Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.11 no.4 Centurion Jan. 2012
CASE SERIES AND REVIEW OF THE LITERATURE
Bell's cruciate paralysis: a rare neurological diagnosis
M LaubscherI; PH NaudéII; M HeldIII; R DunnIV; N KrugerV
IMBChB, Dip PEC. Hospital and the Department of Orthopaedics, University of Cape Town, South Africa
IIRegistrar. MBChB. Hospital and the Department of Orthopaedics, University of Cape Town, South Africa
IIIRegistrar DrMed. Hospital and the Department of Orthopaedics, University of Cape Town, South Africa
IVRegistrar. MBChB, MMed(Orth), FCS(SA)Orth. Hospital and the Department of Orthopaedics, University of Cape Town, South Africa
VProfessor and Head BSc, MBChB, FRCS(Edinburgh), FCS(SA)Orth Consultant. Hospital and the Department of Orthopaedics, University of Cape Town, South Africa
ABSTRACT
Bell's cruciate paralysis is a rare incomplete spinal cord syndrome characterised by brachial diplegia. It is caused by an insult to the cervicomedullary junction of the spinal cord. We report three cases of cruciate paralysis following traumatic injury to the cervical spine. In all three cases the clinical diagnosis of cruciate paralysis was confirmed with magnetic resonance imaging (MRI). The prognosis varies according to the underlying cause, but is generally good. The clinical diagnosis of cruciate paralysis helps localise the injury to the cervicomedullary junction.
Key words: cruciate paralysis, brachial diplegia, cervicomedullary junction, incomplete spinal cord syndrome, decussation
Introduction
Bell first described 'cruciate paralysis' in 1970.1 The syndrome is caused by an insult to the cervicomedullary junction at the upper part of the pyramidal decussation. Patients with cruciate paralysis present with paresis or paralysis of their upper limbs without significant involvement of their lower limbs.
We present three cases of cruciate paralysis following traumatic injury that presented to our unit over a period of 18 months.
Case series
Case 1
An 18-year-old male patient was transferred from a peripheral hospital one day after being injured in a rugby match. He was diagnosed with an upper cervical spine injury and a possible brachial plexus injury at the referring institution. His cervical spine was immobilised in a rigid collar.
On admission he was fully orientated. His only injury was a type 3 odontoid peg fracture with minimal displacement.
Careful neurological examination revealed weakness of his upper limbs (C5-T1), with the right side weaker than the left. He also had slight weakness of his right leg. There was no sensory deficit.
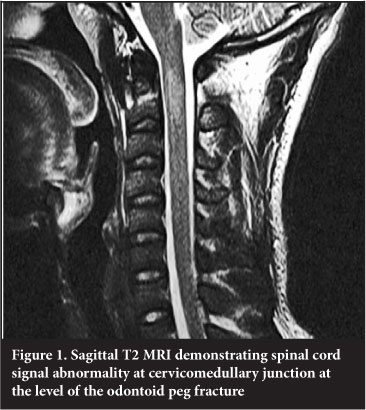
MRI confirmed the injury and revealed swelling and oedema of the spinal cord at the craniocervical junction (Figure 1).
The diagnosis of cruciate paralysis was made.
The patient was treated with traction in Cone's callipers for six weeks. Upon removal of the traction a Philadelphia collar was applied for another six weeks. His neurological deficit improved in traction and upon discharge his ASIA motor score was 90 (improved from 76 on admission). He had no complications from the treatment.
Case 2
A 16-year-old female patient presented to our trauma unit following a diving accident. She was diagnosed with a cervical spine injury with partial neurological deficit. She had no other injuries.
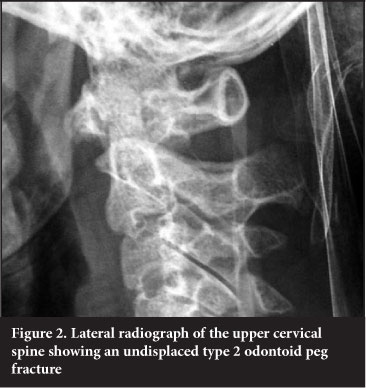
She sustained an undisplaced type 2 odontoid peg fracture (Figures 2 and 3). On neurological examination she had weakness of both arms, left weaker than right, involving the C5 to T1 distribution. Sensation was intact. The only other abnormality on neurological examination was a slight decrease in strength of hip flexion on the right side.

MRI showed a signal abnormality of the spinal cord at the level of the cervicomedullary junction.
She was treated with traction in Cone's callipers for six weeks and placed in a Philadelphia collar for a further six weeks. Her weakness improved during her admission. Her odontoid peg fracture united and she had no complications from her treatment. Her ASIA motor score improved to 92 on discharge (from 74 on admission).
Case 3
A 26-year-old male patient was transferred from a referral institution with a decreased level of consciousness following an assault to the head with a blunt object. He was intubated and ventilated.
On neurological examination he had a decreased level of consciousness with a Glascow Coma Scale (GCS) of 9T/15. His pupils were equal and reactive. He had no movement of his upper limbs, but was moving both his lower limbs on command. He had no obvious sensory deficit.
A computed tomography (CT) scan of his brain showed a subarachnoid haemorrhage with some generalised cerebral oedema, an interhemispheric subdural haematoma and a right zygomatic arch fracture. Radiographs and a CT scan of his cervical spine showed no fractures or dislocations.
Because the intracranial injuries could not explain the neurologic picture, a possible central cord syndrome was suspected and an MRI scan was obtained. MRI revealed a Chiari 1 malformation and bulbous dens. It also showed a signal abnormality of the spinal cord at the junction of the medulla and the proximal cord. There were no ligamentous or other injuries at this level. The diagnosis of a Bell's cruciate paralysis was made.
The patient was treated non-operatively for his head injury. He was placed in a Philadelphia collar as a precautionary measure. After extubation he remained confused and restless, but the motor function in his upper limbs improved. After five days the patient's ASIA motor score improved to 92 (from 68 on admission) and he was transferred to a rehabilitation facility.
At three-month follow-up he had made a full neurological recovery.
Discussion
When there is complete loss of neurological function distal to the level of a spinal cord injury, the injury is said to be functionally complete. Functionally incomplete injuries include a variety of syndromes, which describe distinct patterns of neurological symptoms. Intricate knowledge of the anatomy of the spinal cord is necessary to understand and diagnose these syndromes.2 Incomplete spinal cord syndromes are relatively common complications of injuries to the cervical spine.
Although Nielsen in his textbook on clinical neurology from 1941 refers to isolated upper limb paralysis, Bell was the first to describe 'cruciate paralysis' as a clinical entity in 1970.1 He presented a case series of four cases. Three of these cases presented with more severe upper limb paralysis following insults to the cervicomedullary junction. One case presented with lower limb weakness more than upper limb following surgery to the posterior fossa and upper cervical spine. From this he described what he called 'cruciate paralysis' as paralysis of both arms without significant paralysis of the legs resulting from injury to the junction of the medulla and the cervical spinal cord.1 Various case studies and series have subsequently validated this clinical entity.3-27 Sensory deficit can occur.3 Transient respiratory insufficiency, urinary retention, and associated deficit of a single or multiple cranial nerves have been described.3 The spinal accessory nerve is the cranial nerve most commonly affected, although other cranial nerves can be affected as well.3,21
Wallenberg in 1901 first described the complexity of the neuroanatomy of the corticospinal tracts at the cervicomedullary junction.1 The corticospinal tract is the main motor pathway mediating voluntary movement. It originates in the primary motor cerebral cortex.
The tract then runs through the internal capsule before reaching the brainstem. At the lower medulla oblongata it approaches the midline and crosses to the contralateral side at the pyramidal decussation.4 Here the corticospinal tract of the upper extremity supposedly descends more medially and anteriorly relative to that of the lower extremity (Figure 4). The segment level of the pyramidal decussation of the corticospinal tract of the upper extremity is located proximal to the level of the foramen magnum, which is approximately one cord segment proximal to that of the lower extremity. A percentage of corticospinal fibres (20%) remain ipsilateral and form the anterior corticospinal tract. The fibres that cross form the lateral corticospinal tract, which runs down the spinal cord to the last sacral segments. These fibres synapse at segmental levels onto motor neurons, which control fine movements of distal extremities.2,4

Bell and other authors explained cruciate paralysis by this supposed separate organisation of the upper and lower limb fibres within the corticospinal tracts at the level of the pyramidal decussation.1 It was thought that the crossing upper limb motor neurons were placed in a position more anterior and medial relative to the lower-extremity fibres; hence, insult to this region would selectively affect the upper limbs. This theory has since been disputed.5 Following work from other authors, Pappas et al isolated the forelimb and hindlimb fibres in two different monkey species and traced them. No evidence of differential decussation of the fibres was found and he therefore concluded there is no obvious anatomical explanation for cruciate paralysis.
He did propose two alternative explanations: selective damage to neural areas involving the internuncial cells, the central grey area and the cuneate nucleus, or injury to the anterior corticospinal tract. Evidence for these alternate theories is also lacking.5 The presentation of cruciate paralysis is similar to that of a central cord syndrome. Schneider et al in 1954 described central cord syndrome from traumatic hyperextension of the upper cervical spine. It was thought to result from compression of the cervical cord between bony spurs anteriorly and a rolled ligamentum flavum posteriorly in the already narrowed canal of the degenerate cervical spine.6 In central cord syndrome the upper limbs are always affected more than the lower limbs, although the lower limbs are commonly affected as well. The cranial nerves are never involved. The main difference between the two entities is the precise anatomical location of the lesion leading to the syndromes.7,8,9 In cruciate paralysis, the lesion is thought to lie in a very specific area within the pyramidal decussation. The presence of associated cranial nerve palsies further aid to localise the lesion to the cervicomedullary junction.3,21 In central cord syndrome, the medial fibres of the lateral corticospinal tract, as well as lower motor neurons in the anterior horns, may be affected by the injury. It is thus more commonly associated with injuries to the subaxial cervical spine.7,8,9 Some authors suggest that the two entities should rather be grouped together.10 Another neurological syndrome that can be confused with cruciate paralysis is 'man-in-barrel' syndrome (MBS).11 MBS refers to brachial diplegia associated with cerebral vascular disorders, although other aetiologies have been described.11,12
In cruciate paralysis MRI can be helpful in localising the lesion to the cervicomedullary junction.28 MRI might show oedema or contusion in this area.
Dickman et al examined the possible radiographic localisation of injury in 14 patients diagnosed with cruciate paralysis. Interestingly in four of the seven patients where a MRI was obtained the MRI had no abnormal findings.3
Bell's cruciate paralysis has been described following various different insults to the cervicomedullary junction (Table I).1-3,7,8,13-30 Chiari 1 malformations might predispose individuals to spinal cord injuries, including incomplete spinal cord syndromes.14,17,28

There is no specific treatment for cruciate paralysis. The cause must be treated appropriately. The prognosis also varies according to the underlying cause but is generally good.3 Residual deficits are usually mild and complete recovery is possible as described.
Cruciate paralysis is a clinical diagnosis that can guide the clinician to the area of pathology and again shows the importance of careful neurological evaluation of the spinal injured patient. This will help avoid missing the often subtle neurological signs. In return, suspecting or diagnosing Bell's cruciate paralysis localises a lesion to the cervicomedullary junction and can aid in the diagnosis of the underlying pathology.
The content of this article is the sole work of the authors. No benefits in any form have been or are to be received from a commercial party related directly or indirectly to the subject of this article.
References
1. Bell HS. Paralysis of both arms from injury of the upper portion of the pyramidal decussation: 'cruciate paralysis. J Neurosurg 1970 Oct;33(4):376-80. [ Links ]
2. Levi ADO. Approach to the patient and diagnostic evaluation. In: Winn HR, Youmans JR (eds). Youmans Neurological Surgery. WB Saunders; 2004:4871. [ Links ]
3. Dickman CA, Hadley MN, Pappas CT, Sonntag VK, Geisler FH. Cruciate paralysis: a clinical and radiographic analysis of injuries to the cervicomedullary junction. J Neurosurg 1990 Dec;73(6):850-58. [ Links ]
4. Vulliemoz S, Raineteau O, Jabaudon D. Reaching beyond the midline: why are human brains cross wired? Lancet Neurol 2005 Feb;4(2):87-99. [ Links ]
5. Pappas CT, Gibson AR, Sonntag VK. Decussation of hind-limb and fore-limb fibers in the monkey corticospinal tract: relevance to cruciate paralysis. J Neurosurg 1991 Dec;75(6):935-40. [ Links ]
6. Schneider RC, Cherry G, Pantek H. The syndrome of acute central cervical spinal injury. J Neurosurg 1954;11:546-77. [ Links ]
7. Sweet J, Ammerman J, Deshmukh V, White J. Cruciate paralysis secondary to traumatic atlantooccipital dislocation. J Neurosurg Spine 2010 Jan;12(1):19-21. [ Links ]
8. Inamasu J, Hori S, Ohsuga F, Aikawa N. Selective paralysis of the upper extremities after odontoid fracture: acute central cord syndrome or cruciate paralysis? Clin Neurol Neurosurg 2001 Dec;103(4):238-41. [ Links ]
9. Levi AD, Tator CH, Bunge RP. Clinical syndromes associated with disproportionate weakness of the upper versus the lower extremities after cervical spinal cord injury. Neurosurgery 1996 Jan;38(1):179-83; discussion 183-85. [ Links ]
10. Ciappetta P, Salvati M, Raco A, Artico M. Cruciate hemiplegia: a clinical syndrome, a neuroanatomical controversy. Report of two cases and review of the literature. Surg Neurol 1990 Jul;34(1):43-47. [ Links ]
11. Georgiadis D, Schulte-Mattler WJ. Cruciate paralysis or man-in-the-barrel syndrome? Report of a case of Brachial Diplegia. Acta Neurol Scand 2002;105:337-40. [ Links ]
12. Orsini M, Mello MP, Nascimento OJM, Melo R, CH De Freitas MRG. Man-in-the-barrel syndrome: history and different etiologies. Rev Neurocienc 2009;17(2):138-40. [ Links ]
13. Berck DJ, Mussalli GM, Manning FA. Atraumatic fetal cervical spinal cord injury and cruciate paralysis. Obstet Gynecol 1998 May;91(5 Pt 2):833-834. [ Links ]
14. Bondurant CP, Oro JJ. Spinal cord injury without radiographic abnormality and Chiari malformation. J Neurosurg 1993 Dec;79(6):833-38. [ Links ]
15. Bruni P, Greco R, Hernandez R, Piazza G, Paolucci GC, Matticari A, et al. Cruciate paralysis from a Jefferson's fracture. Report a case and review of the literature. J Neurosurg Sci 1994 Mar;38(1):67-72. [ Links ]
16. Coppola AR. 'Cruciate paralysis': a complication of surgery. South Med J 1973 Jun;66(6):684. [ Links ]
17. da Silva JA, da Costa MD, Leal AB, dos Reis FR, de Queiroz RB. Cruciate hemiplegia associated with basilar impression, Arnold-Chiari malformation and syringomyelia. Case report. Arq Neuropsiquiatr 1996 Dec;54(4):669-72. [ Links ]
18. Dai L, Jia L, Xu Y, Zhang W. Cruciate paralysis caused by injury of the upper cervical spine. J Spinal Disord 1995 Apr;8(2):170-72. [ Links ]
19. Dickman CA, Sonntag VK. Cruciate paralysis after a traumatic upper cervical spine injury. Spine (Phila Pa 1976) 1992 Oct;17(10):1268. [ Links ]
20. Dumitru D, Lang JE. Cruciate paralysis. Case report. J Neurosurg 1986 Jul;65(1):108-10. [ Links ]
21. Kuitwaard K, Vandertop WP. A patient with an odontoid fracture and atrophy of the tongue: a case report and systematic review of the literature. Surg Neurol 2005 Dec;64(6):525-32, discussion 532-33. [ Links ]
22. Ladouceur D, Veilleux M, Levesque RY. Cruciate paralysis secondary to C1 on C2 fracture-dislocation. Spine (Phila Pa 1976) 1991 Dec;16(12):1383-85. [ Links ]
23. Marano SR, Calica AB, Sonntag VK. Bilateral upper extremity paralysis (Bell's cruciate paralysis) from a gunshot wound to the cervicomedullary junction. Neurosurgery1986 May;18(5):642-44. [ Links ]
24. Yayama T, Uchida K, Kobayashi S, Nakajima H, Kubota C, Sato R, et al. Cruciate paralysis and hemiplegia cruciata: report of three cases. Spinal Cord 2006 Jun;44(6):393-98. [ Links ]
25. Zeidman SM, Ducker TB. Rheumatoid arthritis. Neuroanatomy, compression, and grading of deficits. Spine (Phila Pa 1976) 1994 Oct 15;19(20):2259-66. [ Links ]
26. Landau WM. Cruciate paralysis. Neurosurgery 1986 Oct;19(4):676. [ Links ]
27. Landau WM. Cruciate paralysis. J Neurosurg 1992 Aug;77(2):329-30. [ Links ]
28. Erlich V, Snow R, Heier L. Confirmation by magnetic resonance imaging of Bell's cruciate paralysis in a young child with Chiari type I malformation and minor head trauma. Neurosurgery 1989 Jul;25(1):102-105. [ Links ]
29. Chen TY. The clinical presentation of uppermost cervical disc protrusion. Spine (Phila Pa 1976) 2000 Feb 15;25(4):439-42. [ Links ]
30. Faillace WJ, Guthrie T. Recovery from Cruciate Paralysis Due to Axial Subluxation from Metastatic Breast Carcinoma: A Case Report. Breast J 2000 Mar;6(2):139- 42. [ Links ]
 Reprint requests:
Reprint requests:
Dr M Laubscher
Email: maritzl@msn.com














