Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.10 no.4 Centurion Jan. 2011
CASE REPORT AND REVIEW OF THE LITERATURE
Bilateral pneumothoraces and thyroid storm in undiagnosed Graves' disease following posterior fusion scoliosis surgery: a case report
Dr B MraraI; Prof M LukheleII
MBBCh, FCA(SA), Cert Crit Care (SA) Consultant Intensive Care Unit, Chris Hani Baragwanath Hospital, Faculty of Health Sciences, University of the Witwatersrand
MBChB, MMed(Orth), FCS(Orth)(SA) Head of Division of Orthopaedics, Faculty of Health Sciences, University of the Witwatersrand
ABSTRACT
The coexistence of idiopathic scoliosis and Graves' disease is not an established phenomenon. Bilateral pneumothoraces as a complication of posterior pedicle screw correction of scoliosis is an uncommon finding. Thyroid storm as initial presentation in Graves' disease is also uncommon. Surgery and stress are known precipitants of thyroid storm in untreated Graves' disease. We report on a 14-year-old female with idiopathic scoliosis who underwent posterior only pedicle screw correction of the deformity and developed bilateral pneumothoraces and thyroid storm in the first postoperative day. This was her first presentation with Graves' disease. Preoperatively she had reported no symptoms of hyperthyroidism. She was treated successfully and discharged from the hospital.
Key word: idiopathic scoliosis, undiagnosed Graves' disease, post-operation bilateral pneumothoraces, thyroid storm
Case presentation
A 14-year-old female presented with a rightsided mid-thoracic scoliosis. She was noted to have ligamentous hyperlaxity. There were no signs of Marfan syndrome or neurofibromatosis. After a careful search for other causes of scoliosis a diagnosis of idiopathic scoliosis was made. At the first presentation the Cobb angle was 42º and lateral side-bending flexibility 20º (Figure 1). At that stage she was managed conservatively with a thoracolumbar orthosis brace. The deformity progressed despite the brace; the Cobb angle had increased to 55º 2 years post initial presentation. The patient and family were then counselled for surgical correction. The pre-operative anaesthetic assessment was unremarkable except for a resting tachycardia of 120 beats per minute. The ECG showed this to be a sinus tachycardia. A cardiac assessment including an echocardiogram revealed a structurally normal heart. A careful search for possible causes revealed none; there were no symptoms or signs of hyperthyroidism. The tachycardia was thought to be due to anxiety and the decision was made to proceed with the surgery.

A standard general anaesthetic was given with propofol for induction, rocuronium for muscle relaxation, and fentanyl and remifentanil for analgesia. A size 6.0 endotracheal tube was used, a right side radial arterial line inserted and a right internal jugular central line placed without difficulty. She was positioned prone for the surgery.
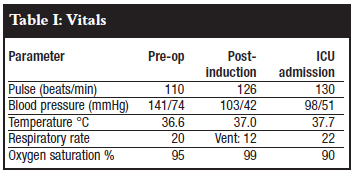
Vitals pre-operatively, intraoperatively and immediately post-operatively are shown in Table I.
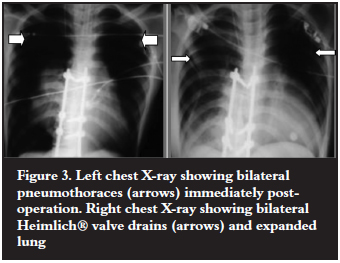
Posterior Ponte osteotomies and pedicle screw correction and stabilisation with two rods were performed. Intra-operatively the correct pedicle screw placement was confirmed by probing the prepared pedicle and image intensifier. No technical challenges or complications were encountered and good correction was achieved (Figure 2). The theatre time was 4 hours. The estimated blood loss was 500 ml, decreasing the haemoglobin from 14.8 to 9.5.The tachycardia subsided. Problems started in the last hour of surgery where endtidal carbon dioxide was noted to rise, along with peak and mean airway pressures. By the end of surgery the clinical picture was that of bilateral tension pneumothoraces with hypotension, low oxygen saturation and high endtidal carbon dioxide. An urgent chest X-ray confirmed the findings (Figure 3). Bilateral Heimlich® valve drains were promptly inserted after needle decompression and her respiratory parameters stabilised (Figure 3). Post operation a CT scan of the spine was done and the position of the pedicle screws in the thoracic spine was confirmed to be inside the pedicle at all the levels (Figure 4).

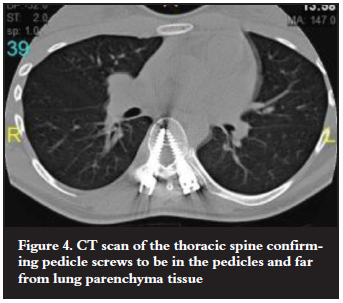
There was also no paraspinal soft tissue collection next to all the thoracic screws to suggest any deviation out of the pedicle during the pedicle screw preparation. There was no observed connection between the right and the left pleura.
She was extubated soon afterwards.
A few hours postop, in the ICU, she was noted to have a persistent tachycardia and fever despite adequate analgesia. The temperature had risen to 38.6 ºC and she was agitated. The agitation and persistent tachycardia in the presence of adequate analgesia triggered the physician to screen the patient for some form of metabolic crisis including hyperthyroidism.
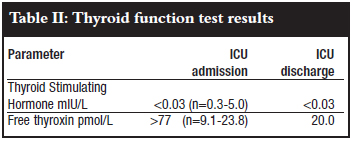
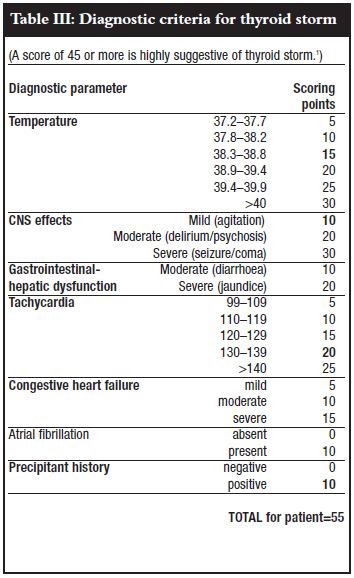
The thyroid function tests confirmed a hyperthyroid state (Table II). Based on the criteria of Burch and Wartofsky, a thyroid storm was diagnosed (Table III).1 She was treated with propranolol, hydrocortisone and carbimazole. AntiTSH receptor antibody results confirmed the diagnosis of Graves' disease.
She responded well to antithyroid treatment and was discharged to the ward after a week in intensive care. She was discharged from the hospital two days later and is continuing carbimazole treatment under the care of an endocrinologist.
Discussion
Graves' disease is a syndrome characterised by hyperthyroidism, goitre, orbitopathy and pretibial myxoedema. Hyperthyroidism is its most common feature.2 The pathogenesis involves the formation of auto antibodies to thyrotropin (TSH) receptors which bind and activate the receptor thereby stimulating thyroid hormone synthesis and thyroid gland growth. Graves' disease presents rarely in adolescence; it has an incidence only of 1 in 300 000 per population.3 A literature review did not find any association of Graves' disease and idiopathic scoliosis. Graves' disease is described in genetic disorders DiGeorge syndrome and Chromosome 22q deletion.4 They present with congenital cardiac lesions, mental retardation, cleft palate, spinal abnormalities and Graves' disease. Other Graves' disease associations are Down's syndrome, Turner syndrome and autoimmune conditions such as juvenile rheumatoid arthritis, Addison's disease, type I diabetes mellitus, myasthenia gravis and systemic lupus erythematosus.5 This patient had no associated pathology.
Thyrotoxicosis from Graves' disease is the most frequent cause of thyroid storm.6 Thyroid storm is a rare lifethreatening hypermetabolic state caused by severe thyrotoxicosis. Untreated thyroid storm has a mortality of up to 90%. It is thought to result from rapid rises in serum thyroid hormone levels, increased responsiveness to catecholamines and enhanced cellular responses to thyroid hormones. This can occur in untreated or partially treated patients who experience severe stress. Frequently described precipitants include surgery and anaesthesia (thyroid or nonthyroid), infection, trauma, parturition and acute iodine overload.
The diagnosis of thyroid storm is clinical; it involves quantifying the severity of thyrotoxic manifestations on thermoregulation, cardiovascular, central nervous and gastrointestinalhepatic systems. Burch and Wartofsky developed a scoring system grading the severity of thyrotoxic manifestations on these organ systems.1 They found a score of above 45 to be highly suggestive of thyroid storm. This score is widely used to differentiate thyroid storm from the milder thyrotoxicosis, because thyroid function tests results cannot differentiate between the two entities.7
The occurrence of thyroid storm as initial presentation in Graves' is commoner in children than adults. The true frequency is unknown. It is described in a few case reports.810 Aslan et al described it in previously undiagnosed Graves' in a prepubertal child with respiratory syncytial virus infection as a precipitant. Yuan et al described its occurrence in a patient with organophosphate poisoning who had a predominantly nicotinic clinical presentation with tachycardia and hypertension. In our patient the stress of surgery and bilateral pneumothoraces probably precipitated thyroid storm in untreated Graves' disease.
The normal heart rate for a child of 14 years is 60-100 beats per minute.11 A resting sinus tachycardia on the preoperative anaesthetic assessment is a frequent finding; it is most commonly caused by anxiety. Other important causes to look for are hyperthyroidism, fever, sepsis, volume depletion, cardiopulmonary pathology and exposure to stimulants. Rare causes include inappropriate sinus tachycardia and postural orthostatic tachycardia syndrome which affects young women.12 Abnormal autonomic control is thought to be the cause. For the anaesthesiologist the finding of a resting sinus tachycardia should prompt a thorough clinical assessment. The need for laboratory investigations is determined by the clinical findings. If abnormal symptomatology and clinical findings are elicited the anaesthesiologist should recommend 24-hour Holter monitoring.12 Hyperthyroidism should be kept in mind in patients with resting sinus tachycardia, and thyroid function tests should be taken even if no other obvious clinical findings of hyperthyroidism are found as is illustrated in this case report.
Posterior approach scoliosis correction with pedicle screw fixation is currently the gold standard in the management of progressive idiopathic scoliosis. It is considered to be safe.13 The complication rate is 11%, the commonest complication being screw malposition.14 Pulmonary complications are rare; one case report of a pneumothorax post thoracic pedicle screw placement was found.15 Hicks et al in a review of 21 studies with a total of 1 666 patients undergoing this type of surgery found one pleural effusion and one pneumothorax.14 The effusion had resulted from intrathoracic screw malposition; while the pneumothorax had occurred in a patient who had undergone thoracotomy. Suk et al reported one spontaneous pneumothorax in a series of 462 patients who underwent thoracic pedicle screw fixation.13
Our patient had internal jugular vein central venous line insertion after induction of anaesthesia. This has a risk of ipsilateral pneumothorax of 0.1-0.2 %.16 The development of bilateral pneumothoraces cannot be explained by this mechanism given that the central venous line was only inserted on one side and no attempts had been made on the opposite side. The postoperative CT scans showed no breaching of the pleura by the screws; thus the cause of the pneumothoraces was perhaps unrelated to the surgery. In the absence of an established cause the only explanation is that the patient developed primary spontaneous bilateral pneumothoraces. She has a thin body habitué, which fits the profile of patients at risk of this condition. Primary spontaneous pneumothoraces usually develop in tall thin people of ages 10-30 years. Smoking is an additional risk factor. The incidence is 18 cases per 100 000 population per year.17 The pathophysiology is loss of lung elastic fibres which results in subpleural bullae which then rupture and cause pneumothoraces. Ligamentous hyperlaxity such as occurs in Marfan syndrome and present in this patient is also a risk factor for lung elastic fibre loss. Findik et al described a case of bilateral pneumothorax following a unilateral transbronchial lung biopsy in the absence of previous thoracic surgery.18 Their patient had pulmonary lymphangioleiomyomatosis and the chest CT scan demonstrated a connection between the right and the left pleural spaces which could explain the bilateral pneumothorax complication. Our patient did not demonstrate any connections between the pleural spaces.
Conclusion
Bilateral pneumothoraces, though a rare complication of posterior approach scoliosis surgery, can occur. Practitioners should have a high index of suspicion for this complication in patients with risk factors for primary spontaneous pneumothorax. A chest X-ray should be done as soon as there is a detected change in ventilation pressure to avoid the development of life-threatening tension pneumothoraces. The finding of a resting tachycardia on the pre-operative assessment should prompt a search for an underlying cause including hyperthyroidism especially in patients undergoing major surgery.
References
1. Burch HB, Wartofsky L. Lifethreatening thyrotoxicosis. Thyroid storm Endocrinology and Metabolic Clinics of North America. 1993;22(2):263-77. [ Links ]
2. Davies TF, Ando T, Lin RY. Thyrotropin receptorassociated diseases: from adenomata to Graves' disease. Journal of Clinical Investigation. 2005;115:19-72. [ Links ]
3. Birrel G, Cheetam T. Juvenile thyrotoxicosis; can we do better? Archives of Disease in Childhood. 2004;89(8):745-50. [ Links ]
4. Seroogy C. DiGeorge Syndrome: Evaluation, diagnosis, and management 2011 [updated 28/01/2011; cited 2011 26/09/2011]; Uptodate] [ Links ].
5. SaiChing JY. Graves' Disease. 2011 [updated 2/6/2011; cited 2011 26/09/2011]; Medscape] [ Links ].
6. Ross D. Thyroid Storm. [Internet] 2011 [updated 27/05/2011; cited 2011 12/07/2011]; Uptodate] [ Links ].
7. Brooks MH, Waldstein SS. Free thyroxine concentrations in thyroid storm. Annals of Internal Medicine. 1980;93:694. Epub S. [ Links ]
8. Aslan IR, Baca EA, Charlton RW, Rosenthal SM. Case report. Respiratory syncytial virus infection as a precipitant of thyroid storm in a previously undiagnosed case of Graves' Disease in a prepubertal girl. International Journal of Pediatric Endocrinology. 2011;2011:1-3. [ Links ]
9. Yuan Y, Lin C, Lin L. Case Report: Thyroid storm precipitated by organophosphate intoxication. American Journal of Emergency Medicine. 2007;25:861 e 1- e 3. [ Links ]
10. Izumi K, Kondo S, Okada T. A case of atypical thyroid storm with hypglycemia and lactic acidosis. Endocrine Journal. 2009;56(6):747-52. [ Links ]
11. Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, et al . Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet. 2011;337(9770):1011-18. [ Links ]
12. DeVoe J, Judkins D. What is the best approach to the evaluation of resting tachycardia for an adult? Journal of Family Practice. 2007;56(1):59-61. [ Links ]
13. Suk S, Kim W, Lee S, Kim J, Chung E. Thoracic pedicle screw fixation in spinal deformities. Spine. 2001;26(18):2049-57. [ Links ]
14. Hicks J, Singla A, Shen F, Arlet V. Complications of pedicle screw fixation in scoliosis surgery. Spine. 2010;35(11):E 465-E 70. [ Links ]
15. Viswanathan A, Relyea K, Whitehead MSWE, Curry D, Luerssen T, Jea A. Pneumothorax complicating 'inoutin' thoracic pedicle screw placement for kyphotic deformity correction in a child. Journal of Neurosurgical Pediatrics. 2008;2:379. [ Links ]
16. Graham A, Ozment C, Tegtmeyer K, Lai S, Braner D. Central venous catheterisation. New England Journal of Medicine. 2007;356:e 21. [ Links ]
17. Sahn SA, Heffner JE. Spontaneous pneumothorax. New England Journal of Medicine. 2000;342:868-74. [ Links ]
18. Findik S, Erkan L, Light RW. Iatrogenic bilateral pneumothorax following unilateral transbronchial lung biopsy. British Journal of Radiology. 2006;79:e22-e24. [ Links ]
 Reprint requests:
Reprint requests:
Prof M Lukhele
Division of Orthopaedics
Room 4M12, Wits Medical School 7 York Road Parktown
Email: mkhululi.lukhele@wits.ac.za
Disclosure" None of the authors received any benefits in the preparation of this case report.














