Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.10 no.2 Centurion ene. 2011
ARTICLE
Cryptococcoma of the ilium in an immuno-competent child - a case report and review of the literature
DT McGuireI; SM BickI; T Westgarth-TaylorII; E HoffmanIII
IMBChB. Registrar, Department of Orthopaedic Surgery, Red Cross Children's Hospital and Groote Schuur Hospital, Cape Town
IIMBChB. Registrar, Department of Radiology, Red Cross Children's Hospital and Groote Schuur Hospital, Cape Town
IIIMBChB, FCS(SA)Ortho. Associate Professor, Department of Orthopaedic Surgery, Red Cross Children's Hospital and Maitland Cottage Paediatric Orthopaedic Hospital, Cape Town
ABSTRACT
Cryptococcosis is a systemic disease caused by the fungus Cryptococcus neoformans which predominantly affects immuno-compromised individuals. Cryptococcal osteomyelitis is rare, having an incidence of 5-10% in patients with systemic cryptococcosis. Isolated cryptococcoma of bone is even less common, especially in immuno-competent individuals.
We report a case of a 10-year-old girl who presented with a mass over her left iliac crest. Radiographs showed a lytic lesion of the ilium. Open biopsy and surgical curettage of the lesion was done.
Histology showed a cryptococcoma. The patient was treated with fluconazole. After three months of treatment she required a repeat curettage of the lesion due to wound drainage and persistent soft tissue swelling. She continued with oral fluconazole treatment and after 7 months the wound had healed, the soft tissue swelling had resolved and radiographs showed resolution of the lesion.
Fungal infections should be included in the differential diagnosis of lytic bone lesions. Tissue diagnosis should be obtained to confirm diagnosis. Fluconazole is an effective treatment for cryptococcal osteomyelitis, with surgical curettage a useful adjunct. Good results can be expected in the majority of cases.
Key words: cryptococcosis, fungus, Aids, bone involvement
Introduction
Cryptococcosis is a disseminated mycosis caused by Cryptococcus neoformans which is a yeast-like encapsulated fungus.1 The most commonly affected organs are the lungs (pneumonia) and central nervous system (meningitis).2 Most patients infected with systemic cryptococcosis are immuno-compromised. It is the second most common fungal infection in Aids patients.3 Cryptococcus neoformans is commonly found in soil and pigeon faeces.
Isolated cryptococcal osteomyelitis is rare.2-4 Bone involvement in patients with systemic disease has an incidence of 5-10%.1,2,4,5 We report a case here of an isolated cryptococcoma of the ilium of an immuno-competent 10-year-old girl.
Case report
A 10-year-old girl was referred from a secondary level hospital to our oncology department with an abdominal mass in the left iliac fossa. Radiographs revealed a lytic lesion of the iliac bone and she was referred to the orthopaedic unit. Clinically she had a left iliac crest mass measuring 5 cm × 5 cm, involving the anterior half of the iliac crest. It extended into the left iliac fossa and under the gluteal muscles. It was smooth and firm in consistency, and was mildly tender only on deep palpation. The overlying skin was normal, and there were no signs of local infection. General examination of the child was unremarkable.
The mass had been present for approximately 6 months. It was slowly enlarging, and there was minimal associated pain. The child had no history of systemic illnesses and had no constitutional symptoms. She had recently moved to our country with her family from a neighbouring country where they had lived on a maize farm.
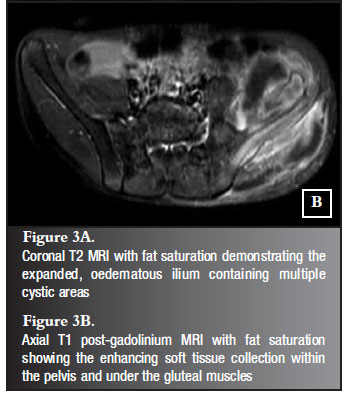
Pelvic radiographs revealed a large, lytic, expansile lesion of the left ilium with scalloping of the iliac bone and subperiosteal new bone formation and a soft tissue mass outside the ilium. The appearance was that of a benign bone tumour, most likely an aneurysmal bone cyst (Figure 1). Chest radiograph was normal. The full blood count was normal. The ESR was elevated to 99 mm. The HIV test was negative and the Mantoux test was non-reactive.
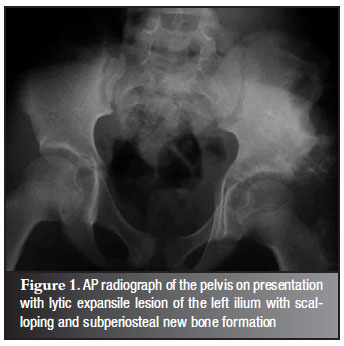
Radionuclide bone scan showed increased blood pool activity in the left iliac bone. On the delayed images the uptake in the bone was irregular, with markedly increased uptake and distorted bony margins (Figure 2).
CT scan was not done.
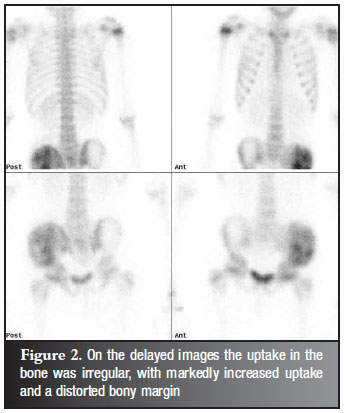
MRI showed an expanded oedematous ilium with multiple cystic areas and a scalloped appearance of the bone. There was a soft tissue mass extending into the pelvis and gluteal muscles which showed inhomogenous enhancement after gadolinium contrast with fat saturation (Figure 3A and B). Although there were no fluid levels the pre-operative differential diagnosis was aneurysmal bone cyst, eosinophilic granuloma and telangiectatic osteosarcoma.
Open biopsy of the iliac crest was performed via a utilitarian approach. The apophysis was split and a subperiosteal approach of the inner and outer table of the ilium was done. The lesion consisted of a gelatinous, light brown substance. The iliac bone was expanded into well circumscribed, scalloped areas. The cortex was centrally eroded and the lesion extended through this hole from underneath gluteus medius to underneath iliopsoas. As much of the lesion as possible was removed by curettage. Samples were sent for frozen section histology, general microscopy, culture and sensitivity (MC & S), fungal MC & S, as well as for tuberculosis MC & S.
The frozen section showed features of cryptococcal infection. Paraffin section was performed which confirmed the diagnosis of a cryptococcoma. There were associated giant cells, neutrophils, macrophages and plasma cells seen. PAS stain showed both encapsulated as well as acapsulate forms of Cryptococcus neoformans.
The patient was treated with oral fluconazole (200 mg per day). The wound healed postoperatively, but at six-week follow-up there was serous fluid oozing from the wound with mild inflammation of the surrounding skin. The patient was put on a two week course of flucloxacillin. The inflammation improved and the oozing stopped.
At three-month follow-up there was again wound oozing with surrounding inflammation. Some soft tissue swelling was still present. The patient then had a repeat curettage. At the time of surgery it was noted that most of the gelatinous material found at the first curettage had not recurred. There was, however a small amount of gelatinous material found in a part of the ilium that had been missed at the first surgery. This was the source of the ooze and it was removed by curettage.
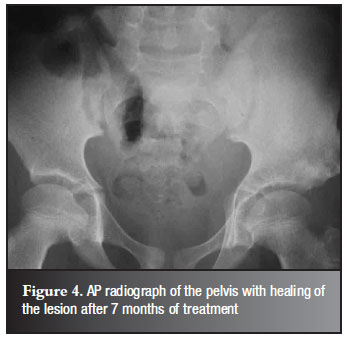
Fluconazole was continued and at seven-month follow-up the soft tissue swelling had resolved and the wound had healed. Radiographs confirmed resolution of the lesion (Figure 4) Fluconazole treatment was stopped.
Discussion
Infections occur through inhalation of yeast-like organisms which enter smaller respiratory passages and then remain dormant depending on the host reaction.6 The pigeon appears to be the chief vector for the distribution and maintenance of Cryptococcus neoformans. The organism is usually found in debris in pigeon roosts or other bird nests.7 Direct inoculation through the skin may also occur.5
There are two types of Cryptococcus neoformans infections, but the manifestation depends on the host response rather than the strain of the organism,8 with infection rarely occurring in immuno-competent hosts.9 The first type occurs in immuno-compromised individuals where the infection spreads rapidly to involve most organ systems, especially the central nervous system (CNS). The second occurs in immuno-competent individuals where the body's natural defence mechanism prevents systemic disease. In these cases organisms can be disseminated haematogenously to distal sites, where re-activation can occur at a later stage and give rise to localised disease.8 The overall incidence of crytococcosis in immuno-competent individuals has been estimated at 0.2 per million per year.10
Cryptococcal skeletal infection was first reviewed in the literature by Collins in 1950.11 He reported skeletal involvement in 10% of patients with systemic cyptococcal disease, but noted that as an isolated entity it was rare. This has been confirmed subsequently by several authors.1-4,12 A literature review of 31 years by Al-Tawfiq in 2007 found 47 published cases of isolated cryptococcal osteomyeltits.13 Thirty-four per cent of these patients had no other underlying systemic illness. The rest had sarcoidosis (19%), tuberculosis (6.4%), diabetes mellitus (8.5%) or other systemic illnesses. The most common site of skeletal involvement is the vertebral body, although no bone is spared.1,2,5,14
The majority of patients with skeletal cryptococcal infections presents with swelling and tenderness.1 Pyrexia is seldom present, and haematological investigations are usually unremarkable with the exception of the ESR which can be mildly raised.5
Typical radiographic appearance is non-specific and is usually that of a lytic lesion with minimal or no periosteal reaction.1 There may be erosion of cortical and cancellous bone with sharply defined sclerotic margins which may be scalloped.4 The differential diagnosis of a lytic bone lesion should include neoplasms, tuberculosis and other bacterial and fungal infections.1,12 Cryptococcomas of bone have been mistaken for Ewing or osteosarcoma, tuberculosis, and avascular necrosis.1,3,15-18
Diagnosis should be confirmed with tissue samples, due to the non-specificity of the appearance of cryptococcomas, as well as its similarity to tuberculosis, especially when it involves the vertebral body.16 Biopsy can be performed by percutaneous fine needle aspiration, or at the time of surgery by incision and drainage or curettage.5 Sixty-six per cent of HIV-negative patients with cryptococcal disease have a positive serum cryptococcal antigen test.19
Before the advent of antifungal therapy with amphotericin B in 1956, there were reports of spontaneous resolution as well as progression to death due to cryptococcosis.11 Since then effective systemic treatment has reduced morbidity and mortality dramatically. Previously, no definite consensus was reached regarding whether systemic drug therapy alone or surgical curettage combined with drug therapy was the treatment of choice for cryptococcal osteomyelitis.12 There are many reports in the literature of patients being cured by either medical or surgical treatment alone, or a combination of the two.2,5,16 According to recommendations made in 2000 by the Infectious Disease Society of America (IDSA), surgery should be reserved for patients with persistent or refractory bone disease, but is rarely needed.12 The goals of surgery are to lessen the infectious burden, prevent a delay in diagnosis and prevent the contiguous spread of infection.20 Systemic treatment previously consisted of combination therapy of amphotericin B and 5-flucytosine. This combination therapy can be highly nephro- and hepatotoxic, and can result in bone marrow suppression. Treatment with fluconazole has been shown to be effective and is much less toxic, and has become the pharmacological agent of choice.6 The most recent guidelines from IDSA indicate that the treatment of choice in immuno-competent patients with non-CNS disease is oral fluconazole 200-400 mg daily for 6-12 months.21
The outcome in HIV-negative patients with cryptococcal osteomyelitis is usually favourable.13 Of the 41 patients in the study by Al-Tawfiq with reported outcomes, 37 (90.2%) had been cured and the other four (9.8%) patients had died. The deaths were attributed to liver failure in one patient and to pneumonia in another patient. The other two causes of death were unclear.
Conclusion
Cryptococcal osteomyelitis is a rare condition in immuno-competent individuals, but fungal infections should always be considered in the differential diagnosis of a lytic bone lesion. Tissue obtained at biopsy of a suspected tumour should always be sent for routine histology, as well as general, fungal and tuberculosis MC & S. Fluconazole is an effective treatment for cryptococcal osteomyelitis, with surgical curettage a useful adjunct. Good results can be expected in the majority of cases.
References
1. Goldshteyn N, Zanchi A, Cooke K, et al. Cryptococcal osteomyelitis of the humeral head initially diagnosed as avascular necrosis. South Medical Journal 2006; 99(10):1140-41. [ Links ]
2. YukFong Liu P. Cryptococcosis osteomyelitis: A case report and review. Diagn Microbiol Infec Diseases 1998;30:33-35. [ Links ]
3. Fialk MA, Marcove RC, Armstrong D. Cryptococcal bone disease: a manifestation of disseminated cryptococcosis. Clin Orthop 1981;158:219-23. [ Links ]
4. Noh HM, Kuszyk BS, Fishman EK. Cryptococcoma of the sacrum. Skeletal Radiol 1999;28:49-51. [ Links ]
5. Behrman RE, Masci JR, Nicholas P. Cryptococcal skeletal infections: case report and review. Reviews Infect Dis 1990;12(2):181-90. [ Links ]
6. Subramanian S, Mathai D. Clinical manifestations and management of cryptococcal infection. J Postgrad Med 2005;51(1):s21-s26. [ Links ]
7. Kumlin U, Olsen B, Granlund M, et al. Cryptococcosis and starling nests. Lancet 1998; 351:1181. [ Links ]
8. Govender S, Ganpath V, Charles R, et al. Localized osseous cryptococcal infection. Acta Orthop Scand 1988; 59(6):720-22. [ Links ]
9. Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. J Infect Dis 1991; 13: 1163-69. [ Links ]
10. Freidman GD. The rarity of cryptococcosis in Northern California: the 10 year experience of a large defined population. Am J Epidemiol 1983; 117: 230-34. [ Links ]
11. Collins VP. Bone involvement in cryptococcosis (torulosis). Am Jour Roentgenol 1950; 63:102-12. [ Links ]
12. Chleboun J, Nade S. Skeletal cryptococcosis. J Bone Joint Surg(Am) 1977; 59- A: 509-14. [ Links ]
13. Al-Tawfiq JA, Ghandour J. Cryptococcus neoformans abscess and osteomyelitis in an immuno-competent patient with tuberculous lymphadenitis. Infection 2007;35(5):377-82. [ Links ]
14. Lie KW, Yu YL, Cheng IKP, et al. Cryptococcal infection of the lumbar spine. Jour Royal Soc Med 1989;82(2):172-73. [ Links ]
15. Zach TL, Penn RG. Localised cryptococcal osteomyelitis in an immuno-competent host. Pediatr Infect Dis 1986;5:601-603. [ Links ]
16. Govender S, Mutasa E, Parbhoo AH. Cryptococcal osteomyelitis of the spine. J Bone Joint Surg(Br) 1999; 81-B(3):459-61. [ Links ]
17. Witte DA, Chen I, Brady J, et al. Cryptococcal osteomyelitis. Report of a case with aspiration biopsy of a humeral lesion with radiological features of malignancy. Acta Cytol 2000;44:815-18. [ Links ]
18. Gupta SK, Chabra R, Sharma BS, et al. Vertebral cryptococcosis simulating tuberculosis. Brit J of Neurosurg 2003; 17(6):556-71. [ Links ]
19. Kiertiburanakul S, Wirojtananugoon S, Pracharktam R, et al. Cryptococcosis in human immunodeficiency virus-negative patients. Int J Infect Dis 2006; 10:72-78. [ Links ]
20. Raftopoulos I, Meller JL, Harris V, et al. Cryptococcal rib osteomyelitis in a pediatric patient. J Pediatr Surg 1998;33(5):771-73. [ Links ]
21. Saag MS, Graybill RJ, Larsen RA, et al. Practice guidelines for the management of cryptococcal disease. Infectious Diseases Society of America. Clin Infect Dis 2000;30:710-18. [ Links ]
 Reprint requests:
Reprint requests:
Dr DT McGuire
Department of Orthopaedic Surgery Medical school, University of Cape Town
Anzio Road
Observatory
7925 Cape Town
Tel: (021) 404-5108 Fax: (021) 472-7093
Email: duncan.mcguire@gmail.com
No benefits of any form have been received from a commercial party related directly or indirectly to the subjectof this article. The content of this article is the sole work of the authors.