Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.11 n.3 Centurion Jan. 2012
CASE REPORT AND REVIEW OF THE LITERATURE
Infantile tuberculous osteomyelitis of the proximal tibia involving the growth plate
WB HiddemaI; BW BarnardII; W BouaichaIII; D HurterIV; GD van der LindeV; CA van der WesthuizenVI; PB YeroVII
IMBChB Community Service Medical Officer, Department of Orthopaedics. Kimberley Hospital, Kimberley, Free State
IIMBChB Medical Officer, Department of Radiology. Kimberley Hospital, Kimberley, Free State
IIIOrthopaedic Specialist (Tunisia); Consultant, Department of Orthopaedics. Kimberley Hospital, Kimberley, Free State
IVMBChB, MMed(DRad) Head: Department of Radiology. Kimberley Hospital, Kimberley, Free State
VMBChB, MMed(Path) Consultant, Department of Pathology. Kimberley Hospital, Kimberley, Free State
VIIMBChB, MMed(Ortho), FCS(Ortho)SA Head: Department of Orthopaedics. Kimberley Hospital, Kimberley, Free State
VIIIOrthopaedic Specialist (Cuba); Consultant, Department of Orthopaedics. Kimberley Hospital, Kimberley, Free State
ABSTRACT
With an ever-increasing prevalence of tuberculosis (TB) in Sub-Saharan Africa it is now more important than ever to consider tuberculosis when drawing up a list of differentials in musculoskeletal disease. We present a case of infantile tuberculous osteomyelitis of the proximal tibia involving the growth plate.
Key words: Musculoskeletal tuberculosis, tuberculous osteomyelitis, epiphyseal tuberculosis, metaphyseal tuberculosis, extrapulmonary tuberculosis
Case report
A 22-month-old boy presented with a three-month history of a painful mass over his left lower leg following a fall onto his left knee.
Further history revealed a previously healthy child with a normal birth developmental history. All his vaccinations, including BCG, were up to date.
Of note in the history was the fact that his mother had been diagnosed with pulmonary tuberculosis (TB) and started on treatment two months prior to his presentation to us. The child had been subsequently screened for tuberculosis with a Mantoux skin test at his local clinic which was positive. He was then also started on initial phase anti-TB chemotherapy consisting of rifampicin, isoniazid and pyrazinamide. Both mother and child were compliant with their treatment. General and systemic examination was normal.
The local examination revealed an obvious swelling over the medial aspect of his left proximal tibia with normal overlying skin and no focal temperature change. The mass was fluctuant, minimally tender and non-pulsatile on palpation and without an associated knee effusion. The child had a normal gait and full painless passive range of motion of his left knee. No neurovascular compromise of his left lower limb was noted. The left hip and ankle joints were normal.
The infective markers were not significantly raised: Erythrocyte sedimentation rate (ESR) was 20 ml hour and C-reactive protein (CRP) was 5.1. The leucocyte count was 9.49 χ 109/L with a normal differential count.
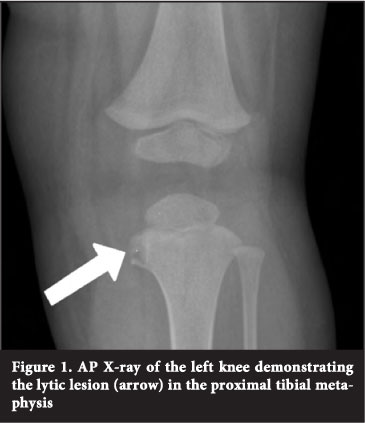
On the AP X-ray of the left knee moderate soft tissue swelling over the medial aspect of the left knee was seen, as well as a lytic lesion measuring 0.5 cm χ 1 cm on the medial aspect of the proximal tibial metaphysis (Figure 1).
MRI revealed a cold abscess, originating in the proximal tibial epiphysis and extending transphyseal into the metaphysis as well as into the surrounding soft tissues. No effusion or articular involvement was noted (Figure 2).

A provisional diagnosis of TB osteomyelitis was made and the child was subsequently taken to theatre for incision, drainage and curettage.
Intra-operatively a thick-walled abscess cavity containing serous fluid was found in the soft tissues on the medial aspect of the left proximal lower leg with a tractus extending into the growth plate (Figure 3). The fluid was aspirated for MCS and biopsies were taken for histopathological evaluation.

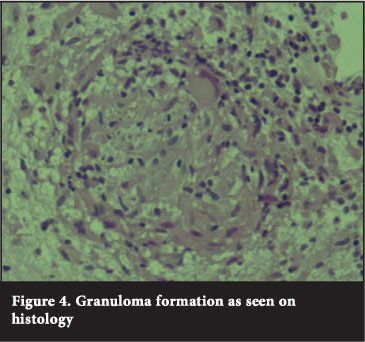
Histological examination confirmed tuberculous granulomas with Langhans giant cells (Figure 4). No acid-fast bacilli were seen with microscopy and culture results were negative, which could be attributed to the fact that the patient had already been on anti-TB chemotherapy for two months prior to the biopsy.
Post-operatively the child recovered well and was discharged on continuation phase anti-TB chemotherapy (rifampicin and isoniazid) for another 9 months.
The importance of monitoring the child's growth over the next several years was discussed with the parents.
Literature review
In 2009, 9.4 million new cases of tuberculosis were reported.1 Skeletal tuberculosis accounts for around 10 to 20 per cent of all extrapulmonary TB cases and only between 1 and 2 per cent of all TB cases.2 However concurrent pulmonary TB is present in less than 50 per cent of skeletal tuberculosis cases in children.3 The axial skeleton is most commonly involved in adults, while peripheral skeletal involvement is more common among children.4 The commonly affected sites in TB osteomyelitis are, in order of frequency, the spine, femur, tibia and fibula.5
TB bacilli reach the proximal tibia by haematogenic spread resulting in a metaphyseal focus. In children younger than one-and-a-half years further spread to the epiphysis occurs through the patent transphyseal vessels from this metaphyseal focus.2 A concomitant septic arthritis can result following drainage of an epiphyseal abscess into the joint through the articular surface, and physeal involvement is explained by direct spread from an adjacent metaphyseal or epiphyseal abscess.
In most cases, the diagnosis of tuberculous osteomyelitis is delayed by up to 6 months. It usually presents as swelling only or swelling and stiffness or pain.6
Radiological signs include, but are not limited to: changes in the joint space, subchondral erosions, lytic bone lesions and articular osteopaenia.7 Markers of acute infection or inflammation including ESR and CRP are elevated but are non-specific.8 A definite diagnosis must be made by biopsy and culture.7,9
Treatment can consist of either TB chemotherapy alone or surgical debridement and TB chemotherapy, but many authors believe TB chemotherapy alone for 9 to 12 months to be sufficient.9,10
Even though open curettage is widely performed and accepted as the norm, Takashi et al provide an interesting minimally invasive endoscopic technique to minimise physeal damage with curettage of transphyseal lesions.
They conclude that there may be potential advantage in the use of endoscopic rather than open methods of debridement of such lesions.11
Osteomyelitis of the proximal tibia can potentially have devastating long-term complications such as premature joint degeneration and longitudinal growth disturbance. Premature joint degeneration follows epiphyseal destruction while longitudinal growth disturbance is a result of physeal destruction. Song and Kim12 reported on three cases of non-tuberculous osteomyelitis involving the proximal tibial epiphyses with an eight to 22-year follow-up. They conclude that the epiphysis has remarkable potential for recovery and regeneration and therefore advise expectant management of the bony epiphyseal defects. However, with regard to the physeal destruction, they advise an early osteotomy (before 4 years) to correct angular deformities as recurrence of angular deformity was not seen in their longterm follow-up and the growth plate can recover its potential for symmetrical growth once normal alignment has been restored.
Kozo et al13 report a case of a 30-month-old infant with TB of the proximal tibia involving the growth plate, where extensive surgical curettage of the growth plate was initially done resulting in no long-term growth abnormalities. This emphasises once again the tremendous potential of the physis to withstand the damage caused by both the infection and the surgical curettage and the ability to continue with symmetrical growth after such an insult.
Discussion
As is evident from the aforementioned literature, infantile tuberculous osteomyelitis of the proximal tibia is only very rarely encountered.
This article serves as a reminder that in order to make an early diagnosis of TB osteomyelitis in children, a high index of suspicion is needed, and it should definitely be included on the list of differentials in children with musculoskeletal complaints of swelling and stiffness. Furthermore it should be kept in mind that the absence of pulmonary TB does not exclude the diagnosis of infantile tuberculous osteomyelitis.
Long-term anti-TB chemotherapy following initial debridement yields good short-and long-term results as seen in several case reports, with only a few growth-related complications. As it is a rare condition further reports with long-term follow-up are warranted. This will provide us with adequate data enabling us to better comment on the prognosis regarding long-term growth disturbances in children with TB osteomyelitis involving the physis.
No benefit has been received by the authors of this article and no perverse incentives were offered to the patient and/or family.
References
1. World Health Organization. Report on global tuberculosis control. 2010. http://whqlibdoc.who.int/publications/2010/ 9789241564069_eng.pdf [ Links ]
2. Morris BS, Varma R, Gang A, et al. Multifocal musculoskeletal tuberculosis in children: appearances on computed tomography. Skeletal Radiol 2002; 31:1-8. [ Links ]
3. Teo HEL, Peh WCG. Skeletal tuberculosis in children. Pediatric Radiol 2004; 34:853-60. [ Links ]
4. Vohra R, Kang HS, Dogra S, Saggar RR, Sharma R. Tuberculosis osteomyelitis. J Bone Joint Surg [Br] 1997; 79:562-66. [ Links ]
5. Vallejo JG, Ong LT, Starke JR. Tuberculous osteomyelitis of the long bones in children. Paediatr Infect Dis J 1995; 14:52426. [ Links ]
6. Chen SC, Huang SC, Wu CT. Non-spinal TB osteomyelitis in children. J Formos Med Assoc 1998; 97(1): 26-31. [ Links ]
7. Hosalkar HS, Agrawal N, Reddy S, Sehgal K, Fox EJ, Hill RA. Skeletal tuberculosis in children in the Western world: 18 new cases with a review of the literature. J Child Orthop 2009; 3(4):319-24. [ Links ]
8. Gunasekera TMR, Karunathilake DH, Jayaweera KAHM. A rare presentation of tuberculous osteomyelitis in childhood. Sri Lanka Journal of Child Health 2008; 37:61-62. [ Links ]
9. Rasool MN. Osseous manifestations of tuberculosis in children. J Paediatric Orthop 2001; 21(6):746-55. [ Links ]
10. Monach PA, Daily JP, Rodriguez-Herrera G, Solomon DH. Tuberculous osteomyelitis presenting as shoulder pain. J Rheumatol 2003; 30(4):851-56. [ Links ]
11. Takashi S, Makoto K, Atsuya W, Nobuyasu O, Kazuhisa T. Endoscopic Surgery for Chronic Osteomyelitis Extending Across the Physis: A Report of Two Cases. J Bone Joint Surg [Am] 2008; 90(8):1744-50. [ Links ]
12. Song KS, Kim HKW. Regeneration of the proximal tibial epiphysis after infantile osteomyelitis: report of three cases with an eight to 22 year follow-up. J Bone Joint Surg [Br] 2005 87(7):979-83. [ Links ]
13. Kozo O, Hideji K, Toshihiko Y, Naoki O. Long-term follow-up of tuberculosis of the proximal part of the tibia involving the growth plate: A case report. J Bone Joint Surg [Am] 2007;89(2):399-403. [ Links ]
 Reprint requests:
Reprint requests:
Dr WB Hiddema
Email: wim.hiddema@gmail.com
Tel: (+27)72 289 7072














