Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.11 no.4 Centurion Jan. 2012
CLINICAL ARTICLE
Posterior vertebral column resection for severe spinal deformities
S AbdullahI; N EnricoII; RN DunnIII
IMS(Orth) UM (University Malaya). Spine Fellow
IIMaster of Nursing, Monash University, Australia Research assistant
IIIMBChB(UCT), MMed(Orth), FCS(SA)Orth. Professor and Head of Department Division of Orthopaedic Surgery, University of Cape Town
ABSTRACT
STUDY DESIGN: A retrospective review of patient records and imaging.
OBJECTIVES: The purpose of this study is to review the indications, surgical challenges and outcomes of patients undergoing posterior vertebral column resection (PVCR).
SUMMARY OF BACKGROUND DATA: PVCR is indicated in the management of severe rigid spine deformities. It is a complex surgical procedure and is only performed in a few spine centres due to the technical expertise required and associated risk.
METHODS: Twelve patients with severe spinal deformities who underwent PVCR were retrospectively reviewed after a follow-up of 2 years.
Surgery was performed with the aid of motor-evoked spinal cord monitoring and cell saver when available. The average surgical duration was 307 minutes (100-490 ± 126.3). The average blood loss was 1350 ml (4OO-3OOO ± 897.9).
The indication for PVCR was gross deformity and myelopathy which was due to congenital spinal deformities and old tuberculosis (TB). Clinical records and the radiographic parameters were reviewed.
RESULTS: Kyphosis of an average of 73° was corrected to 29° and coronal Cobb was corrected from an average of 48° to 22°.
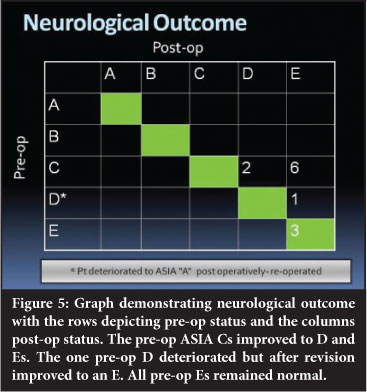
Ten patients improved neurologically to ASIA D and E. One patient deteriorated immediately post-operatively, required revision with no initial improvement but reached ASIA E by 6 months post-op.
Four patients had associated syringomyelia. All were re-scanned at 1 year. The three with small syrinxes demonstrated no progression on MRI and a large syrinx resolved completely.
In addition to the neurological deterioration, complications included one right lower-lobe pneumonia.
CONCLUSION: PVCR is an effective option to correct complex rigid kyphoscoliosis. In addition it allows excellent circumferential decompression of the cord and neurological recovery. When the congenital scoliosis is associated with syringomyelia with no other cause evident, it may allow resolution of the syrinx.
Key words: posterior vertebral column resection, severe spinal deformities, paraparesis
Introduction
Posterior vertebral column resection (PVCR) is a relatively new procedure in the management of severe spinal deformities. This complex surgical procedure is only performed in a few spine centres due to the technical expertise required but is promoted for use in rigid severe spinal deformities.1-4
Previously this surgery was performed using two separate approaches, viz. anterior decancellation and posterior corrective fusion. This has associated morbidity and contributes to a high risk of major complications.3 Zhou et al.5 concluded that a combined anterior and posterior approach is safer compared to posterior vertebral column resection, although there was compromised pulmonary function with the dual approach due to the lengthy time of operation. An anterior and posterior approach offers limited correction in severe deformities.3
Suk et al.1 claim that PVCR will reduce complications, time, effort and blood loss during surgery. They also conclude that this procedure is more reliable, avoiding the complications attributed to the anterior approach. Lenke et al.2 add that this procedure has the ability to correct the deformity to a larger extent as PVCR allows translational and rotational correction of the spinal column. By shortening the column, there is less distractive risk to the cord. In this study, the authors have reviewed the indications, surgical challenges and outcomes of patients undergoing PVCR.
Materials and methods
Between 2003 and 2012, 12 consecutive patients underwent a posterior only VCR at four different institutions, viz. Groote Schuur Hospital, Red Cross Children's Hospital, Constantiaberg Medi-Clinic and Frere Hospital in the Eastern Cape. All patients were operated on by the senior author (RD).
Institutional DRC and ethics approval was obtained for the study 226/2012.
Surgical technique
The surgical technique of a PVCR is challenging and demanding. It requires the technical expertise of the surgical team with an advanced knowledge of spinal deformities procedures. Patients were positioned either on a Relton-Hall frame or OSI 'Jackson' (Orthopedic System Inc, Union City, CA) operative table. All pressure points were adequately identified and padded to avoid excessive pressure as the procedure can be lengthy. Freedom from abdominal compression was ensured to avoid venous distension. A cell saver was used when available as was trans-cranial motor-evoked potential spinal cord monitoring.
Routine sub-periosteal exposure of the vertebral column was performed. Pedicle screws were inserted using the freehand technique. When there was concern as to direction, laminotomies were performed to palpate the pedicle medially. Rigid screws were used routinely to maximise implant strength and correction but polyaxial screws were used on occasion to facilitate rod application in severe rotation.
A wide laminectomy was performed centrally over the apical levels which were resected. This provides adequate exposure of the thecal sac and promotes the surgeon's orientation of the deformity, increasing safety during decompression. It also allows visualisation of dural impingement during the correction process.
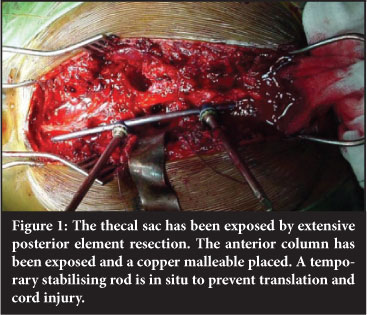
Before the anterior column was resected a temporary stabilising rod was placed using at least two to three pedicle screws both above and below the area to be resected (Figure 1). The vertebral column resection was initiated by gaining access to the cancellous bone of the vertebral body through a lateral pedicle body entrance. Concave resection of the deformity allowed the spinal cord to drift medially and reduce tension. Then the convex part of the corpectomy was performed. Discectomies were performed at the extreme ends to prepare the endplates for subsequent fusion.
Finally the posterior vertebral body wall was removed from anterior to the thecal sac.
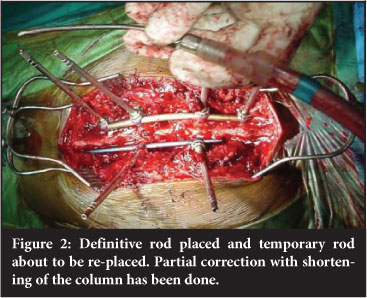
Epidural bleeding was controlled with bipolar cauterisation and topical haemostatic agents such as surgicel and cottonoid patties. Once the resection was complete, definitive rods were applied, an allograft strut or mesh cage inserted into the anterior column defect and the correction performed (Figure 2). The column was shortened and compressed onto the strut/cage. When the gap was too small, morcellised graft was placed into the anterior defect. During closure the ventral thecal sac was repeatedly checked to make sure it was free of any bony impingement.
All patients were stabilised adequately with instrumentation allowing early mobilisation without a brace. On average they were discharged after seven days.
Results
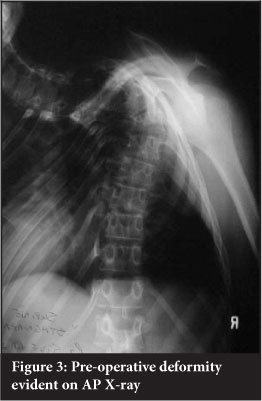
Kyphosis was corrected from an average of 73° (35-130 ± 30.9) to 29°(10-65 ± 16.8) and the coronal Cobb angle from an average of 48° (24-89 ± 21) to 22° (7-44 ± 10.0) (Figures 3 and 4). The average surgical time was 307 minutes (100-490 ± 126.3 min). The average blood loss was 1 350 ml (400-3000 ± 897.9 ml) (Tables I and II).

Of the seven patients with myelopathy, all improved from ASIA C to ASIA E except for one who improved to ASIA D (Figure 5). One patient deteriorated post op from an ASIA D to an ASIA A. An MRI was performed which confirmed residual anterior thecal sac compression. Revision decompression was performed with extension of the anterior column resection. Despite the initial complete neurological picture clinically, he slowly recovered to normal neurological status (ASIA E) by 6 months after surgery.
One patient had a right lower-lobe pneumonia post-oper-atively.
Four patients had associated syringomyelia. All were re-scanned at 1 year. The three with small syrinxes demonstrated no progression. A large syrinx resolved completely (Figures 6 and 7).


Discussion
The surgical treatment of severe rigid spinal deformities is challenging. The use of a vertebrectomy was first performed by MacLennan in 1922.6 He described a posterior apical resection followed by postoperative casting for the treatment of severe scoliosis. Bradford7 described the use of a circumferential vertebrectomy in patients with severe structural spinal deformities via anterior decancellation and posterior fusion. Suk8 promoted the posterior only VCR technique due to a reduction in operating time and blood loss.
He reported on 16 patients with an average age of 29 years who underwent a posterior VCR. Complications were encountered in four patients, including one with complete permanent paralysis. He recommended this as an effective alternative for severe rigid scoliosis but cautioned that it was a highly technical procedure and should only be performed by an experienced surgical team.
Our series on 12 consecutive patients undergoing posterior only VCR for severe paediatric spinal deformity confirms the effectiveness in deformity correction and neurological improvement. However, the complexity of the procedure necessitates an experienced team of surgeons and anaesthetists to perform this procedure adequately and safely. The use of cell saver and spinal cord monitoring are highly recommended, although it is accepted that these modalities are not always available. In fact one of our cases was done on an outreach programme with limited access to sophisticated equipment and an excellent outcome, but this places additional stress on the team.
Conclusion
A PVCR is an extremely effective surgical treatment for severe spinal deformities in terms of kyphosis and scoliosis correction. In addition, it allows adequate thecal sac decompression with high expectancy of improvement in neurological status. It is relatively safe in a well-resourced environment but remains a challenging and complex procedure which requires highly technical expertise of the surgical team. Intra-operative spinal cord monitoring is almost mandatory to minimise neurological deterioration due to the corrective component as is use of a cell saver to address the anticipated large blood loss.
Key points
- PVCR is an effective surgical treatment for severe spinal deformities with fewer complications.
- It requires technical expertise of the surgical team due to its complex, challenging surgical technique and its associated risk.
- The use of spinal cord monitoring is essential to monitor neurologic function during this challenging procedure.
Acknowledgement
The authors thank Ms Marilyn van den Berg for her assistance with the data collection.
Other than institutional research support, the authors have not received any direct funding related to this article.
References
1. Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine 2002;27(21):2374-82. [ Links ]
2. Lenke LG, O'Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke K.M. Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine 2009; 34(20):2213-21. [ Links ]
3. Hamzaoglu A, Alanay A, Ozturk C, Sarier M, Karadereler S, Ganiyusufoglu S. Posterior vertebral column resection in severe spinal deformities. Spine 2011;36(5):340-44. [ Links ]
4. Xie J, Wang Y, Zhao Z, Zhang Y, Si Y, Yang Z, Liu L, Lu N. One stage and posterior approach for correction of moderate to severe scoliosis in adolescents associated with chiari 1 malformation: is a prior suboccipital decompression always necessary? Eur Spine J 2011;20:1106-13. [ Links ]
5. Zhou C, Liu L, Song Y, Liu H, Li T, Gong Q, Zeng J, Kong Q. Anterior and posterior vertebral column resection for severe and rigid idiopathic scoliosis. Eur Spine J 2011;20:1728-34. DOI 10.1007/s00586-011-1861-z. [ Links ]
6. MacLennan A. (1922). Scoliosis. Br Med J 1922;2:865-66. [ Links ]
7. Bradford DS. Vertebral column resection. Orthop Trans 1987;11:502. [ Links ]
8. Suk SI, Chung ER, Lee SM, Lee JH, Kim SS, Kim JH. Posterior vertebral column resection in fixed lumbosacral deformity. Spine 2005;30:703-10. [ Links ]
 Reprint requests:
Reprint requests:
Prof RN Dunn
Department of Orthopaedic Surgery
H49 OMB
Groote Schuur Hospital Observatory 7925
Email: prof@spinesurgery.co.za














