Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.12 no.1 Centurion ene. 2013
PEDIATRIC
Tuberculosis of the hip joint region in children
MAF MohideenI; MN RasoolII
IMBChB(Medunsa). Registrar. Nelson Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMBChB(UKZN), FC(Ortho)SA. Paediatric Orthopaedics. Nelson Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
AIM: To describe the clinical and radiological manifestations of tuberculosis of the hip joint and the resemblance to common osteoarticular lesions in children.
METHODS: Thirty-six children (1 to 12 years) were reviewed retrospectively between 1990 and 2011. Clinical, laboratory and radiological features were assessed. The hips were classified and the outcome was graded as described by Shanmugasundaram.
RESULTS: Common clinical features were a limp, flexion, adduction and internal rotation contractures. Common radiological features were osteopaenia and cystic lesions in the neck and acetabulum. Permeative lesions, focal erosions, pathological fractures and sequestra were less common. Seven children had extra-articular lesions. Of the 29 with osteoarticular involvement, six had purely synovial involvement. Osteoarticular lesions mimicked benign bone and joint conditions. Follow-up was 1 to 6 years, 36% were graded as good, 36% fair and 28% had poor outcome with ankylosis. Other complications included avascular necrosis, coxa vara, coxa magna, growth arrest and flexion-adduction contractures.
CONCLUSION: Tuberculosis of the hip can mimic various benign conditions. Biopsy from a bony lesion is important. The initial radiological appearance predicts the outcome, especially in the 'normal' type of hip.
Key words: tuberculosis, hip joint, children
Introduction
Tuberculosis remains a major cause of skeletal infection in developing countries. In 2008 the WHO report ranked South Africa fourth in terms of absolute number of cases.1 There were 9.2 million new cases and 0.7 million HIV-positive cases. In 2010, although there were an estimated 8.8 million new cases of TB, South Africa had the third highest incidence compared to the other 21 high burden countries.2
In the developed world an increase in the number of cases has been reported. This may be attributed to AIDS (acquired immune-deficiency syndrome), immigration and intravenous drug abuse.3 The increase may be due to immuno-modulation and possibly atypical mycobacteria in some cases.4 Skeletal tuberculosis accounts for 10-35% of extra-pulmonary tuberculosis and about 2% of all cases of tuberculosis.5
Most of the literature on tuberculosis of the hip in children is over 40 years old."1 The lesions were mainly destructive. Treatment was by prolonged traction and spica cast. Many surgeons used radical surgery and arthrodesis to control the disease.9-11 The majority of reports are mixed with adults.5,12,13 Only two cases involving the hip joint have been reported recently in a series from the United Kingdom.14 Holland reported one case in 2010.15
The frequency of tuberculosis of the hip joint is next only to that of the spine and constitutes 15% of all cases of osteoarticular tuberculosis. Osteoarticular manifestations may be intra-articular or extra-articular.5 The variable clinical and radiological presentations may mimic common osseous and articular conditions seen in children and delay the diagnosis of tuberculosis.16 Tuberculosis of the hip joint has been rarely reported in the recent literature.17,18
The aims of this study are to report the clinical and radiological patterns of tuberculosis of the hip joint region in children; highlight the resemblance to various osteoarticular lesions; and correlate the radiological appearance with the outcome of treatment.
Materials and methods
Thirty-six children were retrospectively reviewed between 1990 and 2011 at a local hospital. The ages ranged between 1 and 12 (average 6) years. There were 21 boys and 15 girls. All the osteoarticular lesions were histologically confirmed for tuberculosis.
Clinical and radiological data were collected from case records. Haematological tests done for all patients included a full blood count, erythrocyte sedimentation rate and liver function tests. Radiological tests done included routine hip X-ray, chest X-ray and a bone scan. The Mantoux test was done routinely. Five children had computerised tomography scans to define the bone lesions within the hip.
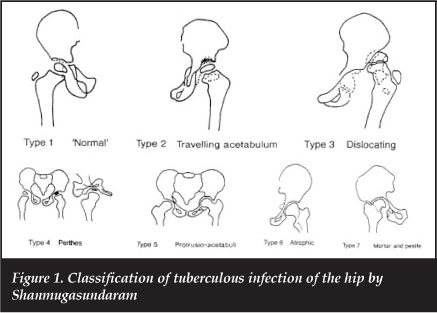
Shanmugasundaram's classification of tuberculosis of the hip joint was used to classify the different radiological patterns of tuberculosis of the hip into seven types13 (Figure 1). All patients had an open biopsy. Debridement, limited synovectomy and curettage of the osseous cavities and defects were performed when bone lesions were present. Antituberculosis treatment was used for a year. This consisted of isoniazide, rifampicin, pyrazinamide and pyridoxine. Post-operatively the hips were immobilised in a spica cast and physiotherapy was commenced after 3 to 4 weeks. Hospital stay ranged between 3 and 8 weeks.
Results
Pain around the hip region and a limp were the main clinical features in all children. Fixed flexion contracture of the hip ranging between 10° and 70° was seen in 28 of the patients. Adduction contracture between 10° and 30° was seen in 27 patients. Three children had discharging sinuses and five had a fluctuant abscess. One child presented with a pathological fracture of the proximal femur.
The albumen was low in eight patients. The chest X-ray showed evidence of pulmonary tuberculosis in 20% of the cases and the bone scan revealed multiple site involvement in two patients with involvement of the elbow and spine respectively. The patients had an ESR ranging between 6-120 mm/hr (average 65 mm/hr). Four patients were known to be infected with HIV and were on antiretrovirals for which they were being followed up by the paediatricians.
The Mantoux test was negative in six children. All patients had histological features consistent with tuberculosis (granulation, caseous necrosis and giant cells).
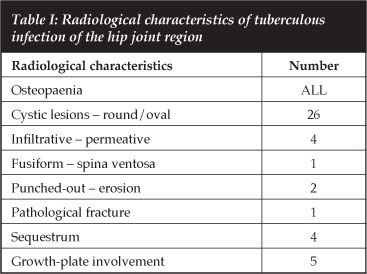
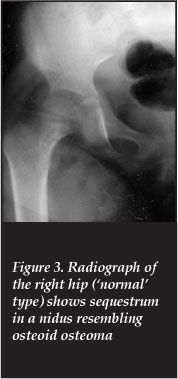
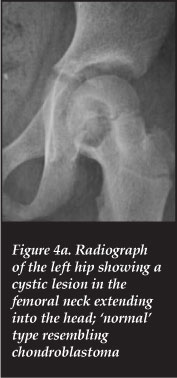
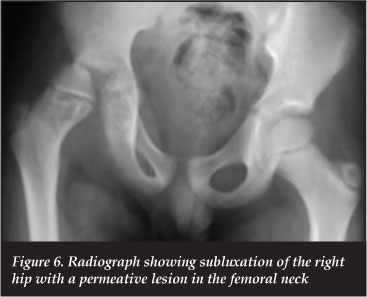
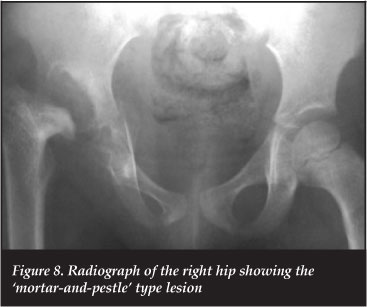
Localised osteopaenia was a common radiological finding. Twenty-six patients had cystic lesions which were either round or oval in shape in the head, neck or acetabulum. Other lesions seen included the infiltrative (permeative), fusiform, punched-out (erosions) and pathologic fractures. In five patients the growth plate was traversed and four had a sequestrum (Table I).
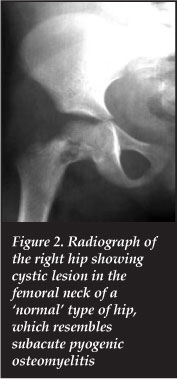
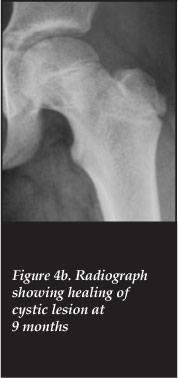
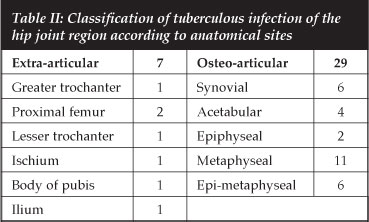
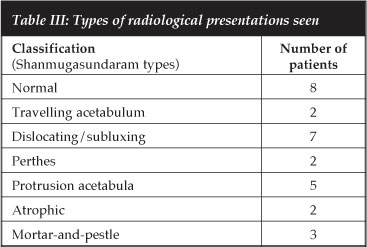
Seven children had extra-capsular tuberculosis and 29 were intra-articular (within the joint capsule) in type. Extra-articular osseous involvement was seen in the proximal femur, greater and lesser trochanter, ilium, ischium and body of the pubis (Table II). Intra-articular infection involved the synovium, acetabulum, epiphysis, metaphysis or the epi-metaphyseal area (Table II). Using the Shanmugasundaram classification there were eight 'normal hips' (Figures 2, 3, 4 and 5), seven dislocating (Figure 6), two travelling acetabulum (Figure 7), two Perthes', five protrusio acetabuli, two atrophic and three mortar-and-pestle types (Figure 8) (Table III). Six hips required extension-abduction-derotation osteotomies for residual flexion adduction deformities. After completion of antituberculous treatment, outcome was graded as good in 36% of the cases, fair in 36% and poor in 28%. All sinuses healed. The pathological fracture healed with immobilisation by six weeks in a spica cast.

Discussion
Tuberculosis of the hip joint in children has a less destructive presentation than was seen in the past. The lesions can present in a synovial or osseous form. The osseous lesions maybe intra-articular, within the joint capsule or extracapsular (extra-articular).5 The clinical and radiological manifestations can imitate rheumatoid arthritis, transient synovitis, septic arthritis and retroviral disease in the synovial form and various benign or malignant bone lesions seen in children in the osseous type.3,416 The intra-articular form may originate from the acetabular or femoral side, and progresses to involve the joint.
The infection can progress through various stages with initial synovitis, effusion and rarefaction, to advanced arthritis with complete destruction. Various radiological appearances are seen, i.e. subluxation, dislocation, erosion, cystic lesions, protrusion and ankylosis.5
Phemister, in a detailed pathological study, found that primary bone involvement in children was usually metaphyseal due to embolism and infarction in metaphyseal end arteries.19 Cavities, cystic lesions, erosions and sequestra may occur. The osseous lesions in this study were mainly metaphyseal appearing as cystic, permeative and focal erosions in the cancellous portions of the femoral head, neck and acetabulum.
Shanmugasundaram proposed a radiological classification for tuberculosis of the hip joint.13 He concluded that the radiological appearance of the hip at presentation almost always predicts the final clinical outcome. He described seven morphological types (Figure I) based on the destructive pattern for all ages. In the 'normal' type, the disease mainly involved the synovium. There may be cysts or cavities in the femoral head, neck or acetabulum, with no gross destruction of the subchondral bone and the joint space remains normal. Eight 'normal hips' with a good outcome were seen in this study. In the 'travelling acetabulum' type, the lesion is in the roof. There is narrowing of the joint space, with progressive upward displacement of the femoral head. These are usually associated with a poor prognosis. Two cases were seen in this study with a fair outcome. In the 'dislocating' type, the head dislocates posteriorly, or subluxes due to laxity of ligaments and capsular distension. The prognosis is poor. Seven cases were seen in this study, with poor results in three. Subluxed hips did well following reduction. In the Perthes' type, the epiphysis is fragmented, dense and flattened. The femoral neck is widened. It resembles Perthes' disease and is probably due to embolic episodes. The prognosis is poor. Fibrous ankylosis was seen in two cases in this study. In the 'protrusio-acetabuli' type, the lesion is mainly in the floor of the acetabulum. With progression, medial displacement of the floor occurs with pressure of the femoral head. The os innominatum gets thinned out in the acetabulum. The prognosis was reported to be good in children. We saw five cases in which the prognosis was fair. Articular cartilage was denuded at surgical exploration. The 'atrophic' hip is characterised by marked narrowing of the joint space.
The differentiation from rheumatoid arthritis and idiopathic chondrolysis is difficult. It has a poor prognosis. Two children with poor results were seen in this study; they developed fibrous ankylosis. In the 'mortar-and-pestle' type, the head of the femur becomes ground down progressively, resembling a pestle within a mortar. Patients still retain a good range of movement. We saw three cases with a fair result.
In this study, only 36% of patients had a good or excellent result. The majority had a fair or poor result. This is due to late presentation with established radiological changes. These hips were mainly of the poor prognostic types, with erosion of the head or acetabulum, dislocation or joint narrowing. The atrophic type had marked joint line narrowing resembling idiopathic chondrolysis. The clinical features were mainly flexion, adduction and internal rotation contractures with subsequent shortening.
Abscesses were seen commonly in the series by Martini.20 They were rare in this study, and occurred over the anterolateral thigh, posteriorly over the glutei, and medially in the adductor region. Sinuses and lymph nodes were also seen rarely. They were more commonly described in the study by Vohra et al.16
The characteristic radiological manifestations of tuberculosis of the hip were osteopaenia and cystic bone lesions varying in size, resembling chondroblastoma, eosinophilic granuloma and subacute pyogenic osteomyelitis. Less commonly seen were infiltrative (permeative) lesions resembling chronic osteomyelitis. Pathological fractures and periosteal reaction were rarely seen.
Versveld and Solomon emphasised that the cystic lesion in bone reflects the major granulomatous lesion, and biopsy material from this area is more representative of tuberculosis than the surrounding synovium which may exhibit a non-specific inflammatory response.21 They found a 41% occurrence of hip involvement in children with osteoarticular tuberculosis, and the cystic lesion was predominant.
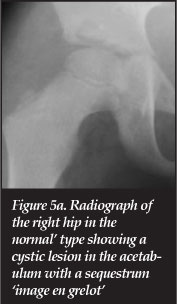
Sequestra are also seen in osteoarticular tuberculosis. A cavity may contain a sequestrum of necrotic spongiosa. Four cases in this study resembled conditions such as osteochondroma and enchondroma. Martini describes these lesions as an 'image en grelot' (little spherical bell) (Figure 5a).20
Bone grafting of cystic lesions was perfomed by Kumar.22 Hosalkar used osteoset pellets to fill bone defects.14 We found that lesions up to 2.5 cm healed spontaneously.
The treatment of osteoarticular tuberculosis includes anti-tuberculosis drugs. Many authors suggest that medical treatment alone is enough. Dosages followed the WHO guidelines. Isoniazide (4-6 mg/kg), rifampicin (8-12 mg/kg), pyrazinamide (20-30 mg/kg) and supplemental pyridoxine (5-10 mg/day) were used in this patient group.
Other authors believe that surgical debridement and drainage is necessary. Wilkinson and Marmor popularised radical synovectomy, debridement, capsulotomy and curettage.23,24 Fusion occurred in eleven per cent of hips, and a large number had coxa magna.23 More recently, Babhulkar and Moon also performed a synovectomy.5,18 Babhulkar emphasised preservation of the articular cartilage and avoidance of total synovectomy to preserve the blood supply to the head. Dislocation of the head was discouraged. Katayama et a/ combined joint debridement with interposition of fascia to facilitate hip movement.25 The results were not encouraging. Vishwakarma interposed a multi-layered cap of amniotic membrane as a biological tissue, in children between the ages of ten and 16 with hip ankylosis. He obtained a stable joint with good function.26 No inflammatory reaction was recorded. However, long-term follow-up is not available.
We used an anterior approach combined with adductor tenotomy and flexor release when contractures were present. Limited synovectomy was performed. Cystic lesions, erosions and infiltrative lesions were routinely curetted and biopsied. Post-operatively the hips were immobilised in abduction of 20-30°. Physiotherapy was commenced after 3-1 weeks.
Traction and mobilisation usually yield good results in early cases. However, it is not adequate in an unstable hip. We used a spica cast for unstable hips and applied an above-knee cast with a broomstick in abduction for four to six weeks in stable hips. Shanmugasundaram used skin traction for up to 22 months.13 Others used skeletal traction.18 Continuous passive motion (CPM) has also been used.17 Although fibrous ankylosis was seen in five patients in this series, spontaneous bony fusion did not occur.
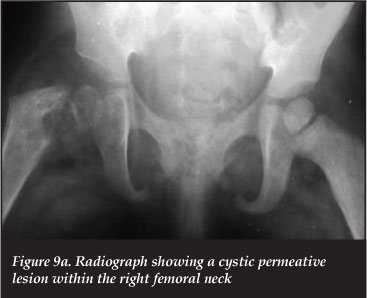
The outcome of tuberculosis of the hip in children depends on the extent of the disease. Tuberculosis of the femoral head and neck may lead to various deformities. Chronic hyperaemia may lead to enlargement of the femoral head epiphysis and metaphysis (coxa magna).27 Lesions of the head and neck can cause avascular necrosis after healing, resulting in reduction of the size of the head and neck (coxa brevia). Three cases were seen in this study. Interference with the growth plate can lead to coxa vara. This deformity may also occur with collapse of the femoral neck (Figures 9a and b).

Tuberculosis of the hip in children has variable radiological manifestations. The osteoarticular lesions have a variable outcome. Pure osseous lesions with an intact joint outline have a good outcome. As in other studies,5,17,18 we found that the radiological morphology at presentation generally predicts the final outcome as suggested by Shanmugasundaram.13 However, the latter study needs to be carried out on a larger scale in relation to several clinical variables. It does not address clinical problems such as flexion, adduction and internal rotation and the role of adductor tenotomy and realignment abduction extension osteotomy. It also does not address lesions in the proximal femur that progress from extra-articular to intra-articular lesions and subsequent complications of coxa vara, avascular necrosis and coxa magna. His patients were immobilised for prolonged periods, some up to 2 years. He did not state whether his patients had biopsies, but stated that surgery provided little benefit. His report combines adults and children. Like Babulkhar, Versveld and Campbell, we advocate open biopsy to provide an accurate diagnosis with limited synovectomy.5,17,21 Pyogenic osteomyelitis and septic arthritis are common in our environment and can resemble tuberculosis in the chronic phase. We found that prolonged immobilisation was not necessary like other studies.17,18
Conclusion
Tuberculosis of the hip region in children can manifest in various radiological forms. Lack of familiarity may lead to a delay in diagnosis and treatment.
No benefits in any form have been received or will be received from any commercial party related directly or indirectly to the subject of this article.
We used an anterior approach combined with adductor tenotomy and flexor release when contractures were present
References
1. Dye C, Floyd K, Uplekar M. WHO report 2008. Global tuberculosis control: surveillance, planning, financing. World Health Organization, Geneva, Switzerland. [ Links ]
2. WHO report 2011. Global tuberculosis control: surveillance, planning, financing. World Health Organization, Geneva, Switzerland. [ Links ]
3. Yao DC, Sartoris DJ. Musculoskeletal tuberculosis. Radiol Clin N Am 1995;33:679-89. [ Links ]
4. Wang MN, Chen WM, Lee KS, et al. Tuberculous osteomyelitis in young children. J Pedr Orthop 1999;19:151-55. [ Links ]
5. Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res 2002;398:93-99. [ Links ]
6. Smith LD. Tuberculosis of the hip in children. J Bone Joint Surg 1926;8:636-42. [ Links ]
7. Hibbs RA. A preliminary report of twenty cases of hip joint tuberculosis treated by an operation devised to eliminate motion by fusing the joint. J Bone and Joint Surg 1926;8:522-33. [ Links ]
8. Wilson JC. Extra-articular fusion of the tuberculous hip joint. California and Western Med 1927;27:774-77. [ Links ]
9. McCarroll HR, Heath RD. Tuberculosis of the hip in children. J Bone Joint Surg 1947;29:889-906. [ Links ]
10. Gruca A, Warsaw P. Treatment of quiescent tuberculosis of the hip joint by excision and 'dynamic' osteotomy. J Bone Joint Surg 1950;32B:174-82. [ Links ]
11. Roberts WM, Webster FS. Early surgical treatment of tuberculosis of the hip in children. Surg Gyne Obstet 1951;92:155-63. [ Links ]
12. Tuli SM, Mukherjee SK. Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. J Bone Joint Surg 1981;63B:29-32. [ Links ]
13. Shanmugasundaram TK (ed). A clinicoradiological classification of tuberculosis of the hip. In: Shanmugasundaram TK. Current concepts in bone and joint tuberculosis. Madras, India: Proceedings of Combined Congress of International Bone and Joint Tuberculosis Club and the Indian Orthop Assoc, 1983, p. 60. [ Links ]
14. Hosalkar HS, Agarwal N, Reddy S, et al. Skeletal tuberculosis in children in the western world: 18 new cases with a review of the literature. J Child Orthop 2009;3:319-24. [ Links ]
15. Holland TS, Sangster MJ, RW Paton, LP Ormerod. Bone and joint tuberculosis in children in the Blackburn area since 2006: a case series. J Child Orthop 2010;4:67-71. [ Links ]
16. Vohra R, Kang HS, Dogra S. Tuberculous osteomyelitis. J Bone Joint Surg 1997;79B:562-66. [ Links ]
17. Campbell JA, Hoffman EB. Tuberculosis of the hip in children. J Bone Joint Surg 1995;77:319-26. [ Links ]
18. Moon MS, Kim SS, Lee SR, Moon YW, Moon JL, Moon SI. Tuberculosis of the hip in children: A retrospective analysis. Ind J Orthop 2012;46: 91-99. [ Links ]
19. Phemister DB. Changes in the articular surfaces in tuberculosis arthritis. J Bone Joint Surg 1925;7: 835-47. [ Links ]
20. Martini M (ed). Tuberculosis of the bones and joints 1988; 111-122 Springer-Verlag, Berlin Heidelberg. [ Links ]
21. Versveld GA, Solomon A. A diagnostic approach to tuberculosis of bones and joints. J Bone Joint Surg 1982;64B:446-49. [ Links ]
22. Kumar K, Saxena MB. Multifocal osteoarticular tuberculosis. Int Orthop 1988;12:135-38. [ Links ]
23. Wilkinson MC. Tuberculosis of the hip and knee treated by chemotherapy, synovectomy and debridement: A follow-up study. J Bone Joint Surg 1969;51A:1343-59. [ Links ]
24. Marmor L, Chan KP, Ho KC. Surgical treatment of tuberculosis of the hip in children. Clin Orthop 1969;67:133-42. [ Links ]
25. Katayama R, Itami Y. Treatment of hip and knee joint tuberculosis. J Bone Joint Surg 1962;44A:897-917. [ Links ]
26. Vishwakarma GK, Khare AK. Amniotic arthroplasty for tuberculosis of the hip joint. J Bone Joint Surg 1986;68B:68-74. [ Links ]
27. Teo EL, Peh WC. Skeletal tuberculosis in children. Paed Radiol 2004;34:853-60. [ Links ]
 Reprints requests:
Reprints requests:
mncwabeh@ukzn.ac.za