Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.12 n.1 Centurion Jan. 2013
SPINE
Anterior surgical correction of thoracolumbar and lumbar scoliosis: efficacy and morbidity
RP DachsI; RN DunnII
IMBChB (UCT). Registrar. Department of Orthopaedic Surgery, University of Cape Town
IIMBChB (UCT), MMed(Orth)UCT, FCS(SA)Orth. Head of Department. Department of Orthopaedic Surgery, University of Cape Town
ABSTRACT
STUDY DESIGN: A retrospective review of adolescent patients undergoing instrumented anterior spinal fusion (ASF) by a single surgeon for thoracolumbar or lumbar (TL/L) scoliosis.
OBJECTIVE: The aim of this study is to investigate the efficacy and associated morbidity of anterior instrumented corrective fusion for thoracolumbar and lumbar scoliosis.
MATERIALS AND METHODS: The medical records and radiographs of 36 consecutively managed patients who underwent anterior spine surgery for thoracolumbar or lumbar curves by a single surgeon between 2001 and 2011 were retrospectively reviewed. The cohort consisted of 26 female and 10 male patients with idiopathic scoliosis as the commonest aetiology. Data collated and analysed included patient demographics, surgical factors, post-operative management and complications. In addition, radiographic analysis was performed on pre-operative and follow-up X-rays, and Scoliosis Research Society (SRS 22) scores were collated.
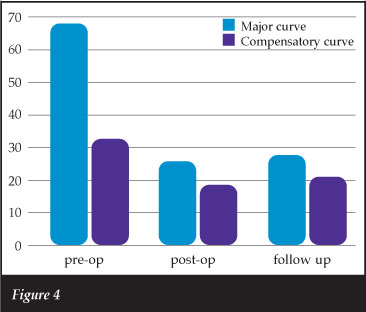
RESULTS: Thoracolumbar/lumbar curves were corrected from 68.4°±18.8° (34°-120°) to 25.9°±16.6° (7°-66°) (average of 62.1% correction). The thoracic compensatory curve spontaneously corrected from 32.8°±14.0° (12°-53°) to 18.4°±14.2° (4°-440) (average of 43.9% correction). Sagittal imbalance of greater than 4 cm was found in 40% of patients pre-operatively and in 16% post-operatively (85% negative sagittal imbalance, 15% positive sagittal imbalance). Rotation according to the Nash-Moe method corrected by 1.2 of a grade (2.37±0.69-1.17±0.58). Average operative time was 194 minutes and estimated blood loss was 460 ml. The diaphragm was taken down in 34 of the 36 patients but no patients required post-op ventilation. The average high care stay was 1.2 days. Average follow-up was 16.9 months. Good maintenance of correction was shown at most recent follow-up, with the mean thoracolumbar/lumbar curve measuring 27.9°±16.7°, and the mean compensatory thoracic curve measuring 20.9°±16.3°. There were no significant neurological or respiratory complications, and no cases had radiological signs of pseudoarthrosis. Scoliosis Research Society scores were obtained in 75% of the idiopathic scoliosis group (18/24), and improved from 75.91 pre-operatively to 84.72 post-operatively. A total of 93.8% were satisfied/very satisfied with their treatment, and 87.5% would probably/definitely have the same treatment again.
CONCLUSION: Anterior corrective fusion for thoracolumbar and lumbar scoliosis is effective in both deformity correction and the maintenance thereof. Spontaneous correction of the thoracic curve can be expected and thus limit the fusion to the lumbar curve. Despite the concerns of taking down the diaphragm, there is minimal morbidity.
LEVEL OF EVIDENCE: Level IV.
Key words: anterior instrumented fusion; surgical correction; thoracolumbar/lumbar scoliosis; efficacy and morbidity; Scoliosis Research Society (SRS 22)
Introduction
Both posterior and anterior instrumented fusions are successfully utilised for the correction of thoracolumbar and lumbar scoliosis. Anterior spinal approaches for thoracolumbar curves are appealing because they facilitate large coronal and rotational correction with shorter segment fusions.1 This results in sparing of distal levels, reduced instrumentation costs and blood transfusion requirements.2 However several studies have voiced concern regarding the associated morbidity after chest cage violation and surgery on the diaphragm."
Whether this approach-related pulmonary function impairment is a clinically significant factor in anterior surgery is controversial. However this concern, together with advances in posterior segmental pedicle screw techniques, has led to an increase in posterior surgery, even for large thoracolumbar curves. The maintenance of surgical correction of the primary structural curve and the compensatory thoracic curve are also a concern with shorter anterior fusions.
We undertook a retrospective review of all our patients who underwent anterior instrumented fusion for thora-columbar and lumbar scoliosis, assessing intra-operative factors, post-operative management and complications, radiological outcomes and Scoliosis Research Society (SRS 22) scores.
Methods
Thirty-six consecutive patients who underwent anterior instrumented fusion for thoracolumbar/lumbar scoliosis between 2001 and 2011 were identified. All procedures were performed by the senior author (RND) at Red Cross Children's Hospital, Groote Schuur Hospital or Constantiaberg Medi-Clinic.
Data was obtained from a surgical database and the medical records and radiographs of the study group. Data captured included patient demographics, aetiology of the scoliosis, radiographic analysis pre-operatively and at various stages post-operatively, operative time and blood loss, number of levels fused, instrumentation used, postoperative requirements and complications, and Scoliosis Research Society (SRS 22) scores.
The cohort consisted of 26 female and 10 male patients. Analysis of aetiology revealed 24 patients with adolescent idiopathic scoliosis, ten with neuromuscular scoliosis, one with scoliosis associated with neurofibromatosis and one with a congenital scoliosis (Figure 1). All patients in the neuromuscular group had myelomeningocoeles, which is generally managed in our unit with a long posterior fusion. The subset included in this study had thoracolumbar or lumbar curves which we elected to manage with a short anterior fusion to avoid the risk of pseudoarthrosis associated with the deficient posterior elements, as well as complications related to poor posterior soft tissue cover.

The average age of the study participants was 12.25±3.54 (6-20) years. The apex of the primary curve was from the T11-12 disc to the body of L3 in all cases.
Radiographic evaluation included whole spine standing postero-anterior and lateral X-rays, supine lateral bending films and traction views as required. All measurements were taken pre-operatively, post-operatively and at final or most recent follow-up. Coronal deformity was measured on the standing PA films using the Cobb method. From the lateral standing radiographs, sagittal balance was assessed in all patients with no neuro-muscular involvement by determining the horizontal distance from the midpoint of C7 to the midpoint of the superior S1 endplate, and recorded as less than or greater than 4 cm.
In the idiopathic group, 22 were classified as Lenke 5, and two as Lenke 6 (Lenke 5 having a thoracolumbar/lumbar major structural curve, Lenke 6 having a thoracolumbar/lumbar major structural curve plus a main thoracic structural curve). Overall, the average coronal Cobb angle of the primary curve was 68.4°±18.8° (34°-120°), and the average coronal Cobb angle of the compensatory thoracic curve was 32.8°±14.0° (12°-53°). The average Nash-Moe grade at the apex of the primary curve was 2.37±0.68.7
Surgical technique
A thoracolumbar approach was used from the side of the convexity. The incision was made along the ninth rib, down to the lateral rectus midway between the umbilicus and pubis. A thoracotomy was performed with resection of the anterior portion of the ninth rib. The cartilaginous component was split and the retroperitoneal space entered. This was developed to expose the psoas. The peritoneum was mobilised off the under-surface of the diaphragm. The diaphragm was then circumferentially cut from the chest wall with diathermy leaving a 5-10 mm rim for later repair (Figure 2). This was carefully done towards the spine to finish at the junction of the psoas and crus. A malleable copper retractor was placed anterior to the spine at each disc level as required to protect the aorta. The psoas was mobilised off the discs and retracted posteriorly. The level was confirmed clinically by counting ribs, identifying the psoas ending on the T12/L1 disc space, and with fluoroscopy.

The discs were then removed along with the cartilaginous component of the endplates taking care not to damage the bony endplate. The posterior annulus was exposed but retained. Screws were then placed into the appropriate bodies parallel to the endplates and posterior body wall, as far posteriorly as possible to maximise screw length (Figure 3). The segmental vessels were retained and simply retracted to place the screws.

A straight rod was used for thoracolumbar curves and a rod contoured for lordosis for lumbar curves. This usually achieved spontaneous reduction of the deformity. Occasionally rod rotation and some fine tuning with compression was required to correct the deformity. If there was residual disc space opening such as in a lordotic segment, rib autograft was applied.
The diaphragm was repaired taking care not to bunch it up medially due to the spontaneous muscle retraction, but to evenly reattach it to the peripheral edge. Abdominal muscles were repaired in two layers. An intercostal drain was inserted into the chest. Spinal cord monitoring was not used in the anterior cases due to the low risk of the shortening procedure.
Results
The average number of levels fused was 6.17±1.30 (range 4-9). Thoracolumbar/lumbar curves corrected from 68.4°±18.8° (34°-120°) to 25.9°±16.6° (7°-66°) (average of 62.1% correction) and the thoracic compensatory curve corrected spontaneously from 32.8°±14.0° (12°-53°) to 18.4°±14.2° (4<M4°) (average of 43.9% correction). Sagittal imbalance of greater than 4 cm was found in 40% of patients pre-operatively and in 16% post-operatively (85% negative sagittal imbalance, 15% positive sagittal imbalance). Rotation according to the Nash-Moe method corrected after surgery by 1.2 of a grade (2.37±0.69-1.17±0.58). Average follow-up was 16.9 months. Good maintenance of correction was shown at most recent follow-up, with the mean thoracolumbar/lumbar curve measuring 27.9°±16.7°, and the mean compensatory thoracic curve measuring 20.9°±15.9°, or a mean correction loss of 2° for both curves (Figures 4 and 5). Radiographic assessment of fusion included assessment for cross trabeculation, loss of correction and lucency around the screws. There were no documented cases of pseudoarthrosis at most recent follow-up. Average operative time was 194 minutes and estimated blood loss was 460 ml. The diaphragm was taken down in 34 of the 36 patients. No patients required post-operative ventilation and the average high care stay was 1.2 days. There were no significant neurological or respiratory complications.

Scoliosis Research Society scores were obtained in 75% of the idiopathic scoliosis group (18/24). Pre-operative scores averaged 75.91 (53.0-94.0±13.9), and post-operative scores averaged 84.72 (70.0-94.6±7.6). A total of 93.8% were satisfied/very satisfied with their treatment, and 87.5% would probably/definitely have the same treatment again.
Discussion
Instrumented anterior spinal fusion allows excellent curve correction and greater correction of rotational deformity while preserving more distal motion segments compared to the posterior approach.2,8 On average one to three distal motion segments can be preserved which may reduce the risk of late degenerative changes caudal to the fusion."1
Other potential advantages of instrumented anterior spinal fusion include a reduced incidence of proximal junctional kyphosis, reduced implant prominence and denervation of posterior spinal extensor muscles, and reduced instrumentation costs.2,12 For these reasons anterior instrumented fusion has historically been the preferred approach for the treatment of thoracolumbar/lumbar scoliosis.13-15
In the only prospective randomised study comparing anterior versus posterior spinal fusion for thoracolumbar/lumbar adolescent idiopathic scoliosis, Wang et al found no significant differences in safety or efficacy between the two approaches. However anterior surgery demonstrated shorter fusion levels, reduced operative time, reduced blood loss and transfusion requirements, and reduced implant and hospitalisation expenses.2
Earlier studies have suggested that approach-related pulmonary function impairment may be a significant factor in anterior surgery. Kumano et al noted that anterior instrumentation and fusion failed to improve or worsened pulmonary function tests at an average of 3.8 years post surgery.16 Wong et al reported that anterior spinal instrumentation and fusion for idiopathic scoliosis revealed a decrease in absolute pulmonary function tests.17
These findings however are largely associated with the surgical correction of thoracic structural curves, and other studies with long-term follow-up have failed to show a sustained decrease in pulmonary function associated with anterior surgery. Verma et al demonstrated that an initial decline in pulmonary function postoperatively resolved fully by 6 to 12 months.18,19 They found absolute and predicted forced vital capacity and forced expiratory volume in 1 second pre-operatively and 2 years post-operatively were unchanged. Kim et al provided evidence that an open thoracotomy for treatment of a main thoracic curve will result in a significant decrease in pulmonary function tests at two years, while the thoraco-abdominal approach for treating a thoracolumbar/lumbar curve does not.20 They recommended posterior rib preservation procedures for Lenke type 1 curves and an anterior procedure for Lenke type 5 and 6 curves if indicated, as pulmonary function was maintained post-operatively.
We do not routinely measure pulmonary function tests as part of our workup. However there were no respiratory complications in our group, and no patient required post-operative ventilation, despite routinely taking down the diaphragm.
Both anterior and posterior approaches provide good correction of deformity.2,12 The average number of levels fused in our patient cohort was 6.17±1.30. This fusion provided a 62.1% correction of the major structural curve (average 42.47°±15.8° correction) with excellent maintenance at most recent follow up (average 16.9 months). The thoracic compensatory curve was not included in the instrumented fusion, and spontaneous correction averaged 43.9% (average 15.48°±7.28° correction). This correction was also maintained at most recent follow-up. Forty per cent of our cohort had significant sagittal imbalance pre-operatively (assessed as >4 cm in C7 plumb line). This was predominantly negative sagittal imbalance (85%). This was reduced to 16% of patients post-operatively. There was also significant correction in the axial plane. Pre-operative rotation measured according to the Nash-Moe method corrected from 2.37±0.69 to 1.17±0.58 post-operatively.
Conclusion
Instrumented anterior spinal fusion is a successful, safe and reliable procedure for the correction of thoracolumbar and lumbar scoliosis. It provides effective deformity correction and good maintenance of the correction. Fusion can be limited to the major structural curve, with reliable spontaneous correction of the thoracic curve. There is no significant morbidity associated with taking down the diaphragm. Our study lends further weight to the growing body of evidence that anterior surgery for thoracolumbar/lumbar scoliosis does not result in clinically significant pulmonary morbidity.
The study was approved by the Department of Surgery Research Committee of the Health Sciences Faculty, University of Cape Town, reference 2012/014.
References
1. Majd ME, Castro FP, Holt RT. Anterior fusion for idiopathic scoliosis. Spine 2000;25:696-702. [ Links ]
2. Wang Y, et al. Anterior spinal fusion versus posterior spinal fusion for moderate lumbar/thoracolumbar adolescent idiopathic scoliosis. Spine 2008;33:2166-72. [ Links ]
3. Lamarre A, Hall JE, Weng TR, et al. Pulmonary function in scoliosis one year after surgical correction. In: Proceedings of the Scoliosis Research Society. J Bone Joint Surg Am 1971;53:195. [ Links ]
4. Kumano K, Tsuyama N. Pulmonary function before and after surgical correction of scoliosis. J Bone Joint Surg Am 1982;64:242-48. [ Links ]
5. Wong CA, Cole AA, Watson L, et al. Pulmonary function before and after anterior spinal surgery in adult idiopathic scoliosis. Thorax 1996;51:534-36. [ Links ]
6. Graham EJ, Lenke LG, Lowe TG, et al. Prospective pulmonary function evaluation following open thoracotomy for anterior spinal fusion in adolescent idiopathic scoliosis. Spine 2000;25:2319-25. [ Links ]
7. Nash CL Jr, Moe JH. A study of vertebral rotation. J Bone Joint Aurg Am 1969; 51: 223-29. [ Links ]
8. Gupta M, Puno RM, Merita S, et al. Zielke instrumentation for the treatment of thoracolumbar and lumbar curves in idiopathic scoliosis: Revised [Abstract]. rthop Trans 1984;18:119. [ Links ]
9. Betz RR, Harms J, Clements DH, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic. Spine. 1999;24:225-39. [ Links ]
10. Ginsberg HH, Goldstein LA, Robinson SC, et al. Back pain in postoperative idiopathic scoliosis long-term follow-up study. Spine 1979;4:518. [ Links ]
11. Cochran T, Irstam L, Nachemson A. Long-term anatomical and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine 1983;8:576-84. [ Links ]
12. Hee H, Yu Z, Wong H. Comparison of segmental pedicle screw instrumentation versus anterior instrumentation in adolescent idio-pathic thoracolumbar and lumbar scoliosis. Spine 2007;32:1533-42. [ Links ]
13. Kaneda K, Fujiya N, Satoh S. Results with Zielke instrumentation for idiopathic thoracolumbar and lumbar scoliosis. Clin Orthop Relat Res 1986;19^203. [ Links ]
14. Luk KD, Leong JC, Reyes L, et al. The comparative results of treatment in idiopathic thoracolumbar and lumbar scoliosis using the Harrington, Dwyer, and Zielke instrumentations. Spine 1989;14:275-80. [ Links ]
15. Giehl JP, Volpel J, Heinrich E, et al. Correction of the sagittal plane in idiopathic scoliosis using the Zielke procedure (VDS). Int Orthop 1992;16:213-18. [ Links ]
16. Kumano K, Tsuyama N. Pulmonary function before and after surgical correction of scoliosis. J Bone Joint Surg Am 1982;64:242-48. [ Links ]
17. Wong CA, Cole AA, Watson L, et al. Pulmonary function before and after anterior spinal surgery in adult idiopathic scoliosis. Thorax 1996;51:534-36. [ Links ]
18. Verma K, Lonner B, et al. Maximal pulmonary recovery after spinal fusion for adolescent idiopathic scoliosis. Spine 2011;36:1086-95. [ Links ]
19. Verma K, Auerbach J, et al. Anterior spinal fusion for thoracolum-bar scoliosis: comprehensive assessment of radiological, clinical, and pulmonary outcomes on 2-years follow-up. J Pediatr Orthop 2010;30:664-69. [ Links ]
20. Kim YJ, Lenke LG, Bridwell KH, et al. Prospective pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am 2005;87:1534-41. [ Links ]
 Reprint requests:
Reprint requests:
Prof RN Dunn
info@spinesurgery.co.za
ERRATUM
SA Orthopaedic Journal Summer 2012 volume 11 number 4
Figures 6 to 9 were inadvertently omitted from the article 'Circular external fixator application for midshaft tibial fractures' by Drs N Ferreira, PH Mare and LC Marais in the printed version of SA Orthopaedic Journal Summer 2012 volume 11 number 4.
The omission has been rectified in the online version of the article, which can be found on the SA Orthopaedic Association website: www.saoa.org.za. Click on 'Publications', 'SA Orthopaedic Journal', then 'SAOJ online'.
Go the top of the screen, click on 'all' to see all the issues of SAOJ, select 2012, volume 11 number 4, then click on the article to read the corrected version.
Alternatively, visit the SciELO website: www.scielo.org.za. Click on 'alphabetic list' and then click on 'SA Orthopaedic Journal', and continue as above.
The publisher apologises to the authors and the readers for this oversight.














