Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.12 no.2 Centurion Jan. 2013
HIP
Relationship of radiographic criteria to clinical findings in patients with femoroacetabular impingement
S SolookiI; M SamanianII; MJ EmamiIII; VosoughiIV
IMD Assistant Professor of Orthopaedic Surgery, University of Medical Sciences, Shiraz, Iran
IIMD Orthopaedic Surgeon, University of Medical Sciences, Shiraz, Iran
IIIMD Professor of Orthopaedic Surgery AR, University of Medical Sciences, Shiraz, Iran
IVMD Chief Resident of Orthopaedic Surgery Bone and Joint Disease Research Centre, Department of Orthopaedic Surgery, Chamran Hospital, Shiraz, University of Medical Sciences, Shiraz, Iran
ABSTRACT
BACKGROUND: Femoroacetabular impingement (FAI) leads to pain, limited joint motion and eventually osteoarthritis. The aim was to determine the usefulness of different radiographic criteria to diagnose FAI.
METHODS: A total of 250 healthy-appearing participants were selected randomly for screening of hip pain and specific impingement tests. They were categorised in three groups: Group 0 included asymptomatic participants without positive impingement tests; Group 1 participants were either asymptomatic with positive impingement tests or symptomatic with negative tests; participants with painful hip and positive impingement tests formed Group 2. Radiographic criteria including cross-over sign, posterior wall sign, coxa profunda, acetabular protrusion, pistol grip deformity, centre-edge angle, extrusion index, offset ratio, alpha angle, herniation pits and osteoarthritic changes were utilised in anteroposterior and cross-table lateral radiograph assessment of all cases. Radiographic criteria were compared in different groups.
RESULTS: Only centre-edge angle (mean 35.3 ± 5.9, p=0.05), herniation pits (p=0.04) and osteoarthritic changes (p=0.05) showed a statistically significant difference in patients with FAI in comparison to other groups.
CONCLUSION: As herniation pits and osteoarthritis signs are secondary findings of femoroacetabular impingement and the centre-edge angle value is not very sensitive, radiographic criteria are not diagnostic of FAI.
Key words: femoroacetabular impingement, hip, acetabulum
Introduction
Femoroacetabular impingement (FAI) is defined as the abutment between the femoral neck and the acetabulum rim,1 and is an anatomical deformation of the femoral head or the acetabular rim or both. Although it can be seen in patients with normal hip morphology in extreme range of motion,2 less motion is required to result in abutment in patients with FAI. Two distinct types have been recognised.3,9 The cam type refers to deformed femoral head abutting against the acetabular rim during flexion and internal rotation. It is more common in young active male patients. This lesion can lead to tearing of the labrum notably in the anterosuperior part and eventually results in osteoarthritis.1,4 The other type, pincer lesion, presents more commonly in middle-aged active women. This type occurs with acetabular over-coverage due to repeated contact between the normal femoral head and the acetabular rim.7-8
FAI patients usually suffer from intermittent groin pain worsening with activity.10 Sometimes painful locks and instabilities from the occult labral tear are seen.7 Although several tests such as the posterior inferior impingement test2 and the flexion abduction external rotation (FABER) provocation test7,11 can be performed to identify FAI, the flexion adduction internal rotation (FADIR) test is the most sensitive physical examination test for FAI.12
Several radiographs should be taken in patients with FAI signs and symptoms, including a true anteroposterior (AP) view,13,14 anteroposterior view in 10 to 15 degrees of internal rotation, the Dunn view (AP of the hip in neutral rotation, 45 degrees of flexion and 20 degrees of abduction),15 and a cross-table lateral view of the affected hip.16 Several hip radiographic findings have been considered as clues to diagnose FAI.16-22 The aim of this study is to determine the relationship between different radiographic measurements and patients' signs and symptoms.
Methods
The study was carried out in the Bone and Joint Disease Research Centre, Department of Orthopaedic Surgery, Chamran Hospital, Shiraz University of Medical Sciences, Shiraz, Iran. The study was approved by the ethical committee of the University in accordance with the Ethical Standards of the 1964 Declaration of Helsinki as revised in 2000. A total of 250 young people (all the participants submitted the informed written consent prior to being included in the study) were evaluated from August 2009 to March 2010. These participants were healthy visitors of admitted patients in the hospital of orthopaedic trauma. No-one had a definite history of recent or old hip pathology such as osteonecrosis, Legg-Calvé-Perthes disease, developmental dysplasia of the hip or previous hip surgery. History of any hip pain and related decreased daily activity was taken from each participant. In addition impingement tests2,7,11,12 were carried out by a single orthopaedic surgeon (the second author). Then a true AP and a cross-table lateral view were taken. Eleven radi-ographic measurements were determined for each participant.
Radiographic criteria
1. Cross-over sign
Acetabular retroversion is visualised on an AP pelvic radiograph by projecting the anterior wall lateral to the posterior wall proximally and crossing posterior wall in a medical direction distally.14,16
2. Posterior wall sign
If the posterior wall lies medial to the femoral head centre, it shows a retroverted acetabulum.8,14,16
3. Coxa profunda
Deepened acetabular fossa is determined by overlapping of the medial floor of the acetabulum by the ilioischial line.17
4. Acetabular protrusion
Protrusio acetabuli is defined if the medical line of the femoral head crosses the ilioischial line.17
5. Pistol grip deformity
This sign is positive when femoral head shape is non-spher-ical.18
6. Centre-edge angle
Centre-edge angle is formed by a vertical line and a line connecting the femoral head centre to the lateral edge of the acetabulum. Values of more than 40 degrees are considered positive.16
7. Extrusion index
Extrusion index is the percentage of the femoral head uncovered by the acetabulum. It is positive for values below 10%.16
8. Offset ratio
Head-neck offset is defined as the difference between the anterior radius of the femoral head and the anterior radius of the femoral neck in cross-table lateral view. An abnormal distance is less than 9 mm.19 Offset ratio is determined as the ratio of the head-neck offset distance relative to the femoral head diameter. Values of less than 0.15 are considered abnormal.16
9. Alpha angle
Alpha angle is the angle between the femoral neck axis and a line connecting the head centre to the femoral head-neck junction. A normal alpha angle is typically 45 degrees. Patients with FAI usually have angles of more than 50 degrees.20-21
10. Herniation pits
Femoral herniation pits or Pitt's pits are intraosseous fibro-cystic lesions in the femoral neck as a result of recurrent FAI.22
11. Osteoarthritic changes
These include the presence of any significant ossicle (calcification of the detached labrum) on acetabular rim, joint space narrowing, osteophyte and subchondral cyst formation.16,17
All persons were categorised in three groups according to their history of pain and positivity of impingement tests: Group 0 included participants without any positive history or impingement tests. Participants in Group 1 (low suspicious group) had either positive pain history or positive impingement tests. Group 2 persons had a positive pain history and positive impingement tests. They were regarded as the highly suspicious group. Radiographic criteria were compared in different groups.
Statistical analysis
Analysis was done using the statistical package for the social sciences version 18.0 for Windows (SPSS Inc. Chicago, IL, USA). The prevalence of each radiographic finding was calculated in the different groups. By using the Chi-square test or Fisher's exact test, radiographic criteria were analysed. A p-value equal to and less than 0.05 is considered a statistically significant difference.
FAI patients usually suffer from intermittent groin pain worsening with activity. Sometimes painful locks and instabilities from the occult labral tear are seen
Results
The sample of 250 participants included 208 men and 42 women, aged under 40 years (range: 20-55 years with a mean age of 30). Demographic features of the different groups are described in Table I.
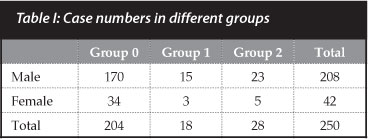
The prevalence of FAI in this study is 11.2%. All participants in Group 2 had unilateral signs and symptoms (right side: 16; left side: 12) although bilateral hip deformities were seen in all cases of this group. Ten participants in Group 1 suffered from hip pain without positive testing and eight cases with positive impingement tests had no history of pain.
Results of various radiographic parameters (Table II)
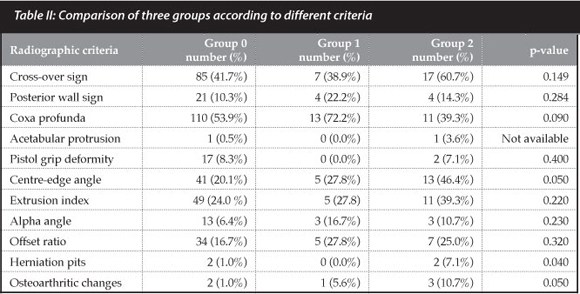
Cross-over sign and positive wall sign
These two radiographic findings of acetabular retroversion are not diagnostic of FAI. Although the cross-over sign was more prevalent in Group 2 cases, a p-value of 0.144 did not show any statistically significant difference.
Coxa profunda and acetabular protrusion
Positive values of coxa profunda in different groups were 53.9% in Group 0, 72.2% in Group 1 and 39.3% in Group 2. There is no statistically significant correlation between symptomatic patients with positive impingement tests and asymptomatic patients according to coxa profunda (p=0.09). There were only two cases with acetabular protrusion in the participants (one in Group 0 and the other in Group 2).
The aim of this study is to determine the relationship between different radiographic measurements and patients' signs and symptoms
Pistol grip deformity
This sign was seen in 8.3% of cases in Group 0 and 7.1% of participants in Group 2. No-one in Group 1 had this sign. A p-value of 0.4 showed no statistical relationship.
Centre-edge angle
A p-value of 0.05 describes a statistically significant relationship between centre-edge angle (mean ± standard deviation: 35.3 ± 5.9) and clinical findings.
Extrusion index
No significant difference was seen in the analysis of this finding with a mean of 11.6% in participants with FAI (p=0.22).
Offset ratio
Analytical tests could not prove any significant relationship in different groups according to this finding (p=0.32). The mean ± standard deviation in Group 2 was 0.16 ± 0.04.
Alpha angle
Radiographs of three cases in Group 2, three cases in Group 1, and 13 cases in Group 0 showed an alpha angle of more than 50 degrees. The p-value of 0.23 is considered an insignificant correlation. The mean angle was 37.2 ± 9.1 degrees in Group 2.
Herniation pits
Fibrocystic lesion of the femoral neck was seen in 7.1 % of Group 2 cases in comparison to about 1.0 % of cases in Group 0 (p=0.04).
Osteoarthritic changes
These findings are the result of the end stages of FAI. They were seen in only three cases in Group 2 (p=0.05).
Discussion
FAI was first described by Myers et al.'23 as an entity while evaluating the cause of severe pain in patients who had undergone peri-acetabular osteotomy due to hip dysplasia. Nowadays FAI is recognised as a common aetiology of hip injury and osteoarthritis.1
The prevalence of FAI in our study is 11.2%. It is similar to the other study that demonstrated a prevalence of about 10-15% in Germany.16 Patients with FAI had unilateral signs and symptoms but bilateral radiographic abnormalities. It may be concluded that FAI is often bilateral but the symptoms might not be present simultaneously. This finding is also consistent with the study conducted by Tannast et aí.16 Allen et aí.24 describe bilateral lesions in 77-80% of FAI patients with cam lesions.
We have attempted to clarify some controversies and questions about radiographic findings of FAI. From 11 investigated radiographic criteria, only centre-edge angle and secondary radiographic findings, including signs of osteoarthritis and femoral neck herniation pits, had a p-value of less than 0.05. Femoral herniation pits are the result of recurrent FAI in symptomatic patients. Their location is in the anterosuperior part of the femoral neck.1617 Although only two participants in Group 2 (7.1%) had this sign in AP pelvic film, a p-value of 0.04 proved it is a statistically significant correlation. Herniation pits were seen less than in the study by Leunig et aí.118 which was 33%. We think that the fewer herniation pits in our series is due to the small number of cases with FAI.
Reactive ossification of the injured acetabular labrum due to chronic irritation results in accessory ossicle along the superior acetabular rim. Hip osteoarthritic changes and accessory ossicle are seen in the end stage of FAI. Therefore the presence of herniation pits, accessory ossicles and osteoarthritic signs are not helpful in diagnosing FAI early. Moreover, these secondary radiographic findings are not always associated with symptomatic hip impingement.17-22 Also, centre-edge angle is not a practical predictor of FAI because of its low sensitivity of 46.4% and mean angle of 35.3 degrees in FAI cases.
An alpha angle of greater than or equal to 55 degrees was found in all FAI patients by Nötzli et aí.'25 They explain that an alpha angle of 55 degrees should be used as a cut-off point for hip impingement. As mentioned previously, the mean angle in FAI patients in the present study is 37.2 degrees with a p-value of 0.23. This finding is less obvious in Group 2 in comparison to Group 1. These results are in contrast to previous studies.16,25
Radiographic criteria are not sufficient for the accurate diagnosis of FAI in some populations since a significant number of asymptomatic persons with high level activities have abnormal pelvic radiographs. These findings may be related to population-specific life styles such as praying, toileting and even sitting on the ground. It is likely that the hip joint accommodates itself to an extreme range of motion from childhood by making a type of congruent incongruency.
The present investigation suffered from some drawbacks:
• The participants were not well matched according to their demographic data.
• The population of FAI patients was small.
• Only X-ray films were evaluated and other modalities were not considered.
It was concluded that in a population with specific life styles radiographic criteria are not diagnostic of FAI. Other modalities such as magnetic resonance imaging, three-dimensional reconstructions, computed tomography, intra-articular injection of anaesthetic agents and arthroscopy may be more helpful.
Conflict of interest: None
References
1. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003 Dec;417:112-20. [ Links ]
2. Crawford, J.R., Villar, R.N. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005 Nov;87(11):1459-62. [ Links ]
3. Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: Part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004 Jan;418:67-73. [ Links ]
4. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005 Jul;87(7):1012-18. [ Links ]
5. Jaberi FM, Parvizi J. Hip pain in young adults: femoroacetabular impingement. J Arthroplasty. 2007 Oct;22(7 Suppl 3):37-42. [ Links ]
6. Kuhlman GS, Domb BG. Hip impingement: identifying and treating a common cause of hip pain. Am Fam Physician. 2009 Dec;15;80(12):1429-34. [ Links ]
7. Banerjee P, McLean CR. Femoroacetabular impingement: a review of diagnosis and management. Curr Rev Musculoskelet Med. 2011 Mar;16:4(1):23-32. [ Links ]
8. Kaplan KM, Shah MR, Youm T. Femoroacetabular impingement-diagnosis and treatment. Bull NYU Hosp Jt Dis. 2010;68(2):70-75. [ Links ]
9. Ganz R Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001 Nov;83(8):1119-24. [ Links ]
10. Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006 Jul;88(7):1448-57. [ Links ]
11. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006 Apr;25(2):299-308. [ Links ]
12. Byrd JW. Physical examination. In: Operative hip arthroscopy. New York, NY. Springer: 2005:36-50. [ Links ]
13. Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003 Feb;407: 241-48. [ Links ]
14. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007 Sep;5(9):561-70. [ Links ]
15. Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiograph-ic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006 Apr;445:181-85. [ Links ]
16. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis - what the radiologist should know. AJR Am J Roentgenol. 2007 Jun;188(6):1540-52. [ Links ]
17. Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004 Dec;429:170-77. [ Links ]
18. Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005 Jul;236(1):237-46. [ Links ]
19. Emary P. Femoroacetabular impingement syndrome: a narrative review for the chiropractor. J Can Chiropr Assoc. 2010 Sep;54(3):164-76. [ Links ]
20. Beall DP, Sweet CF, Martin HD, Lastine CL, Grayson DE, Ly JQ, Fish JR. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005 Nov;34(11):691-701. [ Links ]
21. Eijer H, Podeszwa DA, Ganz R, Leunig M. Evaluation and treatment of young adults with femoro-acetabular impingement secondary to Perthes' disease. Hip Int. 2006 Oct-Dec;16(4):273-80. [ Links ]
22. McCarthy J, Noble P, Aluisio FV, Schuck M, Wright J, Lee JA. Anatomy, patho logic features and treatment of acetabular labral tears. Clin Orthop Relat Res. 2003 Jan;406:38-47. [ Links ]
23. Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after peri-acetabular osteotomy. Clin Orthop Relat Res. 1999 Jun;363:93-99. [ Links ]
24. Allen D, Beaulé PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009 May;91(5):589-94. [ Links ]
25. Nötzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002 May;84(4):556-60. [ Links ]
 Reprint requests:
Reprint requests:
Reprint requests:
Dr Amir Reza Vosoughi
E-mail: vosoughiar@hotmail.com
Tel/Fax: +98 711 6234504














