Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.11 n.3 Centurion Jan. 2012
CLINICAL ARTICLE
Metal-on-metal arthroplasty using the Metasul prosthesis with a minimum ten-year follow-up
JG MyburghI; C SnyckersII; Z OschmanIII; TMonniIV
IMBChB, MMed Orth, FCS(SA)Orth. Department of Orthopaedics, Steve Biko Academic Hospital. University of Pretoria
IIMBChB, MMed Orth, FCS(SA)Orth. Department of Sports Medicine University of Pretoria
IIIMBChB, DCH, MSc Sports. Department of Sports Medicine University of Pretoria
IVMBChB. Department of Orthopaedics, Steve Biko Academic Hospital. University of Pretoria
ABSTRACT
Despite concern in recent literature about the adverse effects and complications of metal-on-metal total hip replacements, we have obtained excellent results ten to 15 years after metal-on-metal total hip arthroplasty in 11 out of 12 patients (91.66%) that were available for clinical follow-up. We could trace 15 out of a total of 18 patients (88.33%). Three patients died between the nine- and ten-year follow-up. All our available patients were clinically examined using the Harris Hip Score; hip radiographs; ultrasound and blood investigations. Only one patient (8.33%) needed revision surgery. This information can be used to reassure both orthopaedic surgeons and patients who had metal-on-metal total hip arthroplasty performed in the past that not all metal-on-metal total hip replacements need to be revised. We would advise that if patients present with symptoms or signs they should be thoroughly examined clinically and radiologically, and undergo laboratory investigations, before considering revision surgery.
Key words: Hip, arthroplasty, metal on metal, bearing surface, results, adverse effects
Purpose of the study
Recent literature raised concern about the adverse effects and complications following metal-on-metal bearing surfaces. The following adverse effects were observed in patients with a metal-on-metal articulation, namely: osteol-ysis,1-3 incidence of pseudotumours,4,5-11 aseptic lymphocyte proliferation,4,12,13 groin pain,14-17 metal allergy15,18-20 and raised blood and urine chromium (Cr) and cobalt (Co) levels.21-28 The purpose of this study was to follow up a cohort of patients that received a metal-on-metal total hip replacement with minimum follow-up of ten years and to evaluate them clinically and radiologically, as well as evaluating their blood chromium and cobalt results and to compare our results with the literature.29-31
Methods
A good clinical history was obtained in all available patients that underwent metal-on-metal total hip replacements during 1996 to 2000 using a 28 mm Metasul prosthesis with a minimum follow-up of ten years. They were clinically examined and evaluated with the Harris Hip Score; hip X-rays; full blood count (FBC); C-reactive protein (CRP); liver function tests (LFT); urea, creatinine and electrolytes (U,K & E); blood and urine chromium and cobalt levels and ultrasonic examination of the hip. The ultrasound was done by an independent experienced ultrasonographer in each case to exclude pseudotumours or fluid collections. Out of a total of 18 patients 12 were alive and could be contacted and a good clinical history was obtained. Three of the 18 patients died of natural causes unrelated to their hip prosthesis between 2008 and 2010. They had not needed any revision hip surgery. Another three patients were lost to follow-up. We were able to examine 11 patients clinically and radiologically using the Harris Hip Score, radiographic examinations and ultrasound. The blood and urine chromium and cobalt levels, full blood count, CRP, LFT and U,K & E were also done on these patients. One patient was interviewed telephonically due to the fact that he lives a long distance from our institution. He is still happy with his replaced right hip after 15 years and due to lack of complaints and symptoms he considered it unnecessary to travel to our institution. A primary hip replacement of his opposite hip was done elsewhere two years ago.
The weakness of the study is the small number of patients which does not allow statistical analysis.
Results
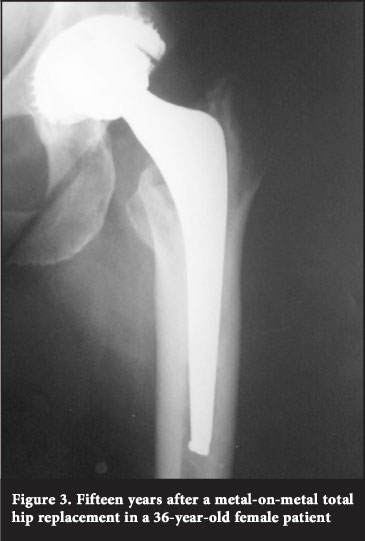
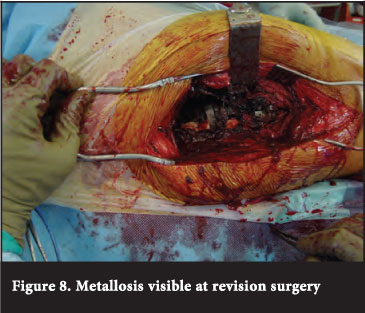
The average Harris Hip Score was 91.5 (54-100). There were no signs of osteolysis or loosening on radiographic examination in 10 (91.7%) of our patients (Figures 1-4). One patient had radiolucent lines and osteolysis on radiographic examination. The same patient had a 92 mm fluid collection localised lateral and distal to the greater trochanter and a prominent effusion of his hip with an anterior posterior diameter of 22 mm and associated synovitis that was visible on ultrasound. The patient subsequently underwent a revision total hip arthroplasty for component loosening and metalosis. The ultrasonographist could not detect any soft tissue masses or fluid collections in the remaining patients.



The mean blood Cr level was 1.92 microg/l (<0.5-14.4 microg/l) and the mean blood Co level was 6.66 microg/l (3.0-15.1 microg/l) (Figure 5). The mean urine Cr was 43.3 microg/l (<0.9-447.9 microg/l) and the mean urine Co was12.21 microg/l (<0.8-71.6 microg/l) (Figure 6). The Co/Cr ratio was 4 microg/g (0.8-11.0 microg/g). There was one exception if all the results were compared.


Discussion
The development of a locally destructive non-neoplastic mass or 'pseudotumour' is not new and has been reported on since the early history of hip arthroplasty, even with metal-on-polyethylene bearing couplings.32 Unfortunately, due to the accelerated search for improved bearing couplings, product withdrawals due to poor results are also not new to arthroplasty.33 This often leads to an aggressive and sometimes exaggerated response from surgeons, at times fuelled by medico-legal concerns. The recent concerns raised about metal-on-metal total hip arthroplasty is another such event.1-20 Although there are currently serious questions being raised as to the validity of metal-on-metal total hip arthroplasty, care should be taken not to include all designs and bearing couplings under the same umbrella. The concept of metal-on-metal failures, pseudotumour development, and metal ion levels is currently a topic of debate and a complete understanding of the complicated biotribological environment is still evasive. As the differential studies indicate, the carbon carbide concentration can have a significant effect on the development of failures.34 Manufacturing techniques can also adversely affect wear particle generation as seen in the early failures with the Birmingham Hip Resurfacing (BHR).35 Serum ion development is also not only seen in the realm of metal-on-metal arthroplasty, as the development of significant serum ion levels have been reported in metal-on-polyethylene total knee arthroplasty.36 Serum ion levels are however higher in metal-on-metal bearing couplings but can show a varying fluctuation that is still not well understood and a universal safe level has not yet been established.37,38
Local destructive non-neoplastic mass or pseudotumour development is also a complex phenomenon with a seemingly multifactorial aetiology.39 Wear particle generation does however seem to be central in the initiation, development or propagation of Adverse Reaction to Metal Debri (ARMD) or Aseptic Lymphocytic Vasculitis Associated Loosening (ALVAL).40 This has led to investigations into inclination angles, anteversion angles and coupling angles.41 Furthermore, certain design features can increase the development of pseudotumours, as evident in the reduced angle of articulation of the recently withdrawn Articular Surface Replacement (ASR).42
The similarity between ALVAL and a type IV hypersensitivity reaction also points to a complex immunological cascade in the development of pseudotumours.
The question can thus be raised: What about current patients with metal-on-metal total hip arthroplasty?
It is thus clear that our understanding of the complex factors surrounding metal-on-metal total hip arthroplasty is still developing and that a reactionary response to a product recall should be avoided. Not all metal-on-metal bearing couplings have been recalled and many are still functioning well. The current controversies surrounding metal-on-metal bearing couplings limits the present use of this bearing surface and ideally metal-on-metal total hip arthroplasty should be reserved for centres of research.
Although some of the Metasul metal-on-metal bearing couplings have recently shown evidence of failures at 12-year follow-up, good medium-term results have been reported using this bearing coupling.43,44
In our series investigating patients ten to 15 years after metal-on-metal total hip arthroplasty, we obtained excellent Harris Hip Scores: no signs of prosthetic loosening or peri-prosthetic osteolysis on radiographs and no signs of pseudotumours on ultrasonic examination in 11 (91.66%) patients who were available for follow-up were present. There was no reason for concern when looking at their blood investigations. The exception was a patient who had a revision of the femoral component and a titanium plate following a peri-prosthetic fracture. The acetabular implant was retained. The patient subsequently developed loosening and a pseudotumour. At the second revision it was found that the loose titanium plate caused local tissue damage and reaction. The patient was revised with an uncemented prosthesis with a crosslinked polyethylene liner and a chromium-cobalt femoral head (Figures 7-9).
 s
s

The remaining patients had excellent Harris Hip Scores and their implants showed no osteolysis or radiological signs of loosening. We advise that patients who had metal-on-metal total hip prostheses should be instructed to visit their orthopaedic surgeon when experiencing any clinical symptoms or signs that may be related to the surgery. If the clinical examination, radiographic examination, serial blood investigations and ultrasound examination are normal and the patient still complains of hip pain, MRI or CT studies may be indicated. Surgeons can reassure patients who had previous metal-on-metal hip replacements that not all of them need revision, but should be followed up on a regular basis and properly investigated if they experience clinical symptoms and signs. We would advise proper clinical, radiological and laboratory examinations prior to any revision surgery. The choice of prosthesis remains difficult and controversial in the active young male patient but metal-on-metal may still be considered as an alternative.29 In female patients less than 40 years of age, metal-on-metal total hip prosthesis should not be considered as they are most likely to develop adverse reactions or loosening according to Glyn-Jones.6
Conclusion
Despite the recent concern about serious adverse effects and complications, we obtained good-to-excellent results after a minimum ten years' meticulous follow-up in 11 out of 12 patients (91.66%).
This information can be used to reassure both surgeons and patients that had metal-on-metal total hip arthroplasties performed in the past that not all need to be revised. The patients should be followed up on a regular basis and properly investigated if they experience clinical symptoms and signs. We would advise a proper clinical, radiological and laboratory examinations prior to any revision surgery.
We do recommend careful selection of patients, detailed attention to surgical technique, positioning of the prosthesis and close follow-up when considering a metal-on-metal articulation. Patients should be counselled about the possibility of tissue reaction and future revision surgery.
As for the future, the Editors of the SAOJ would like to refer orthopaedic surgeons to the memorandum circulated to all orthopaedic surgeons by our President, Prof TLB le Roux.
The content of this article is the sole work of the authors. No benefits of any form have been derived from any commercial party related directly or indirectly to the subject of this article.
References
1. Park YS, Moon YW Lim SJ, Yang JM, Ahn G, Choi YL. Early osteolysis following second-generation metal-on-metal hip replacement. J Bone Joint Surg Am. 2005 Jul;87(7):1515-21. [ Links ]
2. Carr AM, DeSteiger R. Osteolysis in patients with a metal-on-metal hip arthroplasty. ANZ J Surg. 2008 Mar;78(3):144-47. [ Links ]
3. Huber M, Reinisch G, Zenz P, Zweymuller K, Lintner F. Postmortem study of femoral osteolysis associated with metal-on-metal articulation in total hip replacement: an analysis of nine cases. J Bone Joint Surg Am. 2010 Jul;92(8):1720-31. [ Links ]
4. Kwon YM, Thomas P, Summer B, Pandit H, Taylor A, Beard D, Murray DW, Gill AS. Lymphocyte proliferation responses in patients with pseudotumors following metal-on-metal hip resurfacing arthroplasty. J Orthop Res. 2010 Apr;28(4):444-50. [ Links ]
5. Clayton RA, Beggs I, Salter DM, Grant MH, Patton JT, Porter DE. Inflammatory pseudotumor associated with femoral nerve palsy following metal-on-metal resurfacing of the hip. A case report. J Bone Joint Surg Am. 2008 Sep;90(9):1988-93. [ Links ]
6. Glyn-Jones S, Pandit H, Kwon YM, Doll H, Gill HS, Murray DW. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br. 2009 Dec;91(12):1566-74. [ Links ]
7. Grammatopolous G, Pandit H, Kwon YM, Gundle R, McLardy-Smith P, Beard DJ, Murray DW Gill AS. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009 Aug;91(8):1019-24. [ Links ]
8. Malviya A, Holland JP. Pseudotumours associated with metal-on-metal hip resurfacing: 10-year Newcastle experience. Acta Orthop Belg. 2009 Aug;75(4):477-83. [ Links ]
9. Molvik H, Hanna SA, de Roeck NJ. Failed metal-on-metal total hip arthroplasty presenting as painful groin mass with associated weight loss and night sweats. Am J Orthop. 2010 May;39(5):E46-49. [ Links ]
10. Pandit H, Vlychou M, Whitwell D, Crook D, Luqmani R, Ostlere S, Murray D, Athanasou N. Necrotic granulomatous pseudotumours in bilateral resurfacing hip arthoplasties: evidence for a type IV immune response. Virchows Arch. 2008 Nov;453(5):529-34. [ Links ]
11. Watters TS, Eward WC, Hallows RK, Dodd LG, Wellman SS, Bolognesi MP. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty: a case report. J Bone Joint Surg Am. 2010 Jul;92(7):1666-69. [ Links ]
12. Zustin J, Amling M, Krause M, Breer S, Hahn M, Morlock MM, Ruther W, Sauter G. Intraosseous lymphocytic infiltrates after hip resurfacing arthroplasty: a histopathological study on 181 retrieved femoral remnants. Virchows Arch. 2009 May;454(5):581-88. [ Links ]
13. Aroukatos P, Repanti M, Repantis T, Bravou V, Korovessis P. Immunologic adverse reaction associated with low-carbide metal-on-metal bearings in total hip arthroplasty. Clin Orthop. 2010 Aug;468(8):2135-42. [ Links ]
14. Bin Nasser A, Beaule PE, O'Neill M, Kim PR, Fazekas A. Incidence of groin pain after metal-on-metal hip resurfacing. Clin Orthop. 2010 Feb;468(2):392-99. [ Links ]
15. Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty 2008 Oct;23(7):1080-85. [ Links ]
16. Hart AJ, Sabah S, Henckel J, Lewis A, Cobb J, Sampson B, Mitchell A, Skinner JA. The painful metal-on-metal hip resurfacing. J Bone Joint Surg Br. 2009 Jun;91(6):738-44. [ Links ]
17. Shahrdar C, Campbell P, Mirra J, Dorr LD. Painful metal-on-metal total hip arthroplasty. J Arthroplasty 2006 Feb; 21(2):289-93. [ Links ]
18. Biant LC, Bruce WJ, van der Wall H, Walsh WR. Infection or allergy in the painful metal-on-metal total hip arthroplasty? J Arthroplasty 2010 Feb;25(2):334.e11-334.e16. [ Links ]
19. Perumal V, Alkire M, Swank ML. Unusual presentation of cobalt hypersensitivity in a patient with a metal-on-metal bearing in total hip arthroplasty. Am J Orthop. 2010 May;39(5):E39-41. [ Links ]
20. Thomas P, Braathen LR, Dorig M, Aubock J, Nestle F, Werfel T, Willert HG. Increased metal allergy in patients with failed metal-on-metal hip arthroplasty and peri-implant T-lymphocytic inflammation. Allergy 2009 Aug;64(8): 1157-65. [ Links ]
21. Hart AJ, Skinner JA, Winship P, Faria N, Kulinskaya E, Webster D, Muirhead-Allwood S, Aldam CH, Anwar H, Powell JJ. Circulating levels of cobalt and chromium from metal-on-metal hip replacement are associated with CD8+ T-cell lymphopenia. J Bone Joint Surg Br. 2009 Jun;91(6):835-42. [ Links ]
22. Brodner W, Bitzan P, Meisinger V, Kaider A, Gottsauner-Wolf F, Kotz R. Serum cobalt levels after metal-on-metal total hip arthroplasty. J Bone Joint Surg Am. 2003 Nov;85-A(11):2168-73. [ Links ]
23. Isaac GH, Brockett C, Breckon A, van der Jagt D, Williams S, Hardaker C, Fischer J, Schepers A. Ceramic-on-metal bearings in total hip replacement: whole blood metal ion levels and analysis of retrieved components. J Bone Joint Surg Br. 2009 Sep;91(9):1134-41. [ Links ]
24. Lhotka C, Szekeres T, Steffan I, Zhuber K, Zweymuller K. Four-year study of cobalt and chromium blood levels in patients managed with two different metal-on-metal total hip replacements. J Orthop Res. 2003 Mar;21(2):189-95. [ Links ]
25. Rasquinha VJ, Ranawat CS, Weiskopf J, Rodriguez JA, Skipor AK, Jacobs JJ. Serum metal levels and bearing surfaces in total hip arthroplasty. J Arthroplasty 2006 Sep;21(6 Suppl 2):47-52. [ Links ]
26. Vendittoli PA, Roy A, Mottard S, Girard J, Lusignan D, Lavigne M. Metal ion release from bearing wear and corrosion with 28 mm and large-diameter metal-on-metal bearing articulations: a follow-up study. J Bone Joint Surg Br. 2010 Jan;92(1):12-19. [ Links ]
27. Witzleb WC, Ziegler J, Krummenauer F, Neumeister V Guenther KP. Exposure to chromium, cobalt and molybdenum from metal-on-metal total hip replacement and hip resurfacing arthroplasty. Acta Orthop. 2006 Oct;77(5):697-705. [ Links ]
28. Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJ. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: a controlled study. J Bone Joint Surg Br. 2007 Mar;89(3):301-305. [ Links ]
29. Engh CA,Jr, Ho H, Engh CA. Metal-on-metal hip arthroplasty: does early clinical outcome justify the chance of an adverse local tissue reaction?. Clin Orthop. 2010 Feb;468(2):406-12. [ Links ]
30. Della Valle CJ, Nunley RM, Raterman SJ, Barrack RL. Initial American experience with hip resurfacing following FDA approval. Clin Orthop. 2009 Jan;467(1):72-78. [ Links ]
31. De Smet KA. Belgium experience with metal-on-metal surface arthroplasty. Orthop Clin North Am. 2005 ix; Apr;36(2):203-13. [ Links ]
32. Harris WH, Schiller AL, Scholler JM, Freiberg RA, Scott R. Extensive localized bone resorption in the femur following total hip replacement. J Bone Joint Surg [Am] 1976; 58-A: 61218. [ Links ]
33. Toms AP, Marshall TJ, Cahir J, Darrah C, Nolan J, Donell ST, Barker T, Tucker JK. MRI of early symptomatic metal-on-metal total hip arthroplasty: a retrospective review of radiological findings in 20 hips. Clin Radiol. 2008 Jan;63(1):49-58. [ Links ]
34. Milosev I, Trebse R, Kovac S, Cor A, Pisot V. Survivorship and retrieval analysis of Sikomet metal-on-metal total hip replacements at a mean of seven years. J Bone Joint Surg [Am]. 2006;88:1173-82. [ Links ]
35. Daniel J, Ziaee H, Kamali A, Pradhan C, Band T, McMinn DJW Ten-year results of a double-heat-treated metal-on-metal hip resurfacing. Journal of Bone and Joint Surgery -British Volume, Vol 92-B, Issue 1, 20-27. doi: 10.1302/0301 -620X.92B 1.21530. [ Links ]
36. Luetzner J, Krummenauer F, Lengel AM, Ziegler J, Witzleb WC. Serum metal ion exposure after total knee arthroplasty.Clin Orthop Relat Res. 2007 Aug;461:136-42. [ Links ]
37. Mont MA, Schmalzried TP. Modern metal-on-metal hip resurfacing: important observations from the first ten years. Journal of Bone and Joint Surgery - American Volume 2008;90:3-11. [ Links ]
38. Langton DJ, Sprowson AP, Joyce TJ, Reed M, Carluke I, Partington P, Nargol AV. Blood metal ion concentrations after hip resurfacing arthroplasty: a comparative study of articular surface replacement and Birmingham Hip Resurfacing arthroplasties. J Bone Joint Surg Br. 2009 Oct;91(10):1287-95. [ Links ]
39. Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS , MurrayDW. Pseudotumors associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008 Jul;90(7):847-51. [ Links ]
40. Doorn PF, Campbell PA, Worrall J, Benya PD, McKellop HA, Amstutz HC. Metal wear particle characterization from metalon metal total hip replacements: transmission electron microscopy study of periprosthetic tissues and isolated particles. J Biomed Mater Res. 1998 Oct;42(1):103-11. [ Links ]
41. McMinn D, Daniel J, Pradhan C, Ziaee H, Wingate J. 10-Year Results Of Modern Hip Resurfacing: Hip Function, Clinico-Radiological and Ct Scan Assessment, #P098 - American Academy of Orthopaedic Surgeons. Las Vegas 2009. [ Links ]
42. Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, Counsell I, Mclardy-Smith P, Beard DJ, Gill HS, Murray DW. Increased Wear Of Metal-On-Metal Hip Resurfacing Implants Revised Due To Pseudotumors. Presentation # 664 at the AAOS Annual Meeting. New Orleans 2010. [ Links ]
43. Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation. Four to seven-year results. J Bone Joint Surg [Am].2000;82:789-98. [ Links ]
44. Lazennec JY, Unexpected bad mid-term results with second generation (Metasul) metal-on-metal THP 12 years follow up. Proceedings of the 15th Triennial Congress of Asia Pacific Orthopaedic Association. September 2007, Seoul, Korea. [ Links ]
 Reprint requests:
Reprint requests:
Prof JG Myburgh
Department of Orthopaedics
Room 71306, Level 7, Bridge A
Steve Biko Academic Hospital University of Pretoria
Tel:+2712 354 2851
E-mail: hans.myburgh@up.ac.za














