.
This case highlights some of the important fundamentals of the paediatric cervical spine, its biomechanics, susceptibility to injury, and the progressive nature of deformities where the inciting factor cannot be addressed.
The patient's primary care giver gave informed consent for the use of clinical details and photographic materials.
No benefits in any form have been or are to be received from a commercial party related directly or indirectly to the subject of the article. The content of this article is the sole work of the authors.
References
1. Bailey DK. The normal cervical spine in infants and children. Radiology, 1952;59(5):712-19. [ Links ]
2. Sherk HH, et al. Hydrocephalus, cervical cord lesions, and spinal deformity. Spine (Phila Pa 1976), 1986;11(4):340-42. [ Links ]
3. Jagannathan J, et al. Cervical spine injuries in pediatric athletes: mechanisms and management. Neurosurg Focus, 2006;21(4):E6. [ Links ]
4. Lowry DW, et al. Upper cervical spine fusion in the pediatric population. J Neurosurg, 1997;87(5):671-76. [ Links ]
5. Ishikawa M, et al. Long-term impact of atlantoaxial arthrodesis on the pediatric cervical spine. J Orthop Sci, 2009;14(3):274-78. [ Links ]
6. Anderson RC, et al. Long-term maintenance of cervical alignment after occipi-tocervical and atlantoaxial screw fixation in young children. J Neurosurg, 2006;105(1 Suppl):55-61. [ Links ]
7. Parisini P, et al. C1-C2 posterior fusion in growing patients: long-term follow-up. Spine (Phila Pa 1976), 2003;28(6):566-72; discussion 572. [ Links ]
8. Yoshimoto H, et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976), 2004;29(2):175-81. [ Links ]
9. Matsunaga S, Onishi T, Sakou T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976), 2001;26(2):161-65. [ Links ]
10. Dunn NA, Lewis-Barned NJ, Jones JK. Multiple subaxial subluxation of cervical spine: a side effect of corticosteroids? Br Med J (Clin Res Ed), 1985;290(6464):299-300. [ Links ]
11. Place HM, Enzenauer RJ. Cervical spine subluxation in Marfan syndrome. A case report. J Bone Joint Surg Am, 2006;88(11):2479-82. [ Links ]
12. Townsend EH Jr, Rowe ML. Mobility of the upper cervical spine in health and disease. Pediatrics, 1952;10(5):567-74. [ Links ]
 Reprint requests:
Reprint requests:
Reprint requests:
Dr P Ryan paulrya@ialch.co.za














