Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.10 n.3 Centurion Jan. 2011
CLINICAL ARTICLE
Anterior-only transthoracic surgery for adult spinal tuberculosis
Bryan RiemerI; Robert DunnII
IDr. MBChB(UCT). Registrar, Department of Orthopaedic Surgery, University of Cape Town
IIProf. MBChB(UCT), FCS(SA)Orth, MMed(Orth). Associate Professor and Head of Spinal Services: Groote Schuur Hospital, Division of Orthopaedic Surgery, University of Cape Town, South Africa
ABSTRACT
Historically, anterior decompression followed by posterior fusion has been the surgical management of choice in spinal tuberculosis. Due to theatre time being at a premium, we have evolved to anterior only debridement, allograft strut reconstruction and instrumentation for tuberculosis in the adult thoracic spine.
The aim of this study was to review the safety and efficacy of this treatment.
METHODS: Twentynine adult thoracic tuberculosis patients were identified where anterior-only surgery had been performed. These were all midthoracic TB as circumferential surgery is still favoured in thoraco-lumbar disease. The surgery was performed by a single surgeon at a tertiary hospital.
A retrospective review of clinical notes and radiological studies was performed.
RESULTS: The average surgical time was 2 hours 15 minutes with a median blood loss of 700 ml. The majority of patients had two vertebral bodies involved and required an average of a four-body fusion.
Twenty-eight of the patients presented with altered neurology; three only had sensory changes while 25 presented with paraparesis and an inability to ambulate. Twentythree patients recovered to independent mobility at their latest follow-up appointment.
There was an average preoperative kyphosis angle of 33º, which improved immediately post-operatively to 22º, (p = 0.03). The average deformity at latest follow-up was 32º (p = 0.003).
Sixteen of 28 patients had documented bony fusion with no evidence of instrumentation failure or loosening in any patients.
There were two deaths related to the patients' general poor state of health and co-morbidities.
CONCLUSION: Transthoracic anterior-only debridement, allograft strut graft and simple body fixation provides an effective option for the management of adult thoracic tuberculosis.
There is a high success rate in achieving return to ambulatory status with few complications. Although loss of early sagittal correction is seen with time, this does not affect neurological outcome. Intra-operative attention to maintaining end-plate integrity is encouraged in an effort to reduce graft subsidence.
Key words: Spine, tuberculosis, anterior, surgery, adult
Tuberculosis (TB) continues to be the leading worldwide cause of death from infectious disease, and is causing increasingly widespread concern.1 TB is endemic in South Africa, with a reported incidence of 718 in 100 000 persons. In isolated pockets of the Western Cape, there is currently an epidemic of TB, with an incidence of 1 200 in 100 000 persons.2 Involvement of the skeletal system is relatively rare; for every 300 cases of pulmonary TB, one case of skeletal TB is seen.3
There has been a global increase in TB, which can be attributed to poverty, insufficient and inadequate healthcare resources and the impact of the human immunodeficiency virus (HIV) epidemic. Onethird of the increased incidence of TB can be directly attributed to HIV.4 HIV results in a far greater incidence of skeletal TB; Moon found that in HIV-negative patients between 3% and 5% will have skeletal involvement while up to 60% of HIV-positive patients will have skeletal involvement.5
Spinal TB is potentially the most dangerous form of skeletal TB by virtue of its capacity to cause bone destruction, deformity, and paraplegia. Surgery has been advocated in the presence of spinal deformity, significant neurological dysfunction, failure of medical management and persistent severe pain.6
The mainstay of treatment for tuberculous infection is medical chemotherapy as shown by the MRC trials.7 However antituberculous drugs cannot address the resultant bone destruction, such as pre-existing and/or residual deformity, paraplegia or pulmonary insufficiency due to spinal deformity. Restoration of spinal stability is crucial in the management of spinal TB in selected cases.8
There is a large volume of literature examining the optimal surgical management of TB of the spine. Most recent publications advocate anterior decompression followed by posterior stabilisation either in the same setting or within a 2-week period.9 Anterior thoracic spine lesions may be resected via a transthoracic approach. This method allows direct visualisation of the anterior thoracic spine for optimal lesion resection and the placement of anterior grafts and instrumentation.
Tuberculous inflammation of the spine is usually located ventrally; an anterior approach offers the most direct access to the disease process. This approach also enables minimal removal of normal bone, rapid removal of inflammatory and necrotic components and effective reconstruction of the weight-bearing anterior column. Strong torsional and axial stability, shortsegment fixation, prevention of posterior paraspinal musculature injury, and improved wound healing are also facilitated.10 It also avoids the need for a second procedure, thus decreasing the theatre time required. Although the combined anterior and posterior approach has been well-documented, it is associated with greater blood loss, more post-operative complications and a longer hospital stay.11
Aims and objectives
Our aim was to study the safety and efficacy of a one-stage, anterior-only debridement, inter-body allograft and instrumented fusion for the management of tuberculous disease of the thoracic spine in the adult population.
Methodology
A retrospective review of case notes and radiographs of 29 consecutively managed adult patients with TB of the thoracic spine was performed after Institutional Human Research Ethics Committee approval was obtained.
These were identified from a prospectively maintained database. All patients underwent anterior-only surgery, which involved anterior decompression and a structural graft fusion. All surgery was performed by the senior author (RD) between 2002 and 2010.
Patient demographics, age at surgery, initial presentation, initial investigations including HIV status, surgical management, blood loss, surgical time, graft and implant used, complications, in addition to pre- and post-operative neurological Frankel grading were recorded.12 Plain radiological findings were reviewed at three time points: pre-operatively, immediately post-operatively and at the latest outpatient follow-up visit.
Diagnosis of TB was suspected on history, clinical examination and special investigations (blood results, plain radiographs and MRI scan). The diagnosis was confirmed at surgery with resected specimens sent for histology, microscopy and culture.
Histology results were deemed positive if acid fast bacilli (AFB), caseous necrosis or granulomatous inflammation with necrosis were present. Granulomatous inflammation without necrosis was interpreted as suggestive. TB was confirmed in 25 of 29 patients. A further two patients had results suggestive of TB, i.e. granuloma but no caseation. The remaining two patients did not have histopathological or microbiological evidence of TB. Laboratory records for one patient could not be located and the other had received TB treatment 6 months prior to surgery. Figure 1 demonstrates the diagnostic results.

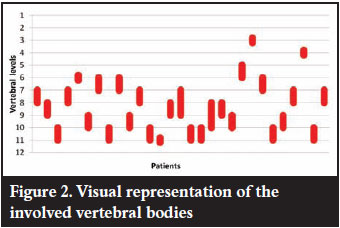
Figure 2 is a visual representation of the involved vertebral bodies in our series. It is evident that the majority of disease was in the lower thoracic spine (T6T11), the most prevalent site of TB spondylitis in the literature. The average number of vertebral bodies involved was two. There were no patients with involvement of T12 included in the series as posterior instrumentation is utilised for lesions involving the thoraco-lumbar junction due to the increased stress.
All patients underwent a transthoracic decompression and anterior instrumented fusion.13 A single lumen endotracheal tube with lung packing was typically used to avoid the prolonged anaesthetic preparation time associated with double lumen tubes. A left-sided thoracotomy was used for the majority of cases with the identified rib excised, generally two levels above the target vertebrae. Once the spine was exposed, the abscess was delineated and a plane developed between the anterior longitudinal ligament and the aorta. A copper malleable retractor was placed in this plane to retract and protect the great vessels. Discectomies were performed at the levels adjacent to the destroyed levels. The diseased spine was resected and the thecal sac exposed to ensure adequate decompression of the neural elements. The allograft was cut to size and placed between the healthy end plates with distraction to facilitate placement. Body screws and a single rod were placed to prevent graft displacement (Figures 3 and 4). The chest was closed in layers over an intercostal drain.


All patients were started on Rifafour (a combination tablet containing rifampicin, isoniazid, pyrazinamide and ethambutol) after surgery if not already receiving treatment. The full-dose, four-drug combination therapy was continued for a minimum of 9 months. The decision to terminate treatment was based on the patients' clinical response to treatment, their radiological findings and ESR. Patients were reviewed on a 3-monthly basis with repeat plain radiology and ESR.
Results
Of the 29 patients, 22 were female and seven were male. The mean age at time of surgery was 46 (16 - 74 ± 16.0) years. The mean white cell count (WCC) was 8.00 (3.9 - 12.9 ± 3.3) and erythrocyte sedimentation rate (ESR) was 87 (10 - 136 ± 41.6).
Of the 29 patients, 21 were tested for HIV; eight of the 21 were HIV positive (38%).
The average surgical time was 135 (90 - 197 ± 30.7) minutes and the median blood loss was 700 ml (300 - 2000 ± 474.5).
A bone bank humeral allograft was used as a strut graft in 22 of the 29 cases and this is the graft of choice. Six had a fibula allograft. In a single case a metal cage was used as this patient presented with a vertebra plana and was initially thought to have a malignancy. Final histology and microbiology revealed the diagnosis of TB.
Drug sensitivity testing was performed in 13 TB culturepositive cases, of which a single patient was found to have multi-drug resistant TB (MDR-TB).
At presentation, 25 of 29 patients were nonambulant (Frankel grading A, B or C). Of the four ambulant patients (Frankel grading D or E), three had altered sensation and one had no neurological deficit.
In a single case there was some deterioration in neurological function post-operatively, however there was rapid recovery to the preoperative neurological level within a few days. At later follow-up this patient had full recovery to normal neurology (a Frankel grade E).
At the most recent post-operative follow-up, 23 of 29 patients were ambulant with or without walking aids. Of the six nonambulant patients, two were early post-operative deaths, two were lost to follow-up after discharge and two were in an early post-operative stage. These patients in the early post-operative period have shown some neurological improvement, but not to that of a sufficiently useful motor level as yet. These results are shown in Figure 5.

Lateral spine plain films were analysed and the kyphosis angle measured pre-operatively, immediately post-operatively and at the latest follow-up visit.
There was an average preoperative kyphosis angle of 33º, which improved immediately post-operatively to 22º, (p = 0.03). The average deformity at latest follow-up was 32º (p = 0.003).
In 16 of 29 patients evidence of bony fusion was documented based on clinical and radiological findings (Figure 6). No cases of instrument failure, loosening of implants or graft dislodgement occurred.

There were two early post-operative deaths. Both patients were elderly with multiple comorbid conditions. The first patient was admitted to the intensive care unit (ICU) post-operatively, suffered multi-organ failure and died after a protracted course. The second patient experienced respiratory difficulty post-operatively; discussion deemed the patient not to be an intensive care unit candidate and the patient later died from respiratory failure.
In one case the diaphragm was inadvertently opened during the exposure due to the presence of extensive adhesions. The defect was repaired and the patient was not observed to suffer any further morbidity as a result.
Discussion
The surgical technique of choice for spinal TB has been subject to continual debate throughout the history of spinal surgery.14 Hibbs15 and Albee16 introduced posterior fusion for TB of the spine in 1911; Ito et al17 followed in 1934 with the introduction of anterior surgery. Both these procedures had a high failure rate due to the lack of adequate chemotherapy. In 1956, Hodgson and Stock18 first described a radical anterior decompression and bone grafting of the defect under the cover of chemotherapy, with good results. Anterior radical surgery (the Hong Kong operation) was then advocated as the treatment of choice for spinal TB until the mid 1970s.
The major advantage of anterior radical surgery was essentially deformity correction and to a certain extent prevention of deformity progression. However due to graft failure, the procedure was not always successful in preventing kyphosis progression or in correcting the underlying deformity.
This shortcoming resulted in many surgeons looking to improve on this procedure. Moon in 1975 first studied inter-spinous wiring and fusion or cementation to help prevent deformity progression followed by an evaluation of a passive posterior compression rodhook system in children in 1978.19 The combined twostage operation of posterior instrumentation and anterior radical surgery was introduced by Moon et al in 1983 with a good outcome.20 Rajasekaran and Shanmugasundaram proposed that patients requiring removal of more than two disc spaces may benefit from extra measures, such as extended periods of non-weight-bearing, posterior arthrodesis and prolonged brace use.21
In 1990 Louw proposed the Kalafong procedure which involved an anterior radical debridement followed by a posterior instrumented fusion, either in the same setting or in a second theatre setting within a 2-week period.22 Govender and Parbhoo have since used fresh frozen humeral allograft anteriorly with onlay posterior fusion in children with TB spondylitis and showed good results.23
TB of the spine is a common problem encountered in the Western Cape of South Africa. In Cape Town we have treated 29 adult patients with TB of the thoracic spine with an anterior-only surgical approach via a thoracotomy, anterior decompression and instrumented fusion with a structural allograft. The surgery has a low complication rate, allows for adequate decompression of the neural elements and a stable reconstruction. The surgery can be performed in a single episode, does not require repositioning or a second surgical intervention. The paraspinal musculature is neither breached nor damaged. Wound healing has not been a concern; the anterior thoracotomy wound generally heals well as it is far from the pathology and is not vulnerable to pressure in the same manner as a posterior midline wound would be. An anterior-only approach also avoids the danger of prominent hardware as may be found with posterior instrumentation.
Although there is an initial correction of the kyphotic deformity there is a trend for the deformity to recur. This deformity returns to the preoperative level of angulation over time but this does not seem to have a negative effect on neurological outcome. The deformity is in the thoracic spine, which has a natural kyphosis. The rib cage supports the spine in the thoracic region, augmenting the stability of the spine and preventing further progression.
In the management of fractures of the spine, Verlaan found that most operative treatment techniques will fail to maintain the operatively achieved alignment to some degree and will drift into kyphosis of approximately 10º greater than that achieved at the time of surgery.24 The correction lost using short segment fixation for fractures was reported as 7.6º. This is similar to our findings.
This loss of deformity correction is likely to be due to slow and gradual subsidence of the graft into the vertebral body end-plates which may be softened by the disease process or recumbancy. This subsidence may be exacerbated by end-plate violation during decompression or graft insertion and great care needs to be taken when performing the debridement to maintain the end-plate integrity.
Failure of structural allografts is usually due to infection or fracture.25 We have not observed fractures or additional bacterial infection in our series. This may be due to the fact that metal is harmless in a TB lesion as shown by both Oga, Ha and colleagues; TB is usually present in planktonic form, has very slow division, does not produce an adhesion molecule or biofilm and has a low organism population in bone.26,27
Conclusion
Transthoracic anterior-only debridement, allograft strut graft and simple body fixation provide an effective option for the management of adult thoracic TB.
There is a high success rate in achieving return to ambulatory status with few complications. Although loss of early sagittal correction is seen with time, this does not affect neurological outcome. Intra-operative attention to maintaining end-plate integrity is encouraged in an effort to reduce graft subsidence.
References
1. Mankin HJ. Tuberculosis of bone and joints: the Red King lives. Curr Opin Orthop 2001;12:489-98. [ Links ]
2. Donald, PR. The epidemiology of tuberculosis in South Africa. In: Novartis Foundation Symposium. Genetics and tuberculosis. Chichester: John Wiley; 1998:24-41. [ Links ]
3. Strebel PM, Seager JR. Epidemiology of tuberculosis in South Africa. In: Coovadia HM, Benatar SR (eds). A century of tuberculosis: South African perspectives. Cape Town: Oxford University Press;1991:58-90. [ Links ]
4. Centers for Disease Control: Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Morb Mortal Wkly Rep. 1992;41:1-19. [ Links ]
5. Moon MS. Tuberculosis of the spine: Controversies and a new challenge. Spine 1997;22:1791-97. [ Links ]
6. Medical Research Council Working Party on Tuberculosis of the Spine: A 10-year assessment of controlled trial comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong Kong. J Bone Joint Surg Br 1982;64:393-98. [ Links ]
7. Medical Research Council Working Party on tuberculosis of the spine fiveyear assessment of controlled trials of shortcourse chemotherapy regimens of 6, 9 or 18 months' duration for spinal tuberculosis in patients ambulatory from the start or undergoing radical surgery. International Orthopaedics 1999;23(2):73-81. [ Links ]
8. Dadi Jin, Dongbin Qu, Jianting Chen, Hao Zhang. Onestage anterior inter-body autografting and instrumentation in primary surgical management of thoraco-lumbar spinal tuberculosis. Eur Spine J 2004;13:114-21. [ Links ]
9. Moon MS, Woo YK, Lee KS, et al: Posterior instrumentation and anterior inter-body fusion for tuberculous kyphosis of dorsal and lumbar spines. Spine 1995;20:1910-16. [ Links ]
10. Cavusoglu H, Kaya RA, Turkmenoglu ON et al. A long-term follow-up study of anterior tibial allografting and instrumentation in the management of thoraco-lumbar tuberculous spondylitis. J Neurosurg Spine 2008;8:30-38. [ Links ]
11. Klockner CK, Valencia R. Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine 2003;28:1036-42. [ Links ]
12. Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969;7:179-92. [ Links ]
13. Govender S. Outcome of Allografts and Anterior Instrumentation. Clin Orthop and Rel Research 2002;398:60-66. [ Links ]
14. Khoo LT, Mikawa K, Fessler RG. A surgical revisitation of Pott distemper of the spine. Spine 2003;3:130-45. [ Links ]
15. Hibbs RA. An operation for Pott's disease of the spine. J Am Med Assoc 1911;59:433-36. [ Links ]
16. Albee FH. Transplantation of a portion of the tibia into the spine for Pott's disease. A preliminary report. J Am Med Assoc 1911;57:885-86. [ Links ]
17. Ito H, Asami T. A new radical operation for Pott's disease. Report of ten cases. J Bone Joint Surg 1934;15:499. [ Links ]
18. Hodgson AR, Stock FS. Anterior spinal fusion: a preliminary communication on the radical treatment of Pott's disease and Pott's paraplegia. Br J Surg 1956;44:266-75. [ Links ]
19. Moon MS. Development in the management of tuberculosis of the spine. Current Orthopaedics 2006;20:132-40. [ Links ]
20. Moon MS. Treatment of spinal infections. Commemorative issue. Third spinal section congress, WPOA J Western Pacific Orthop Assoc 1983;7-11. [ Links ]
21. Rajasekaran S, Shanmugasundaram TK. Prediction of the angle of gibbus deformity in tuberculosis of the spine. J Bone Joint Surg 1987;69-A:503-509. [ Links ]
22. Louw JA. Spinal tuberculosis with neurological deficit: Treatment with anterior vascularized rib grafts, posterior osteotomies and fusion. J Bone Joint Surg 1990;72-B:686-93. [ Links ]
23. Govender S, Parbhoo AH: Support of the anterior column with allografts in tuberculosis of the spine. J Bone Joint Surg 1999;81-B:106-109. [ Links ]
24. Verlaan JJ, Diekerhof CH, Buskens E et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: A systematic review of literature on techniques, complications and outcome. Spine 2004;29:803-14. [ Links ]
25. Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW. Long-term results of allograft replacement in the management of bone tumours. Clin Orthop 1996;324:86-97. [ Links ]
26. Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Spine 1993;18:1890-94. [ Links ]
27. Ha KY, Chung YG, Ryoo SJ. Adherence and biofilm formation of Staphylococcus epidermis and Mycobacterium tuberculosis on various spinal implants. Spine 2004;29(24):1-6. [ Links ]
 Reprint requests:
Reprint requests:
Prof RN Dunn
info@spinesurgery.co.za
No benefits of any form have been received from a commercial party related directly or indirectly to the subjectof this article.














