Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.10 no.3 Centurion ene. 2011
CLINICAL ARTICLE
Anatomical classification and surgical considerations: primary spinal tumours an overview
JH Davis
Consultant Orthopaedic and Spinal Surgeon. Department of Orthopaedic Surgery, Tygerberg Hospital, Stellenbosch
ABSTRACT
Primary spinal tumours make up 11% of primary musculoskeletal tumours, and 4.2% of spinal tumours.1 Six per cent of these spinal tumours are to be considered malignant.2 The intrinsic rarity of these tumours therefore make it very difficult for a single spinal surgeon to amass a large enough number of surgical cases to string together a valid and well-constructed series in a single career. The sparse body of available literature stems mostly from multi-centre research.
Inappropriate treatment and incomplete resection not only increase the rate of recurrence, but have in fact been shown to be detrimental to the patient's survival.3-5 Thorough understanding of the principles involved as well as experience therefore limits the treatment of such cases to bigger centres with high enough numbers to be considered practised.
Key words: Primary spinal tumour, Enneking, Weinstein-Boriani-Biagini, classification, vertebrectomy
The Enneking classification system
The Enneking classification system6 as popularised in the 1980s was initially envisaged as a staging system for oncological lesions of the appendicular skeleton, in specific long bones. It has been validated in the literature as predictive of prognosis, as well as in guiding surgical resection margins. The Enneking staging system rests on three tiers, the first being histological grading of the lesion (through microscopic evaluation of a tissue sample). Increasing evidence of anaplasia such as hyperchromasia, pleomorphism and numerous atypical mitoses designate a lesion as a higher grade lesion:
• G0 - Benign lesion
• G1 - Low grade malignant lesion
• G2 - High grade malignant lesion
The second tier rests on the containment of the tumour within the compartment of origin, with a tumour-site value assigned according to the local spread of the tumour.
This is typically evaluated through imaging modalities such as computer tomography (CT) and magnetic resonance imaging (MRI) to clearly define the extent of bony destruction as well as infiltration of the adjacent soft tissues and compartments. Histopathological analysis of gross specimens (following excision) further confirms suspected local extent of tumour spread and infiltration.
• T0 - Benign lesion; compartment confined
• T1 - Benign aggressive - / Malignant lesion; compartment confined
• T2 - Benign aggressive - / Malignant lesion; spread beyond compartment of origin
Lastly the lesion's tendency to metastasise is assigned as:
• M0 - No metastases
• M1 - Regional - / Distant metastases
Distant spread is shown with whole body radionuclide studies or additional imaging modalities. A technetium-99m (99mTc) bone scan can detect lesions as small as 2 mm and will pick up on 5-15% alteration in local bone turnover. Bone destruction in both osteolytic and osteoblastic lesions can be identified 2-18 months earlier than traditional plain film radiographs. Plasmacytoma may present the unique problem in that it may be purely lytic, and therefore not detected by an ordinary bone scan. In these cases 99mTc-sestamibi has been demonstrated as a very useful modality with a specificity of 96% and a sensitivity of 92%. MRI as an alternative can be considered the standard in today's terms.
Positron emission tomography (PET scan) with tracer fluorine-18 (F-18) fluorodeoxyglucose (FDG) is growing in prominence as a modality used in musculoskeletal oncology. This glucose analog tracer assimilated by glucose-using cells is phosphorylated by hexokinase (mitochondrial hexokinase is greatly increased in malignant cells with a rapid turnover). No further actions can occur in terms of aerobic metabolism within the cells, for the required oxygen on the tracer has been replaced by F-18. Most cells (with the exception of renal and hepatic cells) cannot remove the phosphate introduced by hexokinase because of the inherent ionic charge seen in phosphorylated sugars. This leads to accumulation and an intense radiolabelling of tissues with high glucose uptake, as is seen in most cancers.
Following staging, recommendations regarding surgical margins can be made as simply summarised in Table I. (Note: Arabic numerals are used for benign lesions and Roman numerals for malignant lesions.)
In 1997 Boriani et al applied the principles from Enneking's staging system in recommendations regarding primary spinal tumours.7 The presence of a pseudo capsule, skip lesions, extra-compartmental spread, metastases and lesion aggression determine staging of lesions specific to the spinal column.
The Enneking staging system in the spine
Benign lesions
Stage 1 (Benign latent lesion) (Figure 1)
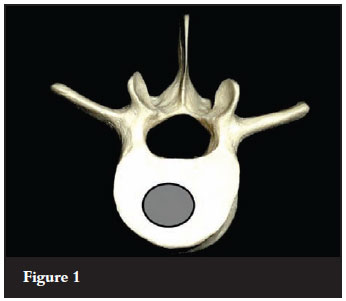
These lesions are usually asymptomatic and rarely require any form of treatment. The lesion in surrounded by a true containing capsule. A good example of a benign latent lesion will be a haemangioma - only requiring treatment if the lesion is causing pressure symptoms through neurological structure compression.
Stage 2 (Benign active lesion) (Figure 2)

These active lesions are slow growing with mild symptoms. There is a thin true capsule present still, with a thin zone of host-reactive tissue surrounding the lesion. Good examples of such lesions in the spine would be an osteoid osteoma or an aneurysmal bone cyst. These lesions lend themselves to intralesional excision, with a low recurrence rate.
Stage 3 (Benign aggressive lesion) (Figure 3)

Benign aggressive lesions display rapid growth, with a thin and incomplete capsule. There is prominent pseudo capsule established by a wide zone of host-reactive tissue. These lesions readily invade adjacent compartments. Intralesional curettage is not sufficient for these lesions and is associated with a high rate of recurrence. A wide marginal excision is indicated for such lesions.
Malignant lesions
Stage I (Low grade malignant lesion) (Figure 4)
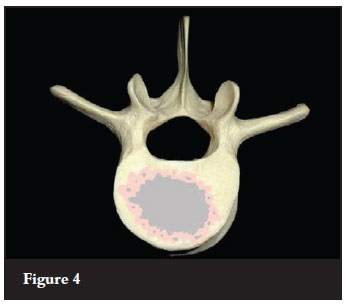
No true capsule is present in the case of these malignant lesions, with only a pseudo capsule of host-reactive tissue present. The pseudo capsule contains islands of tumour tissue. A wide en-bloc excision is indicated for a low grade malignant lesion.
Stage II (High grade malignant lesion) (Figure 5)

High grade malignant lesions display such rapid growth that the host tissue is not granted the opportunity to respond with a reactive tissue zone. These lesions therefore do not exhibit a pseudo capsule. Seeding with satellite tumour nodules and skip lesions are commonplace, with rapid tumour spread to adjacent compartments and the epidural space. Wide en-bloc resection is indicated as treatment modality.
Stage III (Metastatic lesions) (Figure 6)

These lesions are accompanied by spread of tumour to distant sites and organs, irrespective of histological grading. Treatment in Stage III lesions is largely palliative with dependence on adjuvants if perceptible and surgical management directed according to survival prognosis and direct symptoms such as neurological deficit.
Margins as dictated by the Enneking system is often very difficult to adhere to in the spinal column because of the close proximity of structures not so readily sacrificed in an en-bloc excision, for example the spinal cord, aorta and nerve roots. It is also important to consider the extent of the epidural space as a compartment extending from the cephalad to caudad ends of the spinal column. In this light the Weinstein-Boriani-Biagini (WBB) classification was described to aid with decision-making regarding feasible surgical margins in the spinal column.7
The Weinstein-Boriani-Biagini surgical staging system
The WBB surgical staging system describes the involvement of a specific vertebra in terms of sectors involved, arranged clockwise in 12 sectors on an axial vertebral face. The lesion is further confined to five layers of tissue penetration denoted as A-E (see Figure 7). Longitudinal extent is described in numbers of vertebrae involved.
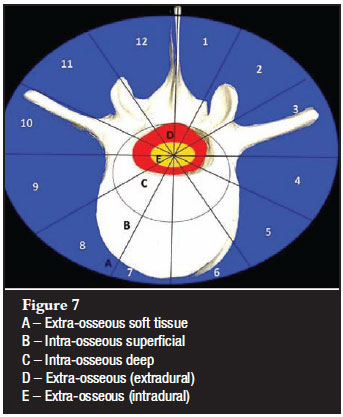
Recommendations can be made regarding the most appropriate approach and procedure to allow for en-bloc removal of a neoplastic lesion, based on the sectors and layers involved in the specific case, including surrounding structures (as denominated by the tissue layers) as required for en-bloc excision of the lesion with an appropriate clear margin.
Procedures
Three procedures are advocated: vertebrectomy, sagittal resection and posterior arch resection.
1. Vertebrectomy
A vertebrectomy (Figure 8) is indicated for lesions in zones 4-8, or 5-9 with at least one pedicle free of tumour. This allows for a combined posterior approach, with the posterior elements removed in a piece-meal fashion. The unaffected pedicle allows for resection on the posterior aspect of the vertebral body, with the subsequent establishment of haemostatic control, as well as freeing of the posterior longitudinal ligament. A second anterior approach is then utilised to remove the vertebral body containing the tumour in its entirety (en-bloc).

2. Sagittal resection
The sagittal resection (Figure 9) is indicated for unilateral lesions from zones 2-5 or 8-11, with the lesion possibly involving the pedicle or transverse process. Again through a combined approach the vertebral body will be split in a sagittal plane, allowing for a clear margin from the lesion. Subsequently a separate approach is used to remove the posterior elements of the unaffected side, allowing for the en-bloc removal of the lesion containing hemi-vertebra.

3. Posterior arch resection
The posterior arch resection (Figure 10) is indicated for lesions restricted to zones 10-3. The posterior elements are resected through a single posterior approach, with the pedicles sectioned adjacent to the vertebral body to allow the removal of the posterior arch en-bloc.

Validation of the Enneking and Weinstein-Boriani-Biagini classification systems
Moderate interobserver reliability and near perfect intraobserver reliability has been demonstrated for both the Enneking and the WBB classification systems. It has been recommended, however, that further research into the matter needs to be done prior to inclusion of these recommendations into mainstream practice.8 The Enneking progressive staging system has been shown to be predictive of prognosis in spinal tumours both in terms of recurrence of lesions and the associated mortality.9
References
1. Boriani S, Biagini R, De Lure F, et al. Primary bone tumours of the spine: A survey of the evaluation and treatment at the Instituto Orthopedico Rizzoli. Orthopedics 1995;18:993-1000. [ Links ]
2. Abdu WA, Provencher M. Primary bone and metastatic tumours of the cervical spine. Magn Reson Imaging Clin North Am 2000;4:299-320. [ Links ]
3. Boriani S, Biagini R, De Lure F. En bloc resections of bone tumours of the thoraco-lumbar spine. A preliminary report on 29 patients. Spine 1996;21:1927-31. [ Links ]
4. Bergh P, Gutenberg B, Meis-Kindblom LG. Prognostic factors and outcome of pelvic, sacral, and spinal chondrosarcomas: A centerbased study of 69 cases. Cancer 2001;91:1201-12. [ Links ]
5. Talac R, Yaszemski MJ, Currier BL, Fuchs B, Dekutoski MB, Kim CW, Sim FH. Relationship between surgical margins and local recurrence of sarcomas of the spine. Clin Orthop Rel Res 2002;397:127-32. [ Links ]
6. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res 1980;106-20. [ Links ]
7. Boriani S, Weinstein JN, Biagini R. Primary bone tumours of the spine. Terminology and surgical staging. Spine 1997 (May);22:1036-44. [ Links ]
8. Chan P, Boriani S, Fourney DR, Biagini R, Dekutoski MB, Fehlings MG, Ryken TC, Gokaslan ZL, Vrionis FD, Harrop JS, Schmidt MH, Vialle LR, Gerszten PC, Rhines LD,Ondra SL, Pratt SR, Fisher CG. An assessment of the reliability of the Enneking and Weinstein-Boriani-Biagini classifications for staging of primary spinal tumours by the Spine Oncology Study Group. Spine 2009 (Feb);34:384-91. [ Links ]
9. Fisher CG, et al. Surgical management of primary bone tumours of the spine: Validation of an approach to enhance cure and reduce local recurrence. Spine 2011 (May);36:830-36. [ Links ]
10. Sundaresan N, Boriani S, Rothman A, Holtzman R. Tumours of the spine. J Neurooncology 2004;69:273-90. [ Links ]
11. Fuchs B, Boos N. Primary tumours of the spine. [ed] Max Aebi Norbert Boos. Heidelberg: Springer-Verlag, 2008. pp.951-76. [ Links ]
 Reprint requests:
Reprint requests:
johanhdavis@yahoo.com
No benefits of any form have been received from a commercial party related directly or indirectly to the subject of this article.














