Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Orthopaedic Journal
versão On-line ISSN 2309-8309
versão impressa ISSN 1681-150X
SA orthop. j. vol.10 no.4 Centurion Jan. 2011
CLINICAL ARTICLE
Canterbury index: an accurate predictor of fracture redisplacement?
Dr H BassonI; Dr SS VermaakII; Dr HF VisserIII; Prof P RheederIV
IMBChB(Pret) Senior Registrar, Department of Orthopaedic Surgery, Steve Biko Academic Hospital, University of Pretoria
IIMBChB(Pret), MSc(Sports Med)(Pret) Senior Registrar, Department of Orthopaedic Surgery, Steve Biko Academic Hospital, University of Pretoria
IIIMBChB(Pret), MMed(Orth)(Pret) Orthopaedic Surgeon Life Eugene Marais Hospital
IVMMed(Int Med)(Pret), MSc(Clin Epi)(Rotterdam), PhD(Utrecht) Division of Clinical Epidemiology School of Health Systems and Public Health, University of Pretoria
ABSTRACT
PURPOSE: Paediatric forearm fractures are commonly seen and treated by closed reduction and plaster cast application in theatre. Historically cast application has been subjectively evaluated for its adequacy in maintaining fracture reduction. More recently emphasis has been placed on objectively evaluating the adequacy of cast application using indicators such as the Canterbury index (CI). The CI has been used in predicting post-reduction, re-displacement risk of patients by expressing the cast and padding indexes as a ratio. The CI has been criticised for not including cast three-point pressure, fracture personality, lack of standardisation of X-ray views as well as practical requirement of physical measurement using rulers.
The aim of this study was to determine whether subjective evaluation of these indices, before and after a tutorial on the CI, was accurate in predicting a patient's ultimate risk of re-displacement, following reduction and casting.
In addition, we aimed to determine whether objective evaluation of these indices by measurement on the hospital's digital X-ray system correlated with the final fracture outcome post-reduction.
MATERIALS AND METHODS: A retrospective study was done on a sample of 11 patients during the period May 2010 to July 2011 at Steve Biko Academic Hospital. In total, 44 X-rays/fluoroscopy views were subjectively evaluated by 20 registrars and eight consultants for possible fracture re-displacement, before and after a tutorial on the CI. Five consultants and 10 registrars each measured 22 cast, padding and CIs on the digital X-ray system.
RESULTS:A formal tutorial did not produce an increase in subjective predictive accuracy. Pre- and post-tutorial observed agreement was seldom better than agreement by chance alone. Poor strength of agreement (κ <0.20) was found in all groups, irrespective of level of displacement, imaging modality, level of orthopaedic training and tutorial attendance. Objective measurement of the indexes all had insignificant p-values for comparing groups, indicating that there was no correlation between the measured indexes and the final outcome irrespective of the level of fracture, imaging modality and level of orthopaedic training. Shortcomings were variable co-operation from participants and non-standardisation of X-rays.
CONCLUSION: In our hospital setting, no clinical value for the subjective and/or objective use of the CI could be found. Subjective agreement was almost the same as expected agreement and objective measurement indicated no correlation with the fracture outcome. It is suggested that patients following closed reduction of forearm fractures be followed up within the first three days, and regularly thereafter, as there is currently no ideal system to predict re-displacement.
Further studies are needed to validate the CI by standardisation of X-rays.
Key words: paediatric, closed forearm fractures, Canterbury index, cast index, padding index
Introduction
Forearm fractures are the most common fractures in the paediatric population,13 while distal radial fractures account for most of these.2,4 Historically closed manipulation, with anatomical reduction and plaster of Paris (POP) moulded casting has yielded good results in the management of these fractures.2 This still remains the preferred treatment in current orthopaedic practice.2,5
The Canterbury index (CI)3,6 is one of the indexes described for evaluating the adequacy of postmanipulation casting. It is a sum of the cast index, first described by Chess and co-workers in 1994, and the padding index. The cast index3,6,7is defined as the measurement of the internal cast width in the lateral view and the internal cast width in the anteroposterior (AP) view at the fracture site, expressed as a ratio (Figure 1a). As the cast becomes more circular, the lateral diameter approaches that of the AP diameter and the cast index would approach the value of 1. The padding index6 is the ratio of the padding thickness under the moulded cast in lateral view, in the plane of deformity correction, to the maximum interosseous distance in the AP view (Figure 1b). The padding index is said to be an indirect measure of the three-point fixation, where the greater the padding thickness at the fracture site the poorer the three-point fixation.6
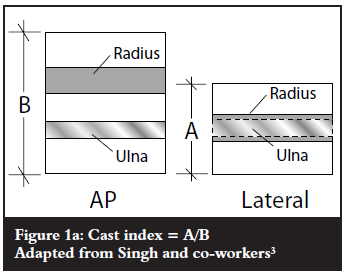
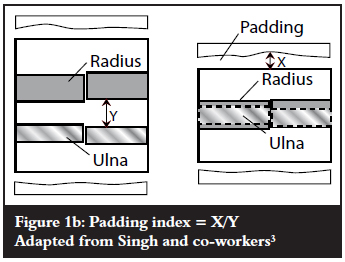
Following cast application, a cast index exceeding 0.8, a padding index exceeding 0.3, and/or the combined CI of more than 1.1 should be closely followed up, as it is prone to re-displacement.3,6
With this study we aimed to determine the accuracy of predicting fracture re-displacement by subjective evaluation of the cast adequacy post reduction, pre- and post a tutorial on the usage of the CI. In addition, we aimed to determine the accuracy of objective evaluation of the cast adequacy post reduction by measuring the CI on the hospital's digital X-ray system and correlating it with the final fracture displacement.
Materials and methods
A retrospective study was done on all patients admitted to Steve Biko Academic Hospital (SBAH), for closed reduction of forearm fractures during the period May 2010 to July 2011. Excluding Salter Harris fractures and fractures that received fixation, 34 closed distal radius with or without ulna fractures from 33 patients, and 18 closed radius and ulna shaft fractures from 17 patients, were identified. Inclusion criteria included patients with an open growth plate, adequate fluoroscopy in theatre post reduction, adequate follow-up X-rays on days 1–7 post-operatively and an X-ray at 3–6 weeks to evaluate for displacement. Exclusion criteria included Salter Harris fractures, open fractures, fractures that were unstable in theatre and required K-wire fixation, as well as those patients who had inadequate X-rays or follow-up.
Based on the criteria, a sample of 11 patients was chosen for the study, six of whom sustained distal radius with or without ulna fractures, and five radius and ulna shaft fractures. Of these patients, two distal radius fractures had clinically significant displacement (>20º angulation and >50% translation as described by Singh1,3,8); three had clinically insignificant displacement (of which two were distal radius fractures and one a shaft fracture); and six had no displacement at final follow-up (Figure 2). No clinically significant displaced shaft fractures from the reviewed period were available to use in the study. The age ranged from 4–14 years (average 7.7 years).
In total, eight consultants and 20 registrars evaluated 44 fluoroscopy views/X-rays. This added up to a total of 1 232 evaluations as compared to the 200 from Singh.3 Displacement risk was recorded for each subject on each fluoroscopy view/X-ray as likely or unlikely. This was followed by an information session on performing the CI. Thereafter, participants re-evaluated all the fluoroscopy views/X-rays, and again rated displacement risk for each case as likely or unlikely (Figure 3). The performances of the subjects were compared to the clinical outcome of the patients.
In the second part of the study five consultants and ten registrars were asked to measure the cast index, padding index and ultimately the CI on the digital X-ray system available at SBAH (Figure 4). A total of 330 CIs were measured. These results were correlated to the three final outcome groups for fracture displacement previously described (Figure 2).
Data analysis
Agreement between observers and actual outcome was measured with the Kappa statistic (which measures agreement beyond that which can be expected by chance). Angles between groups were compared with Mann-Whitney and Kruskal Wallis tests. The p-value for trend was computed from the Spearman test. P-value of <0.05 was deemed statistically significant.9
Results
The pre- and posttutorial agreement (observed, expected and Kappa) are given separately for registrars and consultants, on fluoroscopy, X-ray and combined images (Tables I and II).
Observed agreement: results of subjective evaluation, obtained in the study.
Expected agreement: results that are expected if left to chance.
Pre-tutorial observed agreement was seldom better than agreement by chance alone (expected agreement) (Tables I and II), implying that to flip a coin would almost give the same results as subjectively trying to evaluate a postoperative X-ray for possible re-displacement. The best Kappa (Table III) was 0.257 which is at best fair (for the consultants evaluating any displacement on fluoroscopy), but all the other pre-tutorial Kappa values indicated poor strength of agreement.
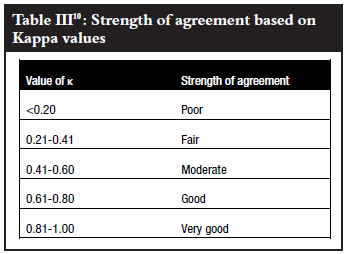
Post-tutorial agreement was worse as compared to pretutorial data, with all the Kappa values indicating poor agreement and having lower values. The only exceptions were the consultants' prediction for major displacement using X-rays and combined imaging, as well as all the participants' X-ray evaluation for any displacement, where the Kappa values did not increase significantly.
Despite this, the values were still poor. The strength of agreement was less for major displacement than for any displacement, with the accuracy of the registrars being below the expected agreement post tutorial. This poor strength of agreement (Kappa value <0.20) was found in all groups, irrespective of level of displacement, imaging modality, level of orthopaedic training and tutorial attendance.
Due to the fact that no shaft fractures had clinically significant displacement at follow-up, the trends could not be calculated and there are no indexes available (Tables IV and V).
For the registrars' X-ray measurements of the distal radius, significant p-values are observed (p <0.05) for the padding and CIs. However, even though the p-trend is also significant (0.012 and 0.024 respectively), it is in the wrong direction, indicating that the indexes decrease as the displacement increases, thus rendering it clinically insignificant. The p-values of the padding and CIs for the registrars' combined fracture X-ray measurements are also significant (p <0.05), but irrelevant due to the fact that the trends are insignificant (0.313 and 0.177 respectively).
The registrars' measurements of the padding index on fluoroscopy views for shaft fractures was significant (p-value = 0.021) indicating a significant decrease in the padding measurement between the undisplaced and insignificantly displaced fractures, as expected. Unfortunately no trend is available, due to the fact that there were no significantly displaced shaft fractures available to include in the study. This measurement taken by the consultants had an insignificant p-value as well as the CIs of both the consultants and registrars for the evaluation of shaft fractures on fluoroscopy. This makes it difficult to interpret the relevance of this p-value, and clinically it appears to be insignificant if looking at the greater picture.
Taking everything into consideration, the cast, padding and CIs all had insignificant p-values for comparing groups, indicating that there was no correlation between the measured indexes and the final outcome irrespective of the level of fracture, imaging modality, level of orthopaedic training and qualification.
Discussion
A well-known complication of paediatric forearm fractures is re-displacement following initial manipulation and casting2,6 with rates as high as 12%-34% cited.2,6,11Various factors have been implicated as possibly contributing to re-displacement and they can be divided into three main groups:2
1. Fracture-related factors (degree of initial displacement, location and geometry of the fracture, isolated distal radius fracture and associated ulna fracture on the same level)12,13
2. Patient-related (muscle atrophy and resolution of the initial swelling while in the cast)2
3. Surgeon-related (ability to reduce the fracture anatomically, and to maintain that reduction with a well-moulded cast)11,12
Of these factors, initial translation of fracture on pre-manipulation X-rays, and failure to achieve anatomical reduction is associated with a high re-displacement rate.11,12 While a poorly applied cast, with subsequent loss of reduction in the cast is said to be the most important causative factor by other authors,6,14 the importance of a well-moulded cast has been emphasised as early as 1968 by Charnley3 and has been reiterated in more recent literature.7 Other authors concluded that a well-moulded below-elbow cast is as effective as an above-elbow cast in the management of distal third forearm fractures in children.4,14
In an attempt to minimise the complication of re-displacement, various indices have been described to look at the adequacy of the post-manipulation casting, thereby predicting whether the fracture will re-displace based on the particular index used. These indices serve as a method for objectively assessing cast adequacy2,3,6 and include:
• the cast index described by Chess and co-workers3,4,6,7
• the Canterbury index (i.e. the sum of the cast index and the padding index)3,6
• the gap index2
• the three-point index2
• the second metacarpal-radius angle2
In the original article by Singh, Bhatia and Housden,3 a 50% reduction in re-displacement rate of paediatric fractures was achieved by adhering to the CI in the teaching of cast application. 2 They also showed that there was good inter-observer and intra-observer reproducibility for the cast and padding indices. In a later study Singh validated the use of the CI, and concluded that it was a safe, reliable and reproducible measure in predicting re-displacement of forearm fractures in children.3 Prior to the use of indexes cast application has been subjectively scrutinised ('eyeballed') to evaluate its adequacy in maintaining fracture reduction. Singh, Bhatia and Housden showed that the accuracy in predicting fracture re-displacement by simply 'eyeballing' the cast was 33% for their consultant group, while only marginally less at 28% in the registrars tested. Both groups showed a statistically significant improvement after applying the CI.3
This study however indicated that the strength of agreement during subjective evaluation was poor and seldom better than the expected agreement, irrespective of the level of displacement, imaging modality and level of orthopaedic qualification. Results in general worsened after the tutorial on the CI. This might be due to the fact that the participants excluded other factors usually taken clinically into account, e.g. fracture pattern.
There was also no correlation between the measured indexes and the final fracture outcome, irrespective of the level of the fracture, the imaging modality and the level of orthopaedic qualification, with almost all the p-values being insignificant.
The shortcomings of this study are the fact that our digital X-ray system does not have standardisation of the Xrays, and this is paramount in validating the CI as an accurate predictor of fracture re-displacement. However, the aim of our subjective part of the study did not require it, due to the fact that we aimed for a real-life, current setting study.
The second shortcoming was the variability of co-operation from the participants.
Conclusion
In our hospital setting, no clinical value for the subjective and/or objective use of the CI could be found. Subjective agreement was almost the same as expected agreement and objective measurement indicated no correlation with the fracture outcome.
Use of the CI in clinical practice is doubtful due to various confounding factors. It has been used due to lack of other available systems, and ideally a system should be sought which incorporates fracture personality, cast threepoint pressure,15-17 standardisation of X-rays, anatomical reduction immediately post-operatively4 and initial displacement. 11,12
It is suggested that patients following closed reduction of forearm fractures be followed up within the first three days and regularly thereafter, as there is currently no ideal system to predict re-displacement. Further studies are needed to objectively validate the CI by standardisation of X-rays.
References
1. Haddad F, Williams R. Forearm fractures in children: avoiding redisplacement. Injury 1995;26(10):691-92. [ Links ]
2. Mazzini J, Martin J. Paediatric forearm and distal radius fractures: risk factors and re-displacement - role of casting indices. International Orthopaedics 2010;34:407-12. [ Links ]
3. Singh S, Bhatia M, Housden P. Cast and padding indices used for clinical decision making in forearm fractures in children. Acta Orthopaedica 2008;79(3):386-89. [ Links ]
4. Webb G, Galpin R, Armstrong D. Comparison of short and long plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Joint Surg (Am) 2006;88- A:9-17. [ Links ]
5. Hove L, Brudvik C. Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg 2008;128:55-60. [ Links ]
6. Bhatia M, Housden P. Redisplacement of paediatric forearm fractures: Role of plaster moulding and padding. Injury Int J Care Injured 2006;37:259-68. [ Links ]
7. Chess D, Hyndman J, Leahey J. Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop 1994;14:211-13. [ Links ]
8. Procter MT, Moore DJ, Paterson JMH. Redisplacement after manipulation of distal radial fractures in children. J Bone Joint Surg (Br) 1993;75:453-54. [ Links ]
9. Ihaka R, Gentleman R. A Language for Data Analysis and Graphics. Journal of Computational and Graphical Statistics 1996;5(3):299-314. [ Links ]
10. Monga P, Raghupathy A, Courtman N. Factors affecting remanipulation in paediatric forearm fractures. J Pediatr Orthop 2010;19-B:181-87. [ Links ]
11. Alemdaroglu K, Iltar S, Cimen O, Uysal M, Alagoz E, Aththan D. Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg (Am) 2008;90- A:1224-30. [ Links ]
12. Bae D. Pediatric distal radius and forearm fractures. J Hand Surg 2008;33-A:1911-23. [ Links ]
13. Younger A, Tredwell S, Mackenzie W. Factors affecting fracture position at cast removal after pediatric forearm fracture. J Pediatr Orthop 1997;17:332-36. [ Links ]
14. Altman DG. Practical statistics for medical research. London: Chapman and Hall. 1991. [ Links ]
15. Charnley J. The closed treatment of common fractures. Williams and Wilkins, Baltimore. 1968. [ Links ]
16. Dicke TE, Nunley JA. Forearm fractures in children. Complications and surgical indications. Orthop Clin North Am 1993;24:333. [ Links ]
17. Voto SJ, Weiner DS, Dennis S. Redisplacement after closed reduction of forearm fractures in children. Journal Pediatric Orthop 1990;10:79-84. [ Links ]
 Reprint requests:
Reprint requests:
Dr HF Visser
Email: docfish@mweb.co.za
Cell: +27(82)3333772
No benefits of any form have been received from a commercial party related directly or indirectly to the subject of this article. The content of this article is the sole work of the authors.














